Abstract
Aim
Proper and adequate documentation in operation notes is a basic tool of clinical practice with medical and legal implications. An audit was done to ascertain if oral and maxillofacial surgery operative notes in an Indian public sector hospital adhered to the guidelines published by the Royal College of Surgeons England.
Methods
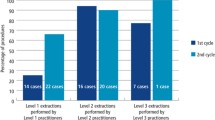
Fifty randomly selected operative notes were evaluated against the guidelines by RCS England with regards to the essential generic components of an operation note. Additional criteria relevant to oral and Maxillofacial Surgery were also evaluated. Changes were introduced in the form of Oral and Maxillofacial Surgery specific consent forms, diagram sheets and a computerized operation note proforma containing all essential and additional criteria along with prefilled template of operative findings. Re-audit of 50 randomly selected operation notes was performed after a 6 month period.
Results
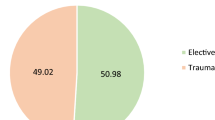
In the 1st audit cycle, excellent documentation ranging from 94 to 100 % was seen in 9 essential criteria. Unsatisfactory documentation was observed in criteria like assistant name, date of surgery. Most consent forms contained abbreviations and some did not provide all details. Additional criteria specific to Oral and Maxillofacial Surgery scored poorly. In the 2nd Audit for loop completion, excellent documentation was seen in almost all essential and additional criteria. Mean percentage of data point inclusion improved from 84.6 to 98.4 % (0.001< P value <0.005). The use of abbreviations was seen in only 6 notes.
Conclusion
Regular audits are now considered a mandatory quality improvement process that seeks to improve patient care and outcomes. To the best of our knowledge, this is the first completed audit on operation notes documentation in Oral and Maxillofacial Surgery from India. The introduction of a computerized operation note proforma showed excellent improvement in operation note documentation. Surgeons can follow the RCS guidelines to ensure standardization of operation notes.


Similar content being viewed by others
References
Shayah A, Agada FO, Gunasekaran S, Jassar P, England RJA (2007) The quality of operative note taking: an audit using the Royal College of Surgeons guidelines as the gold standard. Int J Clin Pract 61:677–679
The Royal College of Surgeons of England (2008) Good surgical practice. The Royal College of Surgeons of England, London
Payne K, Jones K, Dickenson A (2011) Improving the standard of operative notes within an oral and maxillofacial surgery department, using an operative note proforma. J Maxillofac Surg 10(3):203–208
Sinclair A (2008) How to set up a prospective surgical audit. In: Wilcox DT, Godbole PP, Koyle M (eds) Pediatric urology: surgical complications and management. Blackwell Publishing, Oxford, p 3–7
Borchert D, Rarshen H, Kemps M, Lavelle M (2006) Operative notes teaching: re-discovery of an effective teaching tool in surgical training. Int J Surg 8(1):1–11
Al-Hussainy H, Ali F, Jones S, McGregor-Riley J, Sukumar S (2005) Improving the standard of operation notes in orthopaedic and trauma surgery: the value of a proforma. Injury 35:1102–1106
Lefter LP, Walker SR, Dewhurst F, Turner RWL (2008) An audit of operation notes: facts and ways to improve. ANZ J Surg 78:800–807
Rogers A, Banting M, Atherstone A (2008) The quality of operative notes at a general surgery unit. S Afr Med J 98(9):726–728
Din R, Jena D, Muddu BW (2001) The use of an aide-memoire to improve the quality of operation notes in an orthopaedic unit. Ann R Coll Surg Engl 83(5):319–320
The Royal College of Surgeons of England (2014) Good surgical practice. The Royal College of Surgeons of England, London
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None.
Rights and permissions
About this article
Cite this article
Krishnan, B., Prasad, G.A. & Madhan, B. Improving the Quality of Oral and Maxillofacial Surgical Notes in an Indian Public Sector Hospital in Accordance with the Royal College of Surgeons Guidelines: A Completed Audit Loop Study. J. Maxillofac. Oral Surg. 15, 315–320 (2016). https://doi.org/10.1007/s12663-015-0850-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12663-015-0850-x