Abstract
Purpose
There is significant variability in intraoperative red blood cell (RBC) transfusion practice. We aimed to use the theoretical domains framework (TDF) to categorize nonclinical and behavioural factors driving intraoperative RBC transfusion practice in a systematic review of the literature.
Source
We searched electronic databases from inception until August 2021 to identify studies evaluating nonclinical factors affecting intraoperative RBC transfusion. Using the Mixed Methods Appraisal Tool, we assessed the quality of included studies and identified relevant nonclinical factors, which were coded into TDF domains by two independent reviewers using NVivo (Lumivero, QSR International, Burlington, MA, USA). We identified common themes within domains and sorted domains based on the frequency of reported factors.
Principal findings
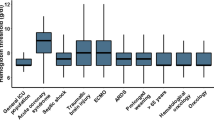
Our systematic review identified 18 studies: nine retrospective cohort studies, six cross-sectional surveys, and three before-and-after studies. Factors related to the social influences, behavioural regulation, environmental context/resources, and beliefs about consequences domains of the TDF were the most reported factors. Key factors underlying the observed variability in transfusion practice included the social effects of peers, patients, and institutional culture on decision-making (social influences), and characteristics of the practice environment including case volume, geographic location, and case start time (environmental context/resources). Studies reported variable beliefs about the consequences of both intraoperative transfusion and anemia (beliefs about consequences). Provider- and institutional-level audits, educational sessions, and increased communication between surgeons/anesthesiologists were identified as strategies to optimize intraoperative transfusion decision-making (behavioural regulation).
Conclusion
Our systematic review has synthesized the literature on nonclinical and behavioural factors impacting intraoperative transfusion decision-making, categorized using the TDF. These findings can inform evidence-based interventions to reduce intraoperative RBC transfusion variability.
Study registration
Open Science Framework (https://osf.io/pm8zs/?view_only=166299ed28964804b9360c429b1218c1; first posted, 3 August 2022)
Résumé
Objectif
Il existe une variabilité importante dans les pratiques de transfusion peropératoire de culots sanguins. Nous avons cherché à utiliser le cadre des domaines théoriques (TDF, pour theoretical domains framework) pour catégoriser les facteurs non cliniques et comportementaux motivant les pratiques de transfusion peropératoire de culots sanguins dans une revue systématique de la littérature.
Sources
Nous avons réalisé des recherches dans les bases de données électroniques de leur création jusqu’en août 2021 pour identifier les études évaluant les facteurs non cliniques affectant la transfusion peropératoire de culots sanguins. À l’aide de l’outil d’évaluation des méthodes mixtes, nous avons évalué la qualité des études incluses et identifié les facteurs non cliniques pertinents, qui ont été codés dans les domaines TDF par deux personnes les révisant de manière indépendante utilisant NVivo (Lumivero, QSR International, Burlington, MA, États-Unis). Nous avons identifié des thèmes communs au sein des domaines et trié les domaines en fonction de la fréquence des facteurs signalés.
Constatations principales
Notre revue systématique a identifié 18 études : neuf études de cohorte rétrospectives, six sondages transversaux et trois études avant-après. Les facteurs liés aux influences sociales, à la régulation comportementale, au contexte et aux ressources environnementaux et les croyances concernant les domaines de conséquences du TDF étaient les facteurs les plus rapportés. Les principaux facteurs sous-jacents à la variabilité observée dans la pratique transfusionnelle comprenaient les effets sociaux des pairs, de la patientèle et de la culture de l’établissement sur la prise de décision (influences sociales) et les caractéristiques de l’environnement de pratique, y compris le volume de cas, l’emplacement géographique et l’heure de début des cas (contexte/ressources environnementaux). Des études ont fait état de croyances variables sur les conséquences de la transfusion peropératoire et de l’anémie (croyances sur les conséquences). Des vérifications au niveau des prestataires et des établissements, des séances de formation et une communication accrue entre les chirurgien·nes et les anesthésiologistes ont été identifiées comme des stratégies pouvant optimiser la prise de décision transfusionnelle peropératoire (régulation comportementale).
Conclusion
Notre revue systématique a synthétisé la littérature sur les facteurs non cliniques et comportementaux ayant une incidence sur la prise de décision transfusionnelle peropératoire, classés à l’aide du TDF. Ces résultats peuvent éclairer les interventions fondées sur des données probantes pour réduire la variabilité de transfusion peropératoire de culots sanguins.
Enregistrement de l’étude
Open Science Framework (https://osf.io/pm8zs/?view_only=166299ed28964804b9360c429b1218c1; soumis pour la première fois, 3 août 2022)


Similar content being viewed by others
Notes
Available from URL: https://osf.io/pm8zs/?view_only=166299ed28964804b9360c429b1218c1 (accessed January 2024).
References
Ackland GL, Brudney CS, Cecconi M, et al. Perioperative Quality Initiative consensus statement on the physiology of arterial blood pressure control in perioperative medicine. Br J Anaesth 2019; 122: 542–51. https://doi.org/10.1016/j.bja.2019.01.011
Qian F, Osler TM, Eaton MP, et al. Variation of blood transfusion in patients undergoing major noncardiac surgery. Ann Surg 2013; 257: 266–78. https://doi.org/10.1097/SLA.0b013e31825ffc37
Chen A, Trivedi AN, Jiang L, Vezeridis M, Henderson WG, Wu WC. Hospital blood transfusion patterns during major noncardiac surgery and surgical mortality. Medicine (Baltimore) 2015; 94: e1342. https://doi.org/10.1097/MD.0000000000001342
Ejaz A, Spolverato G, Kim Y, Frank SM, Pawlik TM. Variation in triggers and use of perioperative blood transfusion in major gastrointestinal surgery. Br J Surg 2014; 101: 1424–33. https://doi.org/10.1002/bjs.9617
Bennett-Guerrero E, Zhao Y, O’Brien SM, et al. Variation in use of blood transfusion in coronary artery bypass graft surgery. JAMA 2010; 304: 1568–75. https://doi.org/10.1001/jama.2010.1406
Wennberg JE. Unwarranted variations in healthcare delivery: implications for academic medical centres. BMJ 2022; 325: 961–4. https://doi.org/10.1136/bmj.325.7370.961
Partington A, Chew DP, Ben-Tovim D, Horsfall M, Hakendorf P, Karnon J. Screening for important unwarranted variation in clinical practice: a triple-test of processes of care, costs and patient outcomes. Aust Health Rev 2017; 41: 104–10. https://doi.org/10.1071/AH15101
Harrison R, Manias E, Mears S, Heslop D, Hinchcliff R, Hay L. Addressing unwarranted clinical variation: a rapid review of current evidence. J Eval Clin Pract 2019; 25: 53–65. https://doi.org/10.1111/jep.12930
Zuckerman J, Coburn N, Callum J, et al. The contribution of surgeon and hospital variation in transfusion practice to outcomes for patients undergoing gastrointestinal cancer surgery: a population-based analysis. The Society for Surgery of the Alimentary Tract. 2021;
Lenet T, Baker L, Park L, et al. A systematic review and meta-analysis of randomized controlled trials comparing intraoperative red blood cell transfusion strategies. Ann Surg 2022; 275: 456–66. https://doi.org/10.1097/SLA.0000000000004931
Atkins L, Francis J, Islam R, et al. A guide to using the theoretical domains framework of behaviour change to investigate implementation problems. Implement Sci 2017; 12: 77. https://doi.org/10.1186/s13012-017-0605-9
Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med 2009; 6: e1000100. https://doi.org/10.1371/journal.pmed.1000100
Pluye P, Hong QN. Combining the power of stories and the power of numbers: mixed methods research and mixed studies reviews. Ann Rev Public Health 2014; 35: 29–45. https://doi.org/10.1146/annurev-publhealth-032013-182440
Addis DR, Moore BA, Garner CR, Fernando RJ, Kim SM, Russell GB. Case start time affects intraoperative transfusion rates in adult cardiac surgery: a single-center retrospective analysis. J Cardiothorac Vasc Anesth 2020; 34: 632–9. https://doi.org/10.1053/j.jvca.2019.10.044
Cote C, MacLeod JB, Yip AM, et al. Variation in transfusion rates within a single institution: exploring the effect of differing practice patterns on the likelihood of blood product transfusion in patients undergoing cardiac surgery. J Thorac Cardiovasc Surg 2015; 149: 297–302. https://doi.org/10.1016/j.jtcvs.2014.09.004
Goodnough LT, Johnston MF, Toy PT. The variability of transfusion practice in coronary artery bypass surgery. Transfusion Medicine Academic Award Group. JAMA 1991; 265: 86–90.
Jin R, Zelinka ES, McDonald J, et al. Effect of hospital culture on blood transfusion in cardiac procedures. Ann Thorac Surg 2013; 95: 1269–74. https://doi.org/10.1016/j.athoracsur.2012.08.008
Maddux FW, Dickinson TA, Rilla D, et al. Institutional variability of intraoperative red blood cell utilization in coronary artery bypass graft surgery. Am J Med Qual 2009; 24: 403–11. https://doi.org/10.1177/1062860609339384
McQuilten ZK, Andrianopoulos N, Wood EM, et al. Transfusion practice varies widely in cardiac surgery: results from a national registry. J Thorac Cardiovasc Surg 2014; 147: 1684–90. https://doi.org/10.1016/j.jtcvs.2013.10.051
Bennett S, Ayoub A, Tran A, et al. Current practices in perioperative blood management for patients undergoing liver resection: a survey of surgeons and anesthesiologists. Transfusion 2018; 58: 781–7. https://doi.org/10.1111/trf.14465
Camaj A, Zahuranec DB, Paone G, et al. Organizational contributors to the variation in red blood cell transfusion practices in cardiac surgery: survey results from the state of Michigan. Anesth Analg 2017; 125: 975–80. https://doi.org/10.1213/ANE.0000000000002277
Matot I, Einav S, Goodman S, Zeldin A, Weissman C, Elchalal U. A survey of physicians’ attitudes toward blood transfusion in patients undergoing Cesarean section. Am J Obstet Gynecol 2004; 190: 462–7. https://doi.org/10.1016/j.ajog.2003.07.028
Salem-Schatz SR, Avorn J, Soumerai SB. Influence of clinical knowledge, organizational context, and practice style on transfusion decision making. Implications for practice change strategies. JAMA 1990; 264: 476–83.
Salem-Schatz SR, Avorn J, Soumerai SB. Influence of knowledge and attitudes on the quality of physicians’ transfusion practice. Med Care 1993; 31: 868–78. https://doi.org/10.1097/00005650-199310000-00002
Shehata N, Wilson K, Mazer CD, et al. The proportion of variation in perioperative transfusion decisions in Canada attributable to the hospital. Can J Anesth 2007; 54: 902–7. https://doi.org/10.1007/BF03026794
Hensley NB, Cho BC, Visagie M, Lester LC, Abernathy JH 3rd, Frank SM. How do I audit intraoperative blood component utilization in cardiac surgery? Transfusion 2019; 59: 3058–64. https://doi.org/10.1111/trf.15399
Fischer DP, Zacharowski KD, Müller MM, et al. Patient blood management implementation strategies and their effect on physicians’ risk perception, clinical knowledge and perioperative practice—the Frankfurt experience. Transfus Med Hemother 2015; 42: 91–7. https://doi.org/10.1159/000380868
Rodrigues E. Improving communication for a better transfusion practice. Transfusion 2015; 55: 203A.
Brown ML, Parker SE, Quiñonez LG, Li Z, Sundt TM. Can the impact of change of surgical teams in cardiovascular surgery be measured by operative mortality or morbidity? A propensity adjusted cohort comparison. Ann Surg 2011; 253: 385–92. https://doi.org/10.1097/SLA.0b013e3182061c69
Smith CD, Korenstein D. Harnessing the power of peer pressure to reduce health care waste and improve clinical outcomes. Mayo Clin Proc 2015; 90: 311–2. https://doi.org/10.1016/j.mayocp.2015.01.011
Haessler S, Bhagavan A, Kleppel R, Hinchey K, Visintainer P. Getting doctors to clean their hands: lead the followers. BMJ Qual Saf 2012; 21: 499–502. https://doi.org/10.1136/bmjqs-2011-000396
Wu KH, Cheng FJ, Li CJ, Cheng HH, Lee WH, Lee CW. Evaluation of the effectiveness of peer pressure to change disposition decisions and patient throughput by emergency physician. Am J Emerg Med 2013; 31: 535–9. https://doi.org/10.1016/j.ajem.2012.10.012
Detsky AS, Verma AA. A new model for medical education: celebrating restraint. JAMA 2012; 308: 1329–30. https://doi.org/10.1001/2012.jama.11869
Hibbs SP, Brunskill SJ, Donald GC, Saunders HD, Murphy MF. Setting priorities for research in blood donation and transfusion: outcome of the James Lind Alliance priority-setting partnership. Transfusion 2019; 59: 574–81. https://doi.org/10.1111/trf.15077
Braester A, Shaoul E, Mizrachi O, Akria L, Shelev L, Barhoum. Patient involvement in the transfusion decision-making can change patient blood management practice for better or worse. Acta Haematol 2022; 145: 5–8. https://doi.org/10.1159/000518947
Carson JL, Guyatt G, Heddle NM, et al. Clinical practice guidelines from the AABB: red blood cell transfusion thresholds and storage. JAMA 2016; 316: 2025–35. https://doi.org/10.1001/jama.2016.9185
Mueller MM, Van Remoortel H, Meybohm P, et al. Patient blood management: recommendations from the 2018 Frankfurt Consensus Conference. JAMA 2019; 321: 983–97. https://doi.org/10.1001/jama.2019.0554
Baker L, Park L, Gilbert R, et al. Intraoperative red blood cell transfusion decision-making: a systematic review of guidelines. Ann Surg 2021; 274: 86–96. https://doi.org/10.1097/SLA.0000000000004710
Goodnough LT. Targeting continuing medical education on decision makers: who decides to transfuse blood? J Contin Educ Health Prof 1992; 12: 163–9. https://doi.org/10.1002/chp.4750120308
Shehata N, Burns LA, Nathan H, et al. A randomized controlled pilot study of adherence to transfusion strategies in cardiac surgery. Transfusion 2012; 52: 91–9. https://doi.org/10.1111/j.1537-2995.2011.03236.x
Author contributions
Tori Lenet contributed to all aspects of this manuscript, including conception and design; acquisition, analysis, and interpretation of data; and drafting the article. Pauline Berthelot contributed to study conception, protocol writing, design, and data acquisition. Alexa Grudzinski, Alexander Banks, and Joseph Tropiano contributed to data analysis and manuscript editing. Daniel McIsaac, Alan Tinmouth, and Dean Fergusson contributed to the conception and editing of the manuscript. Andrea Patey provided content expertise and contributed to data interpretation and editing of the manuscript. Guillaume Martel contributed to study conception, data interpretation, and editing of the manuscript.
Acknowledgements
We would like to acknowledge Risa Shorr for the development of the search strategy.
Disclosures
The authors do not declare any conflicts of interest.
Funding statement
This review was not supported by any financial support.
Editorial responsibility
This submission was handled by Dr. Stephan K. W. Schwarz, Editor-in-Chief, Canadian Journal of Anesthesia/Journal canadien d’anesthésie.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is accompanied by an Editorial. Please see Can J Anesth 2024; https://doi.org/10.1007/s12630-024-02738-w.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Lenet, T., Berthelot, P., Grudzinski, A.L. et al. Nonclinical factors affecting intraoperative red blood cell transfusion: a systematic review. Can J Anesth/J Can Anesth (2024). https://doi.org/10.1007/s12630-024-02739-9
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12630-024-02739-9