Abstract
Purpose
Cerebral autoregulation (CA) is a mechanism that acts to maintain consistent cerebral perfusion across a range of blood pressures, and impaired CA is associated with delirium. Individualized CA-derived blood pressure targets are poorly characterized in critically ill patients and the association with intensive care unit (ICU) delirium is unknown. Our objectives were to characterize optimal mean arterial pressure (MAPopt) ranges in critically ill adults without brain injury and determine whether deviations from these targets contribute to ICU delirium.
Methods
We performed a retrospective cohort analysis of patients with shock of any etiology and/or respiratory failure requiring invasive mechanical ventilation, without a neurologic admitting diagnosis. Patients were screened daily for delirium. Cerebral oximetry and mean arterial pressure data were captured for the first 24 hr from enrolment.
Results
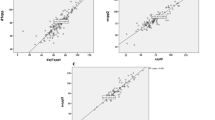
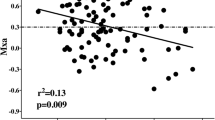
Forty-two patients with invasive blood pressure monitoring data were analyzed. Optimal mean arterial pressure targets ranged from 55 to 100 mm Hg. Optimal mean arterial pressure values were not significantly different based on history of hypertension or delirium status, and delirium was not associated with deviations from MAPopt. Nevertheless, the majority (69%) of blood pressure targets exceeded the current 65 mm Hg Surviving Sepsis guidelines.
Conclusion
We observed that MAPopt targets across patients were highly variable, but did not observe an association with the incidence of delirium. Studies designed to evaluate the impact on neurologic outcomes are needed to understand the association with individualized mean arterial pressure targets in the ICU.
Study registration
ClinicalTrials.gov (NCT02344043); first submitted 22 January 2015.
Résumé
Objectif
L’autorégulation cérébrale (AC) est un mécanisme qui agit pour maintenir une perfusion cérébrale constante pour une gamme de tensions artérielles, et une altération de l’AC est associée au delirium. Les cibles de tension artérielle individualisées dérivées de l’AC sont mal caractérisées chez les patient·es gravement malades et l’association avec le delirium à l’unité de soins intensifs (USI) est inconnue. Nos objectifs étaient de caractériser la tension artérielle moyenne optimale (TAMopt) chez les adultes gravement malades sans lésion cérébrale et de déterminer si les écarts par rapport à ces cibles contribuaient au delirium à l’USI.
Méthode
Nous avons réalisé une analyse de cohorte rétrospective de patient·es présentant un choc de toute étiologie et/ou une insuffisance respiratoire nécessitant une ventilation mécanique invasive, et n’ayant pas reçu de diagnostic d’atteinte neurologique à l’admission. Les patients ont été dépistés quotidiennement pour le delirium. Les données d’oxymétrie cérébrale et de tension artérielle moyenne ont été saisies pendant les 24 premières heures suivant le recrutement.
Résultats
Quarante-deux patient·es pour qui des données de monitorage invasif de la tension artérielle étaient disponibles ont été analysé·es. Les cibles optimales de tension artérielle moyenne variaient de 55 à 100 mm Hg. Les valeurs optimales de tension artérielle moyenne n’étaient pas significativement différentes en fonction des antécédents d’hypertension ou de delirium, et le delirium n’était pas associé à des écarts par rapport à la TAMopt. Néanmoins, la majorité (69 %) des cibles de tension artérielle dépassaient celle de 65 mm Hg préconisée par les lignes directrices Surviving Sepsis.
Conclusion
Nous avons observé que les cibles de TAMopt étaient très variables chez les patient·es, mais nous n’avons pas observé d’association avec l’incidence de delirium. Des études conçues pour évaluer l’impact sur les issues neurologiques sont nécessaires pour comprendre l’association avec les cibles de tension artérielle moyenne individualisées à l’USI.
Enregistrement de l’étude
ClinicalTrials.gov (NCT02344043); soumis pour la première fois le 22 janvier 2015.




Similar content being viewed by others
Notes
Code available from URL: https://github.com/jasmine-jk/ICU-MAP-Cleaning (accessed May 2023).
The code is available from URL: https://github.com/jasmine-jk/ICU-MAPopt.git (accessed May 2023).
References
Evans L, Rhodes A, Alhazzani W, et al. Surviving sepsis campaign: international guidelines for management of sepsis and septic shock 2021. Intensive Care Med 2021; 47: 1181–247. https://doi.org/10.1007/s00134-021-06506-y
Asfar P, Radermacher P, Ostermann M. MAP of 65: target of the past? Intensive Care Med 2018; 44: 1551–2. https://doi.org/10.1007/s00134-018-5292-8
Roberts BW, Kilgannon JH, Hunter BR, et al. Association Between elevated mean arterial blood pressure and neurologic outcome after resuscitation from cardiac arrest: results from a multicenter prospective cohort study. Crit Care Med 2019; 47: 93–100. https://doi.org/10.1097/ccm.0000000000003474
Hawryluk G, Whetstone W, Saigal R, et al. Mean arterial blood pressure correlates with neurological recovery after human spinal cord injury: analysis of high frequency physiologic data. J Neurotrauma 2015; 32: 1958–67. https://doi.org/10.1089/neu.2014.3778
Kjaergaard J, Møller JE, Schmidt H, et al. Blood-pressure targets in comatose survivors of cardiac arrest. N Engl J Med 2022; 387: 1456–66. https://doi.org/10.1056/nejmoa2208687
Saugel B, Vincent JL, Wagner JY. Personalized hemodynamic management. Curr Opin Crit Care 2017; 23: 334–41. https://doi.org/10.1097/mcc.0000000000000422
Sarkar S, Singh S, Rout A. Mean arterial pressure goal in critically ill patients: a meta-analysis of randomized controlled trials. J Clin Med Res 2022; 14: 196–201. https://doi.org/10.14740/jocmr4702
Lee KF, Wood MD, Maslove DM, Muscedere JG, Boyd JG. Dysfunctional cerebral autoregulation is associated with delirium in critically ill adults. J Cereb Blood Flow Metab 2019; 39: 2512–20. https://doi.org/10.1177/0271678x18803081
Longhitano Y, Iannuzzi F, Bonatti G, et al. Cerebral autoregulation in non-brain injured patients: a systematic review. Front Neurol 2021; 12: 732176. https://doi.org/10.3389/fneur.2021.732176
Nakano M, Nomura Y, Whitman G, et al. Cerebral autoregulation in the operating room and intensive care unit after cardiac surgery. Br J Anaesth 2021; 126: 967–74. https://doi.org/10.1016/j.bja.2020.12.043
Hori D, Brown C, Ono M, et al. Arterial pressure above the upper cerebral autoregulation limit during cardiopulmonary bypass is associated with postoperative delirium. Br J Anaesth 2014; 113: 1009–17. https://doi.org/10.1093/bja/aeu319
Brown CH, Neufeld KJ, Tian J, et al. Effect of targeting mean arterial pressure during cardiopulmonary bypass by monitoring cerebral autoregulation on postsurgical delirium among older patients: a nested randomized clinical trial. JAMA Surg 2019; 154: 819–26. https://doi.org/10.1001/jamasurg.2019.1163
Hogue CW, Brown CH, Hori D, et al. Personalized blood pressure management during cardiac surgery with cerebral autoregulation monitoring: a randomized trial. Semin Thorac Cardiovasc Surg 2021; 33: 429–38. https://doi.org/10.1053/j.semtcvs.2020.09.032
Hu AM, Qiu Y, Zhang P, et al. Higher versus lower mean arterial pressure target management in older patients having non-cardiothoracic surgery: a prospective randomized controlled trial. J Clin Anesth 2021; 69: 110150. https://doi.org/10.1016/j.jclinane.2020.110150
Khan JM, Wood MD, Lee KF, et al. Delirium, cerebral perfusion, and high-frequency vital-sign monitoring in the critically ill the CONFOCAL-2 feasibility study. Ann Am Thorac Soc 2021; 18: 112–21. https://doi.org/10.1513/annalsats.202002-093oc
Rivera-Lara L, Geocadin R, Zorrilla-Vaca A, et al. Optimizing mean arterial pressure in acutely comatose patients using cerebral autoregulation multimodal monitoring with near-infrared spectroscopy. Crit Care Med 2019; 47: 1409–15. https://doi.org/10.1097/ccm.0000000000003908
Sekhon MS, Smielewski P, Bhate TD, et al. Using the relationship between brain tissue regional saturation of oxygen and mean arterial pressure to determine the optimal mean arterial pressure in patients following cardiac arrest: a pilot proof-of-concept study. Resuscitation 2016; 106: 120–5. https://doi.org/10.1016/j.resuscitation.2016.05.019
Rikhraj KJ, Wood MD, Hoiland RL, Thiara S, Griesdale DE, Sekhon MS. Determining optimal mean arterial pressure after cardiac arrest: a systematic review. Neurocrit Care 2021; 34: 621–34. https://doi.org/10.1007/s12028-020-01027-w
Czosnyka M, Hutchinson P, Smielewski P. Treatment targets based on autoregulation parameters in neurocritical care patients. Curr Opin Crit Care 2020; 26: 109–14. https://doi.org/10.1097/mcc.0000000000000704
Griesdale DE, Sekhon MS, Wood MD, et al. Near-infrared spectroscopy to assess cerebral autoregulation and optimal mean arterial pressure in patients with hypoxic-ischemic brain injury: a prospective multicenter feasibility study. Crit Care Explor 2020; 2: e0217. https://doi.org/10.1097/cce.0000000000000217
Wood MD, Maslove D, Muscedere J, Scott SH, Day A, Boyd JG. Assessing the relationship between brain tissue oxygenation and neurological dysfunction in critically ill patients: study protocol. Int J Clin Trials 2016; 3: 98. https://doi.org/10.18203/2349-3259.ijct20162792
Du CH, Glick D, Tung A. Error-checking intraoperative arterial line blood pressures. J Clin Monit Comput 2019; 33: 407–12. https://doi.org/10.1007/s10877-018-0167-7
Khan JM, Maslove DM, Boyd JG. Optimized arterial line artifact identification algorithm cleans high-frequency arterial line data with high accuracy in critically ill patients. Crit Care Explor 2022; 4: e0814. https://doi.org/10.1097/cce.0000000000000814
Ouimet S, Kavanagh BP, Gottfried SB, Skrobik Y. Incidence, risk factors and consequences of ICU delirium. Intensive Care Med 2007; 33: 66–73. https://doi.org/10.1007/s00134-006-0399-8
Asfar P, Meziani F, Hamel JF, et al. High versus low blood-pressure target in patients with septic shock. N Engl J Med 2014; 370: 1583–93. https://doi.org/10.1056/nejmoa1312173
Ameloot K, De Deyne C, Eertmans W, et al. Early goal-directed haemodynamic optimization of cerebral oxygenation in comatose survivors after cardiac arrest: the Neuroprotect post-cardiac arrest trial. Eur Heart J 2019; 40: 1804–14. https://doi.org/10.1093/eurheartj/ehz120
Lamontagne F, Richards-Belle A, Thomas K, et al. Effect of reduced exposure to vasopressors on 90-day mortality in older critically ill patients with vasodilatory hypotension: a randomized clinical trial. JAMA 2020; 323: 938–49. https://doi.org/10.1001/jama.2020.0930
Grand J, Meyer AS, Kjaergaard J, et al. A randomised double-blind pilot trial comparing a mean arterial pressure target of 65 mm Hg versus 72 mm Hg after out-of-hospital cardiac arrest. Eur Hear Journal Acute Cardiovasc Care 2020; 9: S100–9. https://doi.org/10.1177/2048872619900095
Kato R, Pinsky MR. Personalizing blood pressure management in septic shock. Ann Intensive Care 2015; 5: 41. https://doi.org/10.1186/s13613-015-0085-5
Maldonado JR. Acute brain failure: pathophysiology, diagnosis, management, and sequelae of delirium. Crit Care Clin 2017; 33: 461–519. https://doi.org/10.1016/j.ccc.2017.03.013
Mehta S, Cook D, Devlin JW, et al. Prevalence, risk factors, and outcomes of delirium in mechanically ventilated adults. Crit Care Med 2015; 43: 557–66. https://doi.org/10.1097/ccm.0000000000000727
Wassenaar A, van den Boogaard M, van Achterberg T, et al. Multinational development and validation of an early prediction model for delirium in ICU patients. Intensive Care Med 2015; 41: 1048–56. https://doi.org/10.1007/s00134-015-3777-2
Jentzer JC, Coons JC, Link CB, Schmidhofer M. Pharmacotherapy update on the use of vasopressors and inotropes in the intensive care unit. J Cardiovasc Pharmacol Ther 2015; 20: 249–60. https://doi.org/10.1177/1074248414559838
Hylands M, Moller MH, Asfar P, et al. A systematic review of vasopressor blood pressure targets in critically ill adults with hypotension. Can J Anesth 2017; 64: 703–15. https://doi.org/10.1007/s12630-017-0877-1
Khan BA, Perkins AJ, Gao S, et al. The confusion assessment method for the ICU-7 delirium severity scale: a novel delirium severity instrument for use in the ICU. Crit Care Med 2017; 45: 851–7. https://doi.org/10.1097/ccm.0000000000002368
Dünser MW, Takala J, Ulmer H, et al. Arterial blood pressure during early sepsis and outcome. Intensive Care Med 2009; 35: 1225–33. https://doi.org/10.1007/s00134-009-1427-2
Poukkanen M, Wilkman E, Vaara ST, et al. Hemodynamic variables and progression of acute kidney injury in critically ill patients with severe sepsis: data from the prospective observational FINNAKI study. Crit Care 2013; 17: R295. https://doi.org/10.1186/cc13161
Bickler PE, Feiner JR, Rollins MD. Factors affecting the performance of 5 cerebral oximeters during hypoxia in healthy volunteers. Anesth Analg 2013; 117: 813–23. https://doi.org/10.1213/ane.0b013e318297d763
Steppan J, Hogue CW Jr. Cerebral and tissue Oximetry. Best Pract Res Clin Anaesthesiol 2014; 28: 429–39. https://doi.org/10.1016/j.bpa.2014.09.002
Schneider A, Minnich B, Hofstätter E, Weisser C, Hattinger-Jürgenssen E, Wald M. Comparison of four near-infrared spectroscopy devices shows that they are only suitable for monitoring cerebral oxygenation trends in preterm infants. Acta Paediatr 2014; 103: 934–8. https://doi.org/10.1111/apa.12698
Sakusic A, O’Horo JC, Dziadzko M, et al. Potentially modifiable risk factors for long-term cognitive impairment after critical illness: a systematic review. Mayo Clin Proc 2018; 93: 68–82. https://doi.org/10.1016/j.mayocp.2017.11.005
Author contributions
Jasmine M. Khan and J. Gordon Boyd contributed to all aspects of this manuscript, including study conception and design; acquisition, analysis, and interpretation of data; and drafting the article. Abigail Shore, Kevin F. H. Lee, Michael D. Wood, and David M. Maslove contributed to acquisition, analysis, and interpretation of data. Miranda Hunt and Ilinca Georgescu contributed to the acquisition of data. John Muscedere contributed to conception and design of the study.
Disclosures
The FORESIGHT Cerebral oximeter used in this study was provided as an in-kind contribution by Casmed (Canada), now Edwards Lifesciences.
Funding statement
The original CONFOCAL1 study was supported by funding to Dr. J. Gordon Boyd from the Southeastern Ontario Academic Medical Organization New Clinician Scientist Program and Physician Services Incorporated.
Prior conference presentations
A draft version of this work was presented at the 16th European Delirium Association Annual Meeting (2–4 November 2022, Milan, Italy).
Editorial responsibility
This submission was handled by Dr. Alexis F. Turgeon, Associate Editor, Canadian Journal of Anesthesia/Journal canadien d’anesthésie.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Khan, J.M., Shore, A., Lee, K.F.H. et al. Cerebral autoregulation-based mean arterial pressure targets and delirium in critically ill adults without brain injury: a retrospective cohort study. Can J Anesth/J Can Anesth 71, 107–117 (2024). https://doi.org/10.1007/s12630-023-02609-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12630-023-02609-w