Abstract
Purpose
We sought to understand the beliefs and practices of Canadian intensivists regarding their use of ketamine as a sedative in critically ill patients and to gauge their interest in a randomized controlled trial (RCT) examining its use in the intensive care unit (ICU).
Methods
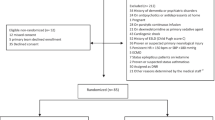
We designed and validated an electronic self-administered survey examining the use of ketamine as a sedative infusion for ICU patients. We surveyed 400 physician members of the Canadian Critical Care Society (CCCS) via email between February and April 2022 and sent three reminders at two-week intervals. The survey was redistributed in January 2023 to improve the response rate.
Results
We received 87/400 (22%) completed questionnaires. Most respondents reported they rarely use ketamine as a continuous infusion for sedation or analgesia in the ICU (52/87, 58%). Physicians reported the following conditions would make them more likely to use ketamine: asthma exacerbation (73/87, 82%), tolerance to opioids (68/87, 77%), status epilepticus (44/87, 50%), and severe acute respiratory distress syndrome (33/87, 38%). Concern for side-effects that limited respondents’ use of ketamine include adverse psychotropic effects (61/87, 69%) and delirium (47/87, 53%). The majority of respondents agreed there is need for an RCT to evaluate ketamine as a sedative infusion in the ICU (62/87, 71%).
Conclusion
This survey of Canadian intensivists illustrates that use of ketamine as a continuous infusion for sedation is limited, and is at least partly driven by concerns of adverse psychotropic effects. Canadian physicians endorse the need for a trial investigating the safety and efficacy of ketamine as a sedative for critically ill patients.
Résumé
Objectif
Nous avons cherché à comprendre les croyances et les pratiques des intensivistes pratiquant au Canada concernant leur utilisation de la kétamine comme sédatif chez la patientèle gravement malade et à évaluer leur intérêt pour une étude randomisée contrôlée (ERC) examinant son utilisation à l’unité de soins intensifs (USI).
Méthode
Nous avons mis au point et validé un sondage électronique auto-administré examinant l’utilisation de la kétamine comme perfusion sédative pour les patient·es aux soins intensifs. Nous avons envoyé le sondage à 400 médecins membres de la Société canadienne de soins intensifs (SCCC) par courriel entre février et avril 2022 et envoyé trois rappels à intervalles de deux semaines. Le sondage a été redistribué en janvier 2023 afin d’améliorer le taux de réponse.
Résultats
Nous avons reçu 87 questionnaires remplis sur 400 (22 %). La plupart des personnes répondantes ont déclaré qu’elles utilisaient rarement la kétamine en perfusion continue pour la sédation ou l’analgésie à l’USI (52/87, 58 %). Les médecins ont déclaré que les conditions suivantes les rendraient plus susceptibles d’utiliser de la kétamine : une exacerbation de l’asthme (73/87, 82 %), une tolérance aux opioïdes (68/87, 77 %), un état de mal épileptique (44/87, 50 %) et un syndrome de détresse respiratoire aigu (33/87, 38 %). Les inquiétudes quant aux effets secondaires qui ont limité l’utilisation de la kétamine par les répondant·es comprennent les effets psychotropes indésirables (61/87, 69 %) et le delirium (47/87, 53 %). La majorité des personnes répondantes étaient d’accord qu’une ERC est nécessaire pour évaluer la kétamine en tant que perfusion sédative à l’USI (62/87, 71 %).
Conclusion
Cette enquête menée auprès d’intensivistes au Canada montre que l’utilisation de la kétamine comme perfusion continue pour la sédation est limitée, au moins en partie en raison d’inquiétudes liées aux effets psychotropes indésirables. Les médecins pratiquant au Canada reconnaissent la nécessité d’une étude sur l’innocuité et l’efficacité de la kétamine comme sédatif pour la patientèle gravement malade.




Similar content being viewed by others
References
Reade MC, Finfer S. Sedation and delirium in the intensive care unit. N Engl J Med 2014; 370: 444–54. https://doi.org/10.1056/nejmra1208705
Stein-Parbury J, McKinley S. Patients' experiences of being in an intensive care unit: a select literature review. Am J Crit Care 2000; 9: 20–7.
Hughes CG, McGrane S, Pandharipande PP. Sedation in the intensive care setting. Clin Pharmacol 2012; 4: 53–63. https://doi.org/10.2147/cpaa.s26582
Ragule CA, Wade KL, Rubino S. Update on the physiologic effects of ketamine in general anesthesia and spinal blockade: a review of the literature. AANA J 2019; 87: 489–94.
Siow WT, Tang SH, Agrawal RV, Tan AY, See KC. Essential ICU drug shortages for COVID-19: what can frontline clinicians do? Crit Care 2020; 24: 260. https://doi.org/10.1186/s13054-020-02971-x
Duprey MS, Dijkstra-Kersten SM, Zaal IJ, et al. Opioid use increases the risk of delirium in critically ill adults independently of pain. Am J Respir Crit Care Med 2021; 204: 566–72. https://doi.org/10.1164/rccm.202010-3794oc
Murray BP, Newsome AS. Opioids for sedation: has the pendulum swung too far? Am J Respir Crit Care Med 2021; 204: 611. https://doi.org/10.1164/rccm.202104-1012le
Wunsch H, Hill AD, Fu L, et al. New opioid use after invasive mechanical ventilation and hospital discharge. Am J Respir Crit Care Med 2020; 202: 568–75. https://doi.org/10.1164/rccm.201912-2503oc
Haas LE, Karakus A, Holman R, Cihangir S, Reidinga AC, de Keizer NF. Trends in hospital and intensive care admissions in the Netherlands attributable to the very elderly in an ageing population. Crit Care 2015; 19: 353. https://doi.org/10.1186/s13054-015-1061-z
Kim JY, Kim JH, Yee J, Song SJ, Gwak HS. Risk factors of opioid-induced adverse reactions in elderly male outpatients of Korea Veterans Hospital. BMC Geriatr 2018; 18: 293. https://doi.org/10.1186/s12877-018-0990-1
LimeSurvey GmbH. Welcome to LimeSurvey. The LifeSurvey. Available from URL: https://www.limesurvey.org (accessed June 2023).
Burns KE, Duffett M, Kho ME, et al. A guide for the design and conduct of self-administered surveys of clinicians. CMAJ 2008; 179: 245–52. https://doi.org/10.1503/cmaj.080372
Boateng GO, Neilands TB, Frongillo EA, Melgar-Quiñonez HR, Young SL. Best practices for developing and validating scales for health, social, and behavioral research: a primer. Front Public Health 2018; 6: 149. https://doi.org/10.3389/fpubh.2018.00149
American Association of Public Opinion Research. Standard definitions: final dispositions of case codes and outcome rates for surveys. 2016. Available from URL: https://aapor.org/wp-content/uploads/2022/11/Standard-Definitions20169theditionfinal.pdf (accessed July 2023).
Green SM, Roback MG, Krauss B, et al. Predictors of airway and respiratory adverse events with ketamine sedation in the emergency department: an individual-patient data meta-analysis of 8,282 children. Ann Emerg Med 2009; 54: 158–68. https://doi.org/10.1016/j.annemergmed.2008.12.011
Newton A, Fitton L. Intravenous ketamine for adult procedural sedation in the emergency department: a prospective cohort study. Emerg Med J 2008; 25: 498–501. https://doi.org/10.1136/emj.2007.053421
Vardy JM, Dignon N, Mukherjee N, Sami DM, Balachandran G, Taylor S. Audit of the safety and effectiveness of ketamine for procedural sedation in the emergency department. Emerg Med J 2008; 25: 579–82. https://doi.org/10.1136/emj.2007.056200
Sener S, Eken C, Schultz CH, Serinken M, Ozsarac M. Ketamine with and without midazolam for emergency department sedation in adults: a randomized controlled trial. Ann Emerg Med 2011; 57: 109–14. https://doi.org/10.1016/j.annemergmed.2010.09.010
Strayer RJ, Nelson LS. Adverse events associated with ketamine for procedural sedation in adults. Am J Emerg Med 2008; 26: 985–1028. https://doi.org/10.1016/j.ajem.2007.12.005
Buckland DM, Crowe RP, Cash RE, et al. Ketamine in the prehospital environment: a national survey of paramedics in the United States. Prehosp Disaster Med 2018; 33: 23–8. https://doi.org/10.1017/s1049023x17007142
Yuhalogarasan A, Barclay C, Verbeek PR. Low-dose ketamine in the prehospital setting. CMAJ 2022; 194: E171. https://doi.org/10.1503/cmaj.80599
Kurdi MS, Theerth KA, Deva RS. Ketamine: current applications in anesthesia, pain, and critical care. Anesth Essays Res 2014; 8: 283–90. https://doi.org/10.4103/0259-1162.143110
Hui C, Monteiro JP, Trivedi D, Vasant D, Carino G. Effect of ketamine on vasopressor needs in mechanically ventilated patients: a retrospective study. Brown K Hosp Med 2022; 1: 1–9. https://doi.org/10.56305/001c.36988
Shrestha GS, Shrestha N, Lamsal R, et al. Emergency intubation in Covid-19. N Engl J Med 2021; 384: e20. https://doi.org/10.1056/nejmvcm2007198
Ilg A BC, Shih J, Yankama T, Hayes Mm, Moskowitz A. Ketamine in critical care: exploring before and during COVID-19 attitudes and practices. Am J Respir Crit Care Med 2022; 205: A3556. Available from URL: https://www.atsjournals.org/https://doi.org/10.1164/ajrccm-conference.2022.205.1_MeetingAbstracts.A3556 (accessed June 2023).
Patel R, Samiee-Zafarghandy S, Ziesenitz V, et al. US drug shortages compared to the World Health Organization's model list of essential medicines for children: a cross-sectional study. Am J Health Syst Pharm 2022; 79: 2012–7. https://doi.org/10.1093/ajhp/zxac210
Pisani MA, Kong SY, Kasl SV, Murphy TE, Araujo KL, Van Ness PH. Days of delirium are associated with 1-year mortality in an older intensive care unit population. Am J Respir Crit Care Med 2009; 180: 1092–7. https://doi.org/10.1164/rccm.200904-0537oc
Luz M, Barreto BB, de Castro RE, et al. Practices in sedation, analgesia, mobilization, delirium, and sleep deprivation in adult intensive care units (SAMDS-ICU): an international survey before and during the COVID-19 pandemic. Ann Intensive Care 2022; 12: 9. https://doi.org/10.1186/s13613-022-00985-y
Gershengorn HB, Wunsch H. Temporal trends and variability in ketamine use for mechanically ventilated adults in the United States. Ann Am Thorac Soc 2022; 19: 1534–42. https://doi.org/10.1513/annalsats.202112-1376oc
Kishimoto T, Chawla JM, Hagi K, et al. Single-dose infusion ketamine and non-ketamine N-methyl-d-aspartate receptor antagonists for unipolar and bipolar depression: a meta-analysis of efficacy, safety and time trajectories. Psychol Med 2016; 46: 1459–72. https://doi.org/10.1017/s0033291716000064
Chou R, Gordon DB, de Leon-Casasola OA, et al. Management of postoperative pain: a clinical practice guideline from the American Pain Society, the American Society of Regional Anesthesia and Pain Medicine, and the American Society of Anesthesiologists' Committee on Regional Anesthesia, Executive Committee, and Administrative Council. J Pain 2016; 17: 131–57. https://doi.org/10.1016/j.jpain.2015.12.008
Kraus C, Rabl U, Vanicek T, et al. Administration of ketamine for unipolar and bipolar depression. Int J Psychiatry Clin Pract 2017; 21: 2–12. https://doi.org/10.1080/13651501.2016.1254802
Perumal DK, Adhimoolam M, Selvaraj N, Lazarus SP, Mohammed MA. Midazolam premedication for Ketamine-induced emergence phenomenon: a prospective observational study. J Res Pharm Pract 2015; 4: 89–93. https://doi.org/10.4103/2279-042x.155758
Groth CM, Droege CA, Connor KA, et al. Multicenter retrospective review of ketamine use in the ICU. Crit Care Explor 2022; 4: e0633. https://doi.org/10.1097/cce.0000000000000633
Perbet S, Verdonk F, Godet T, et al. Low doses of ketamine reduce delirium but not opiate consumption in mechanically ventilated and sedated ICU patients: a randomised double-blind control trial. Anaesth Crit Care Pain Med 2018; 37: 589–95. https://doi.org/10.1016/j.accpm.2018.09.006
Baron R, Binder A, Biniek R, et al. Evidence and consensus based guideline for the management of delirium, analgesia, and sedation in intensive care medicine. Revision 2015 (DAS-Guideline 2015)—short version. Ger Med Sci 2015; 13: Doc19. https://doi.org/10.3205/000223
Devlin JW, Skrobik Y, Gélinas C, et al. Clinical practice guidelines for the prevention and management of pain, agitation/sedation, delirium, immobility, and sleep disruption in adult patients in the ICU. Crit Care Med 2018; 46: e825–73. https://doi.org/10.1097/ccm.0000000000003299
Canadian Medical Association. Critical care medicine profile. 2019. Available from URL: https://www.cma.ca/sites/default/files/2020-10/critical-care-e.pdf (accessed July 2023).
Burns KEA, Moss M, Lorens E, et al. Wellness and coping of physicians who worked in ICUs during the pandemic: a multicenter cross-sectional North American survey. Crit Care Med 2022; 50: 1689–700.
de Koning R, Egiz A, Kotecha J, et al. Survey fatigue Dduring the COVID-19 pandemic: an analysis of neurosurgery survey response rates. Front Surg 2021; 8: 690680. https://doi.org/10.3389/fsurg.2021.690680
Author contributions
Bram Rochwerg and Sameer Sharif designed the study, analyzed the results, and drafted the initial manuscript. Laveena Munshi, Lisa Burry, Sara Gray, Dipayan Chaudhuri, Sangeeta Mehta, Mark Duffett, and Reed A. Siemieniuk all equally contributed in editing the contents of the manuscript.
Acknowledgement
We would like to thank the CCCS members for their help with disseminating the survey. We would also like to thank all the CCCS members who responded to the survey.
Disclosures
None.
Funding statement
Dr. Sameer Sharif holds a McMaster University Department of Medicine Internal Career Research Award.
Editorial responsibility
This submission was handled by Dr. Alexis F. Turgeon, Associate Editor, Canadian Journal of Anesthesia/Journal canadien d’anesthésie.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Sharif, S., Munshi, L., Burry, L. et al. Ketamine sedation in the intensive care unit: a survey of Canadian intensivists. Can J Anesth/J Can Anesth 71, 118–126 (2024). https://doi.org/10.1007/s12630-023-02608-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12630-023-02608-x