Abstract
Purpose
Intravascular fluids are a necessary and universal component of cardiac surgical patient care. Both crystalloids and colloids are used to maintain or restore circulating plasma volume and ensure adequate organ perfusion. In Canada, human albumin solution (5% or 25% concentration) is a colloid commonly used for this purpose. In this narrative review, we discuss albumin supply in Canada, explore the perceived advantages of albumin, and describe the clinical literature supporting and refuting albumin use over other fluids in the adult cardiac surgical population.
Source
We conducted a targeted search of PubMed, Embase, Medline, Web of Science, ProQuest Dissertations and Theses Global, the Cochrane Central Register of Controlled trials, and the Cochrane Database of Systematic Reviews. Search terms included albumin, colloid, cardiac surgery, bleeding, hemorrhage, transfusion, and cardiopulmonary bypass.
Principal findings
Albumin is produced from fractionated human plasma and imported into Canada from international suppliers at a cost of approximately $21 million CAD per annum. While it is widely used in cardiac surgical patients across the country, it is approximately 30-times more expensive than equivalent doses of balanced crystalloid solutions, with wide inter-institutional variability in use and no clear association with improved outcomes. There is a general lack of high-quality evidence for the superiority of albumin over crystalloids in this patient population, and conflicting evidence regarding safety.
Conclusions
In cardiac surgical patients, albumin is widely utilized despite a lack of high- quality evidence supporting its efficacy or safety. A well-designed randomized controlled trial is needed to clarify the role of albumin in cardiac surgical patients.
Résumé
Objectif
Les liquides intravasculaires sont une composante nécessaire et universelle des soins aux patients de chirurgie cardiaque. Les cristalloïdes et les colloïdes sont utilisés pour maintenir ou restaurer le volume plasmatique en circulation et assurer une perfusion adéquate des organes. Au Canada, les solutions d’albumine humaine (concentration de 5 % ou 25 %) constituent un colloïde couramment utilisé à cette fin. Dans ce compte rendu narratif, nous discutons de l’approvisionnement en albumine au Canada, explorons les avantages perçus de l’albumine et décrivons la littérature clinique soutenant ou réfutant l’utilisation de l’albumine par rapport à d’autres solutions pour la population chirurgicale cardiaque adulte.
Sources
Nous avons effectué une recherche ciblée dans les bases de données PubMed, Embase, Medline, Web of Science, ProQuest Dissertations and Theses Global, le Cochrane Central Register of Controlled trials et la Cochrane Database of Systematic Reviews. Les termes de recherche (en anglais) incluaient albumine, colloid, cardiac surgery, bleeding, hemorrhage, transfusion, et cardiopulmonary bypass (soit albumine, colloïde, chirurgie cardiaque, saignement, hémorragie, transfusion et circulation extracorporelle).
Constatations principales
L’albumine est fabriquée à partir de plasma humain fractionné et importée au Canada à partir de fournisseurs internationaux au coût d’environ 21 millions CAD par année. Bien qu’elle soit largement utilisée chez les patients de chirurgie cardiaque à travers le pays, elle est environ 30 fois plus coûteuse que des doses équivalentes de solutions cristalloïdes équilibrées, avec une grande variabilité interinstitutionnelle quant à son utilisation et aucune association claire avec des devenirs améliorés. Il n’existe en général pas de données probantes de qualité élevée confirmant la supériorité de l’albumine par rapport aux cristalloïdes dans cette population de patients, et les données probantes quant à son innocuité sont contradictoires.
Conclusion
Chez les patients de chirurgie cardiaque, l’albumine est largement utilisée en dépit d’un manque de données probantes de haute qualité soutenant son efficacité ou son innocuité. Une étude randomisée contrôlée bien conçue est nécessaire pour clarifier le rôle de l’albumine chez les patients de chirurgie cardiaque.
Similar content being viewed by others
Cardiac surgical patients uniformly require intravascular fluid administration. Crystalloids, colloids, and allogeneic blood products are all commonly infused during routine patient care, both for priming of the cardiopulmonary bypass (CPB) circuit and maintenance of adequate intravascular volume in response to blood loss.1 Colloids are synthetic or natural substances that exert an oncotic pressure facilitating intravascular fluid retention. They differ substantially from crystalloid solutions, which are electrolyte solutions of varying compositions and physiologic similarity to human plasma (Table 1). Synthetic colloids are not commonly used in Canada because of safety concerns, particularly relating to the hydroxyethyl starches.2 Thus, intravenous albumin, which is a natural protein colloid purified from human plasma, is the colloid of choice at many Canadian cardiac surgical centres. Albumin is distributed by Canadian Blood Services and Héma-Québec as a sterile, pathogen-reduced blood product in a 5% (250 mL [12.5 g] or 500 mL [25 g]) solution and a 25% (100 mL [25 g]) solution. The 5% solution is thought to exert a colloid osmotic pressure similar to that of human plasma, while the 25% solution is typically used to treat oncotic deficits.
Albumin is a water-soluble, globular, negatively charged 65 kDa protein that is endogenously synthesized in the liver and catabolized in the endothelium, as well as degraded in muscle, skin, and other organs.3 It represents approximately half of the total plasma protein content, and while approximately 60% of albumin is interstitial and is an important contributor to interstitial oncotic pressure, much of the debate surrounding albumin as a resuscitation fluid is centred on the 40% of total body albumin found intravascularly, which is thought to contribute to 80% of total plasma oncotic pressure.3 Despite the focus on intravascular volume expansion, albumin has numerous other biologic roles, including binding of endogenous and exogenous ligands (drugs, bilirubin, ions, hormones), antioxidant properties, and nitric oxide modulation.3
Albumin was first crystallized in 1934, and subsequently introduced as an intravascular solution in numerous jurisdictions throughout the 1940’s—being widely adopted throughout the decades as a resuscitation fluid in a variety of patient populations.4 The crystalloid vs colloid debate of the last several decades5 brought albumin into the spotlight in the critical care literature, and germinated more rigorous study of its potential advantages and drawbacks. This ongoing debate produced a number of large, randomized controlled trials (RCTs) of albumin use in critically ill patients that even today provide the highest quality evidence informing use in many other patient populations, where the evidence is often restricted to retrospective observational data or small prospective studies.6,7,8
There is little clarity regarding the role of albumin in cardiac surgical patients, with significant heterogeneity in where and how albumin is used in this population in Canada and elsewhere.9,10 Given the well-known safety concerns associated with synthetic colloid alternatives to albumin, such as the hydroxyethyl starches,11 the role of albumin in lieu of or to supplement crystalloids will be the main focus of this article. In this narrative review, our aims are fourfold: 1) to detail the supply and economic environment of albumin use in Canada; 2) to explore the perceived advantages of albumin suggested by early clinical or preclinical data compared with other resuscitation fluids in the perioperative management of cardiac surgery patients; 3) to describe the clinical evidence relating to albumin use in cardiac surgical patients, which is largely informed by the more general surgical and critical care settings; and 4) to highlight the most important controversies drawn from the currently available evidence, including potential future areas of research.
Methods
This narrative review is based on a targeted search of the literature databases including PubMed, Embase, Medline, Web of Science, ProQuest Dissertations and Theses Global, the Cochrane Central Register of Controlled trials, and the Cochrane Database of Systematic Reviews, using search terms combining albumin, colloid, cardiac surgery, bleeding, hemorrhage, transfusion, and cardiopulmonary bypass. Searches of trial registries (ClinicalTrials.gov and WHO ICTRP) were also included. References cited in the retrieved literature were also examined for relevance. Articles were included if they described an association between albumin use in cardiac surgical patients and clinical outcomes. Non-English language articles and abstracts not subsequently published as articles were excluded. This review followed the SANRA reporting recommendations for high-quality narrative reviews.12
The context of albumin prescribing in Canada
As a blood product, albumin is relatively expensive, at approximately 62 CAD per dose (5% 500 mL or 25% 100 mL), compared with approximately 2 CAD per 1 L dose for crystalloids. Medical use of albumin solution is estimated to cost the Canadian healthcare system approximately 21 million CAD per annum,Footnote 1 20% of which is related to cardiac surgical patients.13 Currently, Canada lacks a plasma fractionation company, and is dependent on other developed nations where donors are paid (largely the United States) for its albumin supply (Table 2).
Canadian Blood Services officially recognizes albumin use for a narrow set of specific indications, including 1) patients with liver disease and bacterial peritonitis, 2) large volume paracentesis in patients with cirrhosis, 3) hepatorenal syndrome type 1, 4) thermal injury involving > 50% body surface area, and 5) therapeutic plasma exchange.14 Notably, this list does not include the resuscitation of cardiac surgical patients. Nevertheless, albumin remains freely available for clinicians to prescribe at their discretion. The provincial Ministries of Health across Canada are required to pay for all albumin orders issued in Canadian hospitals, regardless of the cited indication for use or the quality of evidence supporting its use in a given patient population. Despite general encouragement at the local level and from externally published advisory groups encouraging “restrictive” albumin use, between 2003 and 2009 the amount of albumin issued to Canadian hospitals (excluding Québec) grew by 51.8% overall.13
Practice surveys confirm the popularity of albumin as a resuscitation fluid in North America in cardiac surgical patients, whereas in Europe, balanced crystalloid is preferred.15,16 In a European practice survey, crystalloids or a combination of crystalloids with synthetic colloids (primarily gelatins) were used in 89% of perioperative cardiac surgical patients. Only 11% of European cardiac anesthesiologists considered using albumin in the operating room, and the majority did not change their practice for postoperative care in the intensive care unit (ICU).17 However, in the United States, 37% of anesthesiologists and 39% of surgeons considered albumin their first choice fluid in the operating room when replacing intravascular volume for non-bleeding patients, favouring it even over crystalloids in many situations.15 Given the significant associated costs, there have been noted initiatives to decrease albumin utilization at different centres in the United States.17 Nevertheless, the economic benefits of albumin reduction and its impact on patient outcomes is based on only a few studies at present,17 and currently there are no high-quality, large RCTs or systematic reviews and meta-analyses available.17,18,19
There are few appealing substitutes to albumin that offer a colloid oncotic effect and have acceptable safety in cardiac surgical patients. While frozen plasma has in the past been suggested for volume expansion and prevention of coagulopathy, evidence suggests that this practice has little benefit while exposing the patient to allogeneic blood products and potential transfusion complications, particularly transfusion-related acute lung injury.20,21,22 With an overall decline in recent years in the use of synthetic colloids (i.e., hydroxyethyl starches) because of their association with increased incidence of acute kidney injury (AKI), coagulopathy, and mortality in the critical care population, there are few viable synthetic colloid options remaining.23,24,25 Perhaps unsurprisingly given the lack of alternatives, there has been a resultant resurgence in the use of human albumin solution to supplement crystalloids for resuscitation. Thus, despite a lack of compelling clinical evidence indicating superiority over balanced crystalloids, albumin remains a frequently utilized option in the armamentarium of many perioperative clinicians.26,27,28,29,30
The perceived advantages of albumin influencing its use in cardiac surgical patients: preclinical and preliminary clinical evidence
Intravenous fluid therapy is a key component of perioperative cardiac surgical care. Both crystalloids and colloids are commonly used for priming the CPB circuit, volume expansion on CPB, management of intra- and postoperative hypotension, and volume restoration in the bleeding patient prior to or in addition to the provision of allogeneic blood products. Individualized hemodynamic-guided fluid therapy and blood product transfusion, with judicious vasopressor and inotrope use, is a crucial component of perioperative management in cardiac surgical patients to maintain end-organ perfusion, avoid complications of excessive fluid volumes, and improve patient outcomes.1,31,32,33
Cardiac surgical patients tend to receive large volumes of intravenous fluids, particularly in the first 24 postoperative hours, with marked heterogeneity in clinical practice and little consensus on the optimal fluid to be used.34,35 The principles guiding fluid management in cardiac surgery differ from other types of major surgery. The fluid kinetics are more complex and involve a delicate balance of multiple perioperative factors.31 These include the patient’s age, body weight, intraprocedural CPB (circuit, priming volume, fluid composition), cardioplegia solution, thermoregulation, and the use of vasoactive drugs. Low cardiac output and renal dysfunction are common and frequently multifactorial in their etiology.36,37 Surgical factors such as the procedure specifics, surgical urgency, and complexity of the case also contribute.31 The inflammatory changes and direct tissue injury associated with both CPB, ischemia-reperfusion injury, and the surgery itself result in endothelial glycocalyx dysfunction, and altered hydrostatic and oncotic pressure gradients, which lead to increased vascular permeability and transcapillary fluid shifts.36,37
While the superiority of intravenous albumin over balanced crystalloids as a volume expander in cardiac surgery patients has not been established, its use is primarily guided by the belief that it is more effective than crystalloids in preventing interstitial edema through its oncotic effect, and in maintaining microcirculatory perfusion and endothelial glycocalyx integrity.15,38,39 Relating to its colloid oncotic effect, albumin is thought to produce a more sustained intravascular volume expansion compared with crystalloids for a given volume, ostensibly preventing generalized fluid overload and minimizing interstitial edema—with resultant beneficial end-organ effects. This potential volume-sparing effect of colloids is perceived as advantageous in preventing fluid overload complications such as pulmonary edema and right ventricular impairment; nevertheless, it is variably supported by the published literature.39,40,41 Additionally, albumin may also function as an antioxidant to reduce inflammation,42 may play a role in preserving platelet number and function,43 and through its action as a nitric oxide scavenger may decrease nitric oxide mediated vasodilation.44 These effects may be of particular benefit during and after CPB.
Avoiding fluid overload is one of the central tenets of the perioperative care of cardiac surgical patients. Both hypovolemia and hypervolemia are associated with end-organ dysfunction, and the associated morbidity has been described as a “parabolic-U-shape” curve.45 In non-cardiac surgery, a positive fluid balance during the first three to seven days in the ICU is associated with increased in-hospital mortality.46,47 In many cardiac surgery patients, the presence of concomitant cardiopulmonary and renal dysfunction does not allow “excessive” volume administration to treat hypotension. While “excessive” is not well defined, a retrospective study of 1,358 cardiac surgical patients showed a more than three-fold increase in 90-day mortality after 4 L of intraoperative fluid.48 A progressively positive cumulative fluid balance may also be associated with increased renal adverse events, including new requirement for postoperative dialysis.49
Given the association of excess fluid with adverse outcomes, albumin has become popular as a colloid “volume-sparing” bridge to restore peripheral perfusion and to wean vasopressors, although this is not a standardized practice.39 Notably, the addition of albumin to balanced crystalloid resuscitation to minimize the total fluid balance has not been definitely associated with improved patient outcomes such as major morbidity or mortality. Four to five percent human albumin solution is generally iso-oncotic and isotonic with plasma, and is thought to lead to an intravascular volume expansion similar to the infused volume, whereas hyperoncotic 20–25% albumin solutions are purported to result in an intravascular volume increase four times higher than the infused volume.14 This expansion effect may last for up to 24 hr, although in sicker patients with more severe or persistent endotheliopathy the magnitude and duration of this effect may be unpredictable.50 It has been shown that the actual ratio of intravascular to administered volume of colloids in critically ill patients may be closer to 1:1.2, which is significantly less than previously believed.51,52 This magnitude of oncotic effect may in part be modulated by impairments in the integrity of the endothelial glycocalyx associated with cardiac surgery and CPB, leading to increased vascular permeability, decreased intravascular colloid retention, and worsened microvascular perfusion.53,54,55
Distinct from the use of albumin as a perioperative resuscitation fluid, albumin may also be used to prime the CPB circuit along with crystalloids. In North America, approximately 30% of perfusionists use a mixture of 25% albumin and crystalloids for this purpose.15 Several studies have suggested that the use of albumin in the CPB priming solution is beneficial for maintaining colloid oncotic pressure.56,57,58,59 In a 2004 meta-analysis incorporating 21 studies with a total of 1,346 patients, the addition of albumin into the priming fluid was found to be associated with a reduced absolute drop in platelet count while on CPB, better preserved intravascular colloid oncotic pressure, and decreased postoperative weight gain and on-bypass fluid balance.57 Nevertheless, the limited available data show no difference in clinically important, “hard” patient outcomes.60 In recent years, methods to reduce the priming volume (e.g., autologous priming, mini-circuits) have gained popularity given the evidence that they reduce perioperative blood transfusions, potentially reducing the perceived advantages of including albumin in the priming solution.61,62
Clinical evidence for the use of albumin in cardiac surgical patients
Most of the evidence comparing albumin with crystalloids stems from critical care studies that recruited from mixed medical and trauma populations, thus limiting generalizability to the cardiac surgical patient population. This is related to significant underlying physiologic differences in the cardiac surgical population, as well as different patterns of albumin use in current cardiac surgical care compared with administration protocols in prior large critical care trials.7,8,52
In 1998, a Cochrane meta-analysis was published showing a significantly increased risk of harm to critically ill patients administered albumin.63 Of the initial 32 RCTS eligible for inclusion, 14 included surgical patients, and of those, only two had cardiac surgical patients as the primary population of interest. From the 30 RCTs reporting mortality data and involving a total of 1,419 patients, the overall pooled relative risk of death associated with albumin administration was 1.68 (95% confidence interval [CI], 1.26 to 2.23). This had a marked influence on clinical practice at the time, and the use of albumin fell out of favour, with usage decreasing by approximately 50% over six months in some jurisdictions.64
The safety of albumin remained a contested topic in subsequent years, and in 2004 the Saline versus Albumin Fluid Evaluation (SAFE) study, one of the largest albumin studies to date, was published.52 The SAFE study found no benefit on morbidity or mortality of 4% albumin compared with normal saline when used for fluid resuscitation for the initial 28 days from ICU admission. The population included a heterogeneous group of 6,997 ICU patients, from which cardiac surgical patients were notably excluded. Nevertheless, a subgroup analysis of patients with “severe sepsis” (35% of whom had septic shock) showed a potential benefit of 4% albumin, with an adjusted odds ratio (OR) for death of 0.71 (95% CI, 0.52 to 0.97; P = 0.03). Patients who were randomized to the albumin group also received more red blood cell transfusions within the first 48 hr of the study (mean [standard deviation (SD)], 106.5 [321.4] mL vs 61.1 [235.2] mL; P < 0.001). The reasons for this are unclear but may have involved greater hemodilution or coagulopathy associated with albumin, leading to increased bleeding and transfusion.65
Subsequent studies, such as the 2014 Albumin Italian Outcome Sepsis (ALBIOS) trial, compared 20% albumin with crystalloid with crystalloid alone in 1,818 patients with septic shock, but found no mortality benefit at 28 days.6 In the ALBIOS study, only 7% of patients in both groups were elective surgical patients, with nearly 60% comprising medical ICU admissions. Consistent with clinical practice at the time, a large proportion of patients in both groups also received synthetic colloids.66,67 The 2013 Colloids Versus Crystalloids for the Resuscitation of the Critically Ill (CRISTAL) trial, which was a multinational RCT of 2,857 patients, also found no difference in 28-day mortality with the use of albumin.7 Nevertheless, both the ALBIOS and CRISTAL trials did show some benefit in hemodynamic variables for those patients who had received colloid, including faster weaning of vasopressors and decreased overall vasopressor use, a reduced net fluid balance, and higher sustained mean arterial pressure during the first seven days of ICU admission. A recent synthesis of the evidence from a large systematic review and meta-analysis of 55 RCTs involving over 27,000 ICU patients suggested that colloids, including albumin, improved hemodynamic variables such as mean arterial pressure and cardiac index at lower volumes compared with crystalloids, although this did not translate into improved outcomes.68
The most recent (2018) Cochrane review examining the relative utility of colloids over crystalloids for fluid resuscitation in the critically ill included 69 studies and 30,020 patients. Albumin or frozen plasma (n = 22 studies), as well as starches, dextrans, and gelatins, were compared with crystalloids. The review concluded with “moderate certainty” that the use of colloids in critically ill patients, including albumin or frozen plasma, is unlikely to improve mortality, and that its effects on transfusion requirements are “uncertain.”69 Of note, this 2018 Cochrane review specifically excluded studies of elective surgical patients, including elective cardiac surgical patients. In a similar vein, the latest Surviving Sepsis guidelines issued only a weak recommendation for the use of albumin in patients requiring large volumes of crystalloid resuscitation in septic shock because of a low quality of evidence.70,71
Data outside of the critical care setting in cardiac surgery is limited to small, generally retrospective studies that have yielded conflicting results. Various retrospective reviews have suggested that there is no major outcome difference between the use of colloids or crystalloids in cardiac surgical patients, although there are large cost savings with more restricted albumin use.17,18,72 Fink et al. showed that transitioning from a clinical practice with albumin freely available to a balanced crystalloid-based regimen in postoperative cardiac surgical patients at a quaternary centre resulted in significant cost savings (30,549.20 USD over three months) without significantly impacting patient outcomes.17 A large retrospective database study of 19,578 patients who underwent coronary artery bypass grafting surgery indicated lower all-cause mortality with albumin use compared with nonprotein colloids (OR, 0.80; 95% CI, 0.67 to 0.96).73 In a second, more recent retrospective propensity score matched analysis of 1,095 patients undergoing on-pump cardiac surgery from a United States administrative database including 59 hospitals, patients receiving 5% albumin in the operating room and on postoperative day one had significantly decreased in-hospital mortality (OR, 0.5; 95% CI, 0.4 to 0.9) than those who received crystalloid, as well as lower all-cause 30-day readmission in the albumin group (OR, 0.7; 95% CI, 0.5 to 0.9).44 These large effect sizes are unexpected and appear biologically implausible, and hence may be indicative of residual confounding relating to the underlying indication for which albumin was given, reinforcing the concept that a high-quality prospective study in the cardiac surgery setting is needed.
Based on other retrospective studies, it is possible that albumin use in cardiac surgical patients could be harmful overall. In a retrospective cohort study of 2,594 patients undergoing cardiac surgery at a single Australian centre, Matebele et al. observed an association between perioperative exposure to 4% albumin and increased ICU and hospital length of stay, adjusted healthcare costs, and morbidity, including a higher incidence of “redo” operations for bleeding or tamponade, as well as greater red blood cell transfusion (P < 0.01). Nevertheless, patients who received albumin had a higher severity of illness (as measured by ANZROD and EuroSCORE-1) and were more likely to have had greater severity of postoperative bleeding with an unclear temporal relationship to albumin exposure. There was no difference in adjusted mortality between those who did or did not receive albumin (adjusted OR, 1.24; 95% CI, 0.56 to 2.79; P = 0.6).74
More recent prospective studies in cardiac surgical patients have reported improved clinical outcomes, although sample sizes have generally been small, and a risk of publication bias prevails. The 20% Human Albumin Solution Fluid Bolus Administration Therapy in Patients After Cardiac Surgery (HAS-FLAIR) study was a single-centre, open-label pilot which included 100 consecutive cardiac surgical patients requiring volume resuscitation or improvement in cardiac index in the first 24 postoperative hours.39 The first 50 patients requiring fluid bolus therapy were assigned to crystalloid, and the subsequent 50 patients received up to two treatments of 100 mL of 25% albumin, followed by crystalloid if required. HAS-FLAIR showed volume- and vasopressor-sparing benefits of albumin use in cardiac surgery, including a faster time to cessation of norepinephrine administration and a less positive median [interquartile range] fluid balance (albumin group, 1,100 mL [650–1,960] vs crystalloid group, 1,970 mL [1430–2550]; P = 0.0.39 However, this was a small, non-randomized study, and was not designed to detect differences in clinically important outcomes such as morbidity or mortality. Recent studies in cardiac surgical patients are highlighted and detailed further in Table 3.
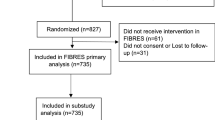
The Albumin in Cardiac Surgery (ALBICS) trial (NCT02560519), which is anticipated to be published soon, is comparing 4% albumin with Ringer’s acetate solution for both CPB prime and volume replacement in cardiac surgery. The primary outcome of this trial is the number of patients with at least one major adverse event during the first postoperative 90 days, including all-cause death, acute myocardial injury, acute heart failure or low output syndrome, resternotomy, stroke, major arrhythmia, major bleeding, infection compromising post-procedural rehabilitation, or AKI. The trial has completed its recruitment target of approximately 1,400 patients from a single academic centre in Finland and closed to recruitment in 2020, and will hopefully shed further light on the role of albumin in the perioperative care of this complex patient group.75
Current controversies
Exogenous albumin for the correction of hypoalbuminemia
Hypoalbuminemia, regardless of underlying pathophysiologic etiology, is an independent predictor of morbidity and poor long-term survival in cardiac surgical patients, major non-cardiac surgical patients, the critically ill, and many other chronic disease states.76,77,78 Prior meta-analyses of cohort studies examining hypoalbuminemia as a predictor of outcomes in the critically ill have found that for each 10 g·L−1 decrease in serum albumin concentration, there is an accompanying 137% increase in the odds of death, an 89% increase in morbidity, and a 71% increase in length of hospital stay.77 Despite this, the administration of exogenous albumin to correct hypoalbuminemia does not appear to improve outcomes in the critical care population, as was shown in numerous large randomized studies.4,6,8,66,79 It is unclear if this is different in cardiac surgical patients. One small, parallel-arm RCT showed that pre-emptive administration of 20% albumin to hypoalbuminemic patients immediately before off-pump coronary artery bypass surgery was associated with a reduced incidence of postoperative AKI (defined using AKI Network [AKIN] criteria) compared with the crystalloid control group (25.7% in the control group vs 13.7% in the treatment group; P = 0.048).80 As a study in off-pump cardiac surgical patients, CPB was minimized as a risk factor. Nevertheless, the crystalloid used in the control group was 0.9% saline, which may be a risk factor for AKI in cardiac surgery patients.81 Additionally, the control group actually received more albumin within 24 hr of CPB than the treatment group did after the surgical insult, which makes the true association of albumin (particularly the timing of administration) with outcomes less clear.80
The role of albumin in the preservation and maintenance of the endothelial glycocalyx
The endothelial glycocalyx is a protein and carbohydrate-rich inner vascular lining that plays a key role in vascular permeability, microvascular tone, prevention of microvascular thrombosis, and cellular adhesion.82 Disturbances of the endovascular glycocalyx precipitated by surgery and CPB are thought to be associated with microcirculatory dysfunction and end-organ complications.53 Significant glycocalyx disturbances, with a resultant potential effect on clinical outcomes, have been documented in various critically ill patient populations.82 There is limited clinical evidence comparing different types of fluids and their effect on the glycocalyx.82,83 Glycocalyx dysfunction is multifactorial in cardiac surgery—resulting from direct tissue injury, systemic inflammation, ischemia-reperfusion injury, oxidative stress, and hypervolemia—and it may persist for days following the original surgery.53 The transcapillary extravascular leak rate of albumin increases within three hours of cardiac surgery, likely because of disruption of the endothelial glycocalyx.31,54,55,84 Therefore, the relative effect of crystalloids and colloids on volume expansion may be determined by the degree of underlying glycocalyx dysfunction. Especially in critically ill cardiac surgical patients, altered glycocalyx permeability may actually result in worsening interstitial edema with colloid administration85 and is unlikely to improve existing interstitial edema.86,87 Preclinical evidence has suggested that albumin not only causes less damage to the glycocalyx but also contributes to its restoration and allows for more favourable microcirculatory perfusion compared with crystalloids.88,89,90,91,92 Nevertheless, these favourable preliminary findings have generally not been replicated in larger clinical studies and/or translated into major advantages in patient outcomes, particularly in cardiac surgical patients.87
Bradykinin-mediated albumin-induced hypotension
Hypotension associated with rapid infusion of albumin products has been recognized since the 1970s.93 This is postulated to be caused by a bradykinin-mediated mechanism, secondary to pre-kallikrein activator (PKA) in the albumin solution. Although believed to be associated with older-generation albumin products containing higher levels of PKA, paradoxical hypotension has been reported with the use of newer-generation 4% albumin for resuscitation in postoperative cardiac surgical patients.94 Such hypotension may be exacerbated in patients taking angiotensin-converting enzyme inhibitors.94 Angiotensin-converting enzyme inhibitors block the conversion of angiotensin-I to angiotensin-II (a potent vasoconstrictor) and block the breakdown of bradykinin (a potent vasodilator).95 Based on the above evidence, consideration may be given to the avoidance or minimization of albumin in patients exposed to renin-angiotensin system inhibitors preoperatively. Nevertheless, this would be rendered difficult given their widespread use in patients presenting for cardiac surgery.96
The association of albumin with hemodilution and coagulopathy
There is some evidence that use of intravenous albumin in cardiac surgery causes greater hemodilution and increased coagulopathy compared with crystalloids, potentially resulting in increased bleeding and blood product transfusion.97,98,99 Albumin may trigger and exacerbate coagulopathy through several mechanisms. Firstly, it may lead to greater hemodilution compared with other fluids, resulting in increased coagulopathic bleeding and need for blood product transfusion.97,98,99 However, the coagulopathy associated with albumin is likely less severe than that produced by synthetic colloids.100,101 Other suggested mechanisms whereby albumin may contribute to coagulopathy include fibrinolysis; inhibition of platelet aggregation through induction of nitric oxide; binding of arachidonic acid, prostacyclin (PGI2), and platelet-activation factor; and a heparin-like activity due to its capacity to bind antithrombin, thereby producing an anti-Xa effect.4,102,103,104
Albumin is known to reduce fibrinogen and coagulation protein levels and prolong laboratory coagulation profiles in patients who undergo plasma exchange.105 A substudy of the SAFE trial confirmed that 4% albumin is associated with a prolonged activated partial thromboplastin time.106 Paar et al. examined the in vitro effect of “low” (mean [SD] 19.3 [7.7] g·L−1), “physiologic” (45.2 [7.8] g·L−1), and “high” (67.5 [18.1] g·L−1) albumin levels on coagulation assays in samples from 25 healthy volunteers.104 Using thromboelastometry, platelet function assays, and thrombin generation assays, these authors reported increased primary hemostasis, increased platelet aggregation, and enhanced clot formation in groups with lower albumin levels than in groups with higher albumin levels. Thrombin generation was not significantly affected. This is in keeping with findings from other viscoelastic testing studies looking at the anticoagulant effects of hemodilution with albumin in clinical (plasma exchange) and experimental settings.105,107
The evidence regarding whether these prolongations of laboratory parameters translate into important bleeding is mixed depending on the clinical context. In a study by Rasmussen et al. in patients undergoing major non-cardiac surgery, albumin was shown to impair platelet activation and to negatively affect clot amplitude and strength, but without any significant difference in the amount of bleeding or need for blood products.108 In a study of patients undergoing plasma exchange, thromboelastographic assessment showed a reduction in clot formation and clot firmness without an increase in bleeding complications.109 In contrast, Shirozu et al. found that preoperative plasma exchange with 5% albumin in patients undergoing living related renal transplantation resulted in similar thromboelastographic derangements but was associated with increased surgical bleeding and prolonged ICU length of stay.110
The association of albumin with perioperative renal injury
The nephrotoxic effects of synthetic colloids have been well documented.111 However, the effects of albumin specifically on renal function are less clear, particularly in cardiac surgery. A recent RCT of 220 hypoalbuminemic cardiac surgical patients undergoing off-pump cardiac bypass grafting found a significantly decreased incidence of AKI within 48 hr in those who underwent albumin replacement perioperatively, although there were some noted sources of bias within the study (Table 3).80
Conversely, in a retrospective single-centre cohort study of 984 on-pump cardiac surgical patients, Frenette et al. found that use of intravenous albumin was associated with a dose-dependent increased risk of AKI.112 This finding persisted after propensity score matching of 141 patients who had received either 5% or 25% albumin with 141 patients who had not received albumin. In this propensity-matched analysis, albumin use was associated with an increased risk of AKI (Risk, Injury, Failure, Loss, and End-stage renal disease [RIFLE] definition) (12% vs 5%; P = 0.03) and AKIN stage 1 events (28% vs 13%; P = 0.002).112 Similarly, in a prospective observational study including 17,742 consecutive patients undergoing cardiac surgery across three centres in Denmark, albumin use compared with crystalloids was associated with adjusted ORs of 2.45 for 30-day mortality (95% CI, 1.21 to 4.96) and 4.84 for new postoperative dialysis (95% CI, 1.91 to 12.2), and adjusted hazard ratios of 1.81 for six-month mortality (95% CI, 1.15 to 2.85) and 1.43 for six-month ischemic events (95% CI, 1.00 to 1.05).113 This signal for an association of albumin use with adverse renal outcomes was not seen in the recent Limiting IV Chloride to Reduce AKI After Cardiac Surgery (LICRA) trial, which was an open-label, prospective study including 1,136 patients undergoing cardiac surgery at a single centre in Australia.114 In this study, there was no significant increase in Kidney Disease: Improving Global Outcomes (KDIGO)-defined stage 2 or 3 AKI across the phases of the perioperative fluid protocol, where both 4% and 20% albumin were used as part of a chloride-limiting strategy.114 Although there was no significant difference in the incidence of AKI, 20% albumin was associated with a significantly lower incidence of hyperchloremia (Table 3).
The tonicity of the albumin solution may also be an important determinant of AKI. Higher concentration albumin solutions contain less chloride than many crystalloid solutions and lower tonicity albumin solutions. There is also significant variability in the chloride concentration of the different commercially available 5% albumin solutions, most of which are hyperchloremic (Table 2).115 This is clinically relevant as there is substantial evidence that supraphysiologic concentrations of chloride result in increased AKI, need for renal replacement therapy, and mortality in surgical and critical care patients.116,117,118,119 In a 2018 trial which randomized 7,942 critically ill patients to either balanced crystalloids or isotonic saline, a greater number of patients in the isotonic saline group had plasma chloride concentrations > 110 mmol·L−1 (35.6% vs 24.5%, P < 0.001) and bicarbonate concentrations < 20 mmol·L−1 (42.1% vs 35.2%; P < 0.001). Correspondingly, the isotonic saline group had a small absolute increase in the risk of death, new renal replacement therapy, or persistent renal dysfunction which may be attributable to hyperchloremic metabolic acidosis, among other factors.120
The mechanism by which hyperchloremia and its related acidosis is associated with adverse outcomes is likely multifactorial.120 Hyperchloremia increases the “strong ion difference,” calculated by adding the plasma sodium, potassium, magnesium and other common positive ion concentrations and subtracting the negative ion concentrations, typically chloride, lactate, and urea.121 The strong ion difference is a major determinant of H+ concentration.122 A decrease in the strong ion difference due to an increase in negative ions such as chloride is associated with metabolic acidosis. Additionally, excess chloride has important effects on renal blood flow and glomerular filtration rate, potentially inducing renal-specific vasoconstriction and reducing glomerular filtration.122 Future RCTs assessing the use of albumin in cardiac surgical patients must carefully account for the variable chloride concentrations found in different albumin formulations, given the independent effect of hyperchloremia on adverse outcomes in the critically ill.120
Conclusion
There is a clear lack of high-quality data to conclusively support the efficacy and safety of albumin over balanced crystalloids for acute volume resuscitation in cardiac surgical patients.26,27,28,29,30,72 This has facilitated ongoing routine administration of albumin without clear evidence of benefit and without a clear understanding of potential harm, particularly in high-risk patient subpopulations undergoing cardiac surgery (such as those with underlying renal dysfunction or heart failure). The associated healthcare expenditures associated with routine albumin administration in the absence of well-defined evidence for its superiority over other fluids are not insignificant.
Results of the ALBICS trial are anticipated soon, and will make an important contribution to the literature.75 Nevertheless, it is likely that this trial will generate as many questions as it answers. ALBICS aims to compare 4% albumin solution with balanced crystalloid, with a primary composite endpoint composed of a broad array of events such as mortality, renal injury, heart failure, stroke, arrythmia, and infection. Based on the current literature, there is limited biological plausibility of albumin having a strong effect on outcomes such as stroke or arrythmia, and ALBICS has relatively low power to detect a difference in more biologically plausible outcomes such as renal injury and days alive outside of ICU. The ALBICS trial had a patient recruitment target of approximately 1,400 patients. Conversely, other trials aiming to detect differences in mortality and renal outcomes in critically ill populations recruited approximately 8,000 patients for adequate power.120 Notably, ALBICS excluded high-risk patients in which clinicians might be significantly more likely to employ albumin, such as patients with very low left ventricular ejection fraction, those with end-stage renal disease, congenital patients, and patients requiring preoperative mechanical ventilation, inotropic support, or mechanical circulatory support. Additionally, the ALBICS trial will not clarify the role of 25% albumin in cardiac surgical patients.
Many questions remain unanswered. Given that the role of RCTs is to provide compelling evidence to change clinical practice, a future trial must include intervention and control arms that reflect how albumin-inclusive resuscitation and albumin-free resuscitation is actually conducted across Canadian cardiac surgical centres, while controlling for differences across albumin formulations (such as chloride content) that could influence outcomes.117 Such a trial would ideally involve at least ten centres across the country to ensure generalizability. As albumin may be preferentially used in higher-risk cardiac surgical patients, such as those with right or left ventricular dysfunction, pre-existing renal disease, and those undergoing complex procedures, such patients should be considered and perhaps even prioritized for study inclusion. Additionally, given the large cost differential between albumin and crystalloids, a well-designed randomized trial showing non-inferiority of balanced crystalloid resuscitation to resuscitation incorporating albumin should provide a compelling rationale to curtail albumin utilization. There is a clear need for well-designed RCTs and higher quality evidence to clarify the role of albumin in cardiac surgical patients, and to better inform clinical practice.
Notes
Roman R. In: Cullum J (Ed.): Medical Services & Hospital Relations, Canadian Blood Services; 2021 (personal communication).
References
Osawa EA, Rhodes A, Landoni G, et al. Effect of perioperative goal-directed hemodynamic resuscitation therapy on outcomes following cardiac surgery: a randomized clinical trial and systematic review. Crit Care Med 2016; 44: 724-33.
Serpa Neto A, Veelo DP, Peireira VG, et al. Fluid resuscitation with hydroxyethyl starches in patients with sepsis is associated with an increased incidence of acute kidney injury and use of renal replacement therapy: a systematic review and meta-analysis of the literature. J Crit Care 2014; 29(185): e1-7.
Levitt DG, Levitt MD. Human serum albumin homeostasis: a new look at the roles of synthesis, catabolism, renal and gastrointestinal excretion, and the clinical value of serum albumin measurements. Int J Gen Med 2016; 9: 229-55.
Vincent JL, Russell JA, Jacob M, et al. Albumin administration in the acutely ill: what is new and where next? Crit Care 2014. DOI: https://doi.org/10.1186/cc13991.
Cook D. Is albumin safe? N Engl J Med 2004; 350: 2294-6.
Caironi P, Tognoni G, Masson S, et al. Albumin replacement in patients with severe sepsis or septic shock. N Engl J Med 2014; 370: 1412-21.
Annane D, Siami S, Jaber S, et al. Effects of fluid resuscitation with colloids vs crystalloids on mortality in critically ill patients presenting with hypovolemic shock: the CRISTAL randomized trial. JAMA 2013; 310: 1809-17.
Finfer S, Bellomo R, Boyce N, et al. A comparison of albumin and saline for fluid resuscitation in the intensive care unit. N Engl J Med 2004; 350: 2247-56.
Task Force on Patient Blood Management for Adult Cardiac Surgery of the European Association for Cardio-Thoracic Surgery (EACTS); European Association of Cardiothoracic Anaesthesiology (EACTA), Boer C, Meesters MI, Milojevic M, et al. 2017 EACTS/EACTA Guidelines on patient blood management for adult cardiac surgery. J Cardiothorac Vasc Anesth 2018; 32: 88-120.
Authors/Task Force Members; Kunst G, Milojevic M, Boer C, et al. 2019 EACTS/EACTA/EBCP Guidelines on cardiopulmonary bypass in adult cardiac surgery. Br J Anaesth 2019; 123: 713-57.
Mutter TC, Ruth CA, Dart AB. Hydroxyethyl starch (HES) versus other fluid therapies: effects on kidney function. Cochrane Database Syst Rev 2013. DOI: https://doi.org/10.1002/14651858.CD007594.pub3.
Baethge C, Goldbeck-Wood S, Mertens S. SANRA—a scale for the quality assessment of narrative review articles. Res Integr Peer Rev 2019; DOI: https://doi.org/10.1186/s41073-019-0064-8.
King WS, Roland K, Selin S, Chipperfield K, Morrison D. Introduction of guidelines for the use of albumin and the effect on albumin prescribing practices in British Columbia. BC Med J 2012; 54: 34-8.
Clarke G, Yan M. Clinical Guide to Transfusion: Albumin 2018 [cited July 29, 2020 2020]. Available from URL: https://professionaleducation.blood.ca/en/transfusion/guide-clinique/albumin (accessed March 2021).
Aronson S, Nisbet P, Bunke M. Fluid resuscitation practices in cardiac surgery patients in the USA: a survey of health care providers. Perioper Med (Lond) 2017; DOI: https://doi.org/10.1186/s13741-017-0071-6.
Protsyk V, Rasmussen BS, Guarracino F, Erb J, Turton E, Ender J. Fluid management in cardiac surgery: results of a survey in European cardiac anesthesia departments. J Cardiothorac Vasc Anesth 2017; 31: 1624-9.
Fink RJ, Young A, Yanez ND, et al. Cohort study of albumin versus lactated Ringer’s for postoperative cardiac surgery fluid resuscitation in the intensive care unit. Pharmacotherapy 2018; 38: 1241-9.
Rabin J, Meyenburg T, Lowery AV, Rouse M, Gammie JS, Herr D. Restricted albumin utilization is safe and cost effective in a cardiac surgery intensive care unit. Ann Thorac Surg 2017; 104: 42-8.
Roberts I, Blackhall K, Alderson P, Bunn F, Schierhout G. Human albumin solution for resuscitation and volume expansion in critically ill patients. Cochrane Database Syst Rev 2011; DOI: https://doi.org/10.1002/14651858.CD001208.pub4.
Doussau A, Perez P, Puntous M, et al. Fresh-frozen plasma transfusion did not reduce 30-day mortality in patients undergoing cardiopulmonary bypass cardiac surgery with excessive bleeding: the PLASMACARD multicenter cohort study. Transfusion 2014; 54: 1114-24.
Casbard AC, Williamson LM, Murphy MF, Rege K, Johnson T. The role of prophylactic fresh frozen plasma in decreasing blood loss and correcting coagulopathy in cardiac surgery. A systematic review. Anaesthesia 2004; 59: 550-8.
Dieu A, Rosal Martins M, Eeckhoudt S, et al. Fresh frozen plasma versus crystalloid priming of cardiopulmonary bypass circuit in pediatric surgery: a randomized clinical trial. Anesthesiology 2020; 132: 95-106.
Zarychanski R, Abou-Setta AM, Turgeon AF, et al. Association of hydroxyethyl starch administration with mortality and acute kidney injury in critically ill patients requiring volume resuscitation: a systematic review and meta-analysis. JAMA 2013; 309: 678-88.
He B, Xu B, Xu X, et al. Hydroxyethyl starch versus other fluids for non-septic patients in the intensive care unit: a meta-analysis of randomized controlled trials. Crit Care 2015; DOI: https://doi.org/10.1186/s13054-015-0833-9.
Bagshaw SM, Chawla LS. Hydroxyethyl starch for fluid resuscitation in critically ill patients. Can J Anesth 2013; 60: 709-13.
Bunn F, Trivedi D, Ashraf S. Colloid solutions for fluid resuscitation. Cochrane Database Syst Rev 2011; DOI: https://doi.org/10.1002/14651858.CD001319.pub3.
Jacob M, Chappell D, Conzen P, Wilkes MM, Becker BF, Rehm M. Small-volume resuscitation with hyperoncotic albumin: a systematic review of randomized clinical trials. Crit Care 2008; DOI: https://doi.org/10.1186/cc6812.
Perel P, Roberts I, Ker K. Colloids versus crystalloids for fluid resuscitation in critically ill patients. Cochrane Database Syst Rev 2013; DOI: https://doi.org/10.1002/14651858.CD000567.pub6.
Roberts I, Blackhall K, Alderson P, Bunn F, Schierhout G. Human albumin solution for resuscitation and volume expansion in critically ill patients. Cochrane Database Syst Rev 2011; DOI: https://doi.org/10.1002/14651858.CD001208.pub4.
Patel A, Laffan MA, Waheed U, Brett SJ. Randomised trials of human albumin for adults with sepsis: systematic review and meta-analysis with trial sequential analysis of all-cause mortality. BMJ 2014; DOI: https://doi.org/10.1136/bmj.g4561.
Romagnoli S, Rizza A, Ricci Z. Fluid status assessment and management during the perioperative phase in adult cardiac surgery patients. J Cardiothorac Vasc Anesth 2016; 30: 1076-84.
Arulkumaran N, Corredor C, Hamilton MA, et al. Cardiac complications associated with goal-directed therapy in high-risk surgical patients: a meta-analysis. Br J Anaesth 2014; 112: 648-59.
Aya HD, Cecconi M, Hamilton M, Rhodes A. Goal-directed therapy in cardiac surgery: a systematic review and meta-analysis. Br J Anaesth 2013; 110: 510-7.
Reddy S, McGuinness S, Parke R, Young P. Choice of fluid therapy and bleeding risk after cardiac surgery. J Cardiothorac Vasc Anesth 2016; 30: 1094-103.
Parke RL, McGuinness SP, Gilder E, McCarthy LW. Intravenous fluid use after cardiac surgery: a multicentre, prospective, observational study. Crit Care Resusc 2014; 16: 164-9.
Woodcock TE, Woodcock TM. Revised Starling equation and the glycocalyx model of transvascular fluid exchange: an improved paradigm for prescribing intravenous fluid therapy. Br J Anaesth 2012; 108: 384-94.
Pesonen E, Passov A, Andersson S, et al. Glycocalyx degradation and inflammation in cardiac surgery. J Cardiothorac Vasc Anesth 2019; 33: 341-5.
Moret E, Jacob MW, Ranucci M, Schramko AA. Albumin-beyond fluid replacement in cardiopulmonary bypass surgery: why, how, and when? Semin Cardiothorac Vasc Anesth 2014; 18: 252-9.
Wigmore GJ, Anstey JR, St John A, et al. 20% Human albumin solution fluid bolus administration therapy in patients after cardiac surgery (the HAS FLAIR Study). J Cardiothorac Vasc Anesth 2019; 33: 2920-7.
Mwaura L, Vuylsteke A. Fueling the debate on albumin after cardiac surgery. J Cardiothorac Vasc Anesth 2019; 33: 2928-9.
Curtis S, Anwar S. Fluid resuscitation after cardiac surgery: the quest for the ideal fluid. J Cardiothorac Vasc Anesth 2019; DOI: https://doi.org/10.1053/j.jvca.2019.06.023.
Taverna M, Marie AL, Mira JP, Guidet B. Specific antioxidant properties of human serum albumin. Ann Intensive Care 2013; DOI: https://doi.org/10.1186/2110-5820-3-4.
Kamra C, Beney A. Human albumin in extracorporeal prime: effect on platelet function and bleeding. Perfusion 2013; 28: 536-40.
Kingeter AJ, Raghunathan K, Munson SH, et al. Association between albumin administration and survival in cardiac surgery: a retrospective cohort study. Can J Anesth 2018; 65: 1218-27.
Vincent JL, Pelosi P, Pearse R, et al. Perioperative cardiovascular monitoring of high-risk patients: a consensus of 12. Crit Care 2015; DOI: https://doi.org/10.1186/s13054-015-0932-7.
Shim HJ, Jang JY, Lee SH, Lee JG. The effect of positive balance on the outcomes of critically ill noncardiac postsurgical patients: a retrospective cohort study. J Crit Care 2014; 29: 43-8.
Li C, Wang H, Liu N, et al. Early negative fluid balance is associated with lower mortality after cardiovascular surgery. Perfusion 2018; 33: 630-7.
Pradeep A, Rajagopalam S, Kolli HK, et al. High volumes of intravenous fluid during cardiac surgery are associated with increased mortality. HSR Proc Intensive Care Cardiovasc Anesth 2010; 2: 287-96.
Kuo G, Chen SW, Lee CC, et al. Latent trajectories of fluid balance are associated with outcomes in cardiac and aortic surgery. Ann Thorac Surg 2020; 109: 1343-9.
Mitra S, Khandelwal P. Are all colloids same? How to select the right colloid? Indian J Anaesth 2009; 53: 592-607.
Martin C, Cortegiani A, Gregoretti C, et al. Choice of fluids in critically ill patients. BMC Anesthesiol 2018; DOI: https://doi.org/10.1186/s12871-018-0669-3.
Finfer S, Bellomo R, Boyce N. A comparison of albumin and saline for fluid resuscitation in the intensive care unit. N Engl J Med 2004; 350: 2247-56.
Dekker NA, Veerhoek D, Koning NJ, et al. Postoperative microcirculatory perfusion and endothelial glycocalyx shedding following cardiac surgery with cardiopulmonary bypass. Anaesthesia 2019; 74: 609-18.
Bruegger D, Rehm M, Abicht J, et al. Shedding of the endothelial glycocalyx during cardiac surgery: on-pump versus off-pump coronary artery bypass graft surgery. J Thorac Cardiovasc Surg 2009; 138: 1445-7.
Sheward V, Tibby S, Bangalore H, Durward A, Murdoch I. Endothelial glycocalyx disruption after cardiac surgery in infants. Crit Care 2011; DOI: https://doi.org/10.1186/cc9502.
Hoeft A, Korb H, Mehlhorn U, Stephan H, Sonntag H. Priming of cardiopulmonary bypass with human albumin or Ringer lactate: effect on colloid osmotic pressure and extravascular lung water. Br J Anaesth 1991; 66: 73-80.
Russell JA, Navickis RJ, Wilkes MM. Albumin versus crystalloid for pump priming in cardiac surgery: meta-analysis of controlled trials. J Cardiothorac Vasc Anesth 2004; 18: 429-37.
Sade RM, Stroud MR, Crawford FA Jr, Kratz JM, Dearing JP, Bartles DM. A prospective randomized study of hydroxyethyl starch, albumin, and lactated Ringer’s solution as priming fluid for cardiopulmonary bypass. J Thorac Cardiovasc Surg 1985; 89: 713-22.
Kuitunen AH, Hynynen MJ, Vahtera E, Salmenpera MT. Hydroxyethyl starch as a priming solution for cardiopulmonary bypass impairs hemostasis after cardiac surgery. Anesth Analg 2004; 98: 291-7.
Weiler P, Hamiko M, Mellert F, et al. Impact of crystalloid or albumin priming of the heart-lung machine on inhospital outcome after coronary artery bypass surgery. Thorac Cardiovasc Surg 2019; 67: 475-83.
Vandewiele K, Bove T, De Somer FM, et al. The effect of retrograde autologous priming volume on haemodilution and transfusion requirements during cardiac surgery. Interact Cardiovasc Thorac Surg 2013; 16: 778-83.
Sun P, Ji B, Sun Y, et al. Effects of retrograde autologous priming on blood transfusion and clinical outcomes in adults: a meta-analysis. Perfusion 2013; 28: 238-43.
Cochrane Injuries Group Albumin Reviewers. Human albumin administration in critically ill patients: systematic review of randomised controlled trials. BMJ 1998; 317: 235-40.
Roberts I, Edwards P, McLelland B. More on albumin. Use of human albumin in UK fell substantially when systematic review was published. BMJ 1999; 318: 1214-5.
The SAFE Study Investigators. Impact of albumin compared to saline on organ function and mortality of patients with severe sepsis. Intensive Care Med 2011; 37: 86-96.
Charpentier J, Mira JP. EARSS Study Group: Efficacy and tolerance of hyperoncotic albumin administration in septic shock patients: The EARSS study [abstract]. Intensive Care Med 2011; 37(Suppl 1): S115-0438.
Caironi P, Tognoni G, Masson S, et al. Albumin replacement in patients with severe sepsis or septic shock. N Engl J Med 2014; 370: 1412-21.
Martin GS, Bassett P. Crystalloids vs. colloids for fluid resuscitation in the intensive care unit: a systematic review and meta-analysis. J Crit Care 2019; 50: 144-54.
Lewis SR, Pritchard MW, Evans DJ, et al. Colloids versus crystalloids for fluid resuscitation in critically ill people. Cochrane Database Syst Rev 2018; DOI: https://doi.org/10.1002/14651858.CD000567.pub7.
Rhodes A, Evans LE, Alhazzani W, et al. Surviving sepsis campaign: international guidelines for management of sepsis and septic shock: 2016. Intensive Care Med 2017; 43: 304-77.
Levy MM, Evans LE, Rhodes A. The surviving sepsis campaign bundle: 2018 update. Intensive Care Med 2018; 44: 925-8.
Lange M, Ertmer C, Van Aken H, Westphal M. Intravascular volume therapy with colloids in cardiac surgery. J Cardiothorac Vasc Anesth 2011; 25: 847-55.
Sedrakyan A, Gondek K, Paltiel D, Elefteriades JA. Volume expansion with albumin decreases mortality after coronary artery bypass graft surgery. Chest 2003; 123: 1853-7.
Matebele MP, Ramanan M, Thompson K, Cornmell G, Naidoo RV, Shekar K. Albumin use after cardiac surgery. Crit Care Explor 2020; DOI: https://doi.org/10.1097/CCE.0000000000000164.
Vlasov H, Juvonen T, Hiippala S, et al. Effect and safety of 4% albumin in the treatment of cardiac surgery patients: study protocol for the randomized, double-blind, clinical ALBICS (ALBumin In Cardiac Surgery) trial. Trials 2020; DOI: https://doi.org/10.1186/s13063-020-4160-3.
de la Cruz KI, Bakaeen FG, Wang XL, et al. Hypoalbuminemia and long-term survival after coronary artery bypass: a propensity score analysis. Ann Thorac Surg 2011; 91: 671-5.
Vincent JL, Dubois MJ, Navickis RJ, Wilkes MM. Hypoalbuminemia in acute illness: is there a rationale for intervention? A meta-analysis of cohort studies and controlled trials. Ann Surg 2003; 237: 319-34.
Meyer CP, Rios-Diaz AJ, Dalela D, et al. The association of hypoalbuminemia with early perioperative outcomes - a comprehensive assessment across 16 major procedures. Am J Surg 2017; 214: 871-83.
Safe Study Investigators; Finfer S, Bellomo R, McEvoy S, et al. Effect of baseline serum albumin concentration on outcome of resuscitation with albumin or saline in patients in intensive care units: analysis of data from the saline versus albumin fluid evaluation (SAFE) study. BMJ 2006; https://doi.org/10.1136/bmj.38985.398704.7c.
Lee EH, Kim WJ, Kim JY, et al. Effect of exogenous albumin on the incidence of postoperative acute kidney injury in patients undergoing off-pump coronary artery bypass surgery with a preoperative albumin level of less than 4.0 g/dl. Anesthesiology 2016; 124: 1001-11.
Kim JY, Joung KW, Kim KM, et al. Relationship between a perioperative intravenous fluid administration strategy and acute kidney injury following off-pump coronary artery bypass surgery: an observational study. Crit Care 2015; DOI: https://doi.org/10.1186/s13054-015-1065-8.
Uchimido R, Schmidt EP, Shapiro NI. The glycocalyx: a novel diagnostic and therapeutic target in sepsis. Crit Care 2019; DOI: https://doi.org/10.1186/s13054-018-2292-6.
Aldecoa C, Llau JV, Nuvials X, Artigas A. Role of albumin in the preservation of endothelial glycocalyx integrity and the microcirculation: a review. Ann Intensive Care 2020; DOI: https://doi.org/10.1186/s13613-020-00697-1.
Magoon R, Makhija N. Endothelial glycocalyx and cardiac surgery: newer insights. J Cardiothorac Vasc Anesth 2020; 34: 310-1.
Jacob M, Bruegger D, Rehm M, et al. The endothelial glycocalyx affords compatibility of Starling’s principle and high cardiac interstitial albumin levels. Cardiovasc Res 2007; 73: 575-86.
van der Heijden M, Verheij J, van Nieuw Amerongen GP, Groeneveld AB. Crystalloid or colloid fluid loading and pulmonary permeability, edema, and injury in septic and nonseptic critically ill patients with hypovolemia. Crit Care Med 2009; 37: 1275-81.
Milford EM, Reade MC. Resuscitation fluid choices to preserve the endothelial glycocalyx. Crit Care 2019; DOI: https://doi.org/10.1186/s13054-019-2369-x.
Jacob M, Bruegger D, Rehm M, Welsch U, Conzen P, Becker BF. Contrasting effects of colloid and crystalloid resuscitation fluids on cardiac vascular permeability. Anesthesiology 2006; 104: 1223-31.
Torres Filho IP, Torres LN, Salgado C, Dubick MA. Plasma syndecan-1 and heparan sulfate correlate with microvascular glycocalyx degradation in hemorrhaged rats after different resuscitation fluids. Am J Physiol Heart Circ Physiol 2016; 310: H1468-78.
Zausig YA, Chappell D, Becker BF, et al. The impact of crystalloidal and colloidal infusion preparations on coronary vascular integrity, interstitial oedema and cardiac performance in isolated hearts. Crit Care 2013; DOI: https://doi.org/10.1186/cc12898.
Naumann DN, Beaven A, Dretzke J, Hutchings S, Midwinter MJ. Searching for the optimal fluid to restore microcirculatory flow dynamics after haemorrhagic shock: a systematic review of preclinical studies. Shock 2016; 46: 609-22.
Boer C, Bossers SM, Koning NJ. Choice of fluid type: physiological concepts and perioperative indications. Br J Anaesth 2018; 120: 384-96.
Harrison GA, Robinson M, Stacey RV, McCulloch CH, Torda TA, Wright JS. Hypotensive effects of stable plasma protein solution (SPPS): a preliminary communication. Med J Aust 1971; 2: 1040-1.
Howard G, Downward G, Bowie D. Human serum albumin induced hypotension in the postoperative phase of cardiac surgery. Anaesth Intensive Care 2001; 29: 591-4.
Brown NJ, Vaughan DE. Angiotensin-converting enzyme inhibitors. Circulation 1998; 97: 1411-20.
Ding Q, Zhang Z, Liu H, et al. Perioperative use of renin-angiotensin system inhibitors and outcomes in patients undergoing cardiac surgery. Nat Commun 2019; DOI: https://doi.org/10.1038/s41467-019-11678-9.
Skhirtladze K, Base EM, Lassnigg A, et al. Comparison of the effects of albumin 5%, hydroxyethyl starch 130/0.4 6%, and Ringer’s lactate on blood loss and coagulation after cardiac surgery. Br J Anaesth 2014; 112: 255-64.
Jacob M, Fellahi JL, Chappell D, Kurz A. The impact of hydroxyethyl starches in cardiac surgery: a meta-analysis. Crit Care 2014; DOI: https://doi.org/10.1186/s13054-014-0656-0.
Rasmussen KC, Secher NH, Pedersen T. Effect of perioperative crystalloid or colloid fluid therapy on hemorrhage, coagulation competence, and outcome: a systematic review and stratified meta-analysis. Medicine (Baltimore) 2016; DOI: https://doi.org/10.1097/MD.0000000000004498.
Winstedt D, Hanna J, Schott U. Albumin-induced coagulopathy is less severe and more effectively reversed with fibrinogen concentrate than is synthetic colloid-induced coagulopathy. Scand J Clin Lab Invest 2013; 73: 161-9.
Kozek-Langenecker SA. Fluids and coagulation. Curr Opin Crit Care 2015; 21: 285-91.
Joorgensen KA, Stoffersen E. Heparin like activity of albumin. Thromb Res 1979; 16: 569-74.
Jorgensen KA, Stoffersen E. On the inhibitory effect of albumin on platelet aggregation. Thromb Res 1980; 17: 13-8.
Paar M, Rossmann C, Nusshold C, et al. Anticoagulant action of low, physiologic, and high albumin levels in whole blood. PLoS One 2017; DOI: https://doi.org/10.1371/journal.pone.0182997.
Tholking G, Mesters R, Dittrich R, Pavenstadt H, Kumpers P, Reuter S. Assessment of hemostasis after plasma exchange using rotational thrombelastometry (ROTEM). PLoS One 2015; DOI: https://doi.org/10.1371/journal.pone.0130402.
Bellomo R, Morimatsu H, Presneill J, et al. Effects of saline or albumin resuscitation on standard coagulation tests. Crit Care Resusc 2009; 11: 250-6.
Pathirana S, Wong G, Williams P, et al. The effects of haemodilution with albumin on coagulation in vitro as assessed by rotational thromboelastometry. Anaesth Intensive Care 2015; 43: 187-92.
Rasmussen KC, Hojskov M, Johansson PI, et al. Impact of albumin on coagulation competence and hemorrhage during major surgery: a randomized controlled Trial. Medicine (Baltimore) 2016; DOI: https://doi.org/10.1097/MD.0000000000002720.
Blasi A, Cid J, Beltran J, Taura P, Balust J, Lozano M. Coagulation profile after plasma exchange using albumin as a replacement solution measured by thromboelastometry. Vox Sang 2016; 110: 159-65.
Shirozu K, Fujimura N, Karashima Y, et al. Effects of preoperative plasma exchange therapy with albumin replacement fluid on blood coagulation in patients undergoing ABO-incompatible living-donor kidney transplantation using rotational thromboelastometry. BMC Anesthesiol 2018; DOI: https://doi.org/10.1186/s12871-018-0536-2.
Reinhart K, Perner A, Sprung CL, et al. Consensus statement of the ESICM task force on colloid volume therapy in critically ill patients. Intensive Care Med 2012; 38: 368-83.
Frenette AJ, Bouchard J, Bernier P, et al. Albumin administration is associated with acute kidney injury in cardiac surgery: a propensity score analysis. Crit Care 2014; DOI: https://doi.org/10.1186/s13054-014-0602-1.
Ryhammer PK, Tang M, Hoffmann-Petersen J, et al. Colloids in cardiac surgery-friend or foe? J Cardiothorac Vasc Anesth 2017; 31: 1639-48.
McIlroy D, Murphy D, Kasza J, Bhatia D, Wutzlhofer L, Marasco S. Effects of restricting perioperative use of intravenous chloride on kidney injury in patients undergoing cardiac surgery: the LICRA pragmatic controlled clinical trial. Intensive Care Med 2017; 43: 795-806.
Lai AT, Zeller MP, Millen T, et al. Chloride and other electrolyte concentrations in commonly available 5% albumin products. Crit Care Med 2018; 46: e326-9.
Krajewski ML, Raghunathan K, Paluszkiewicz SM, Schermer CR, Shaw AD. Meta-analysis of high- versus low-chloride content in perioperative and critical care fluid resuscitation. Br J Surg 2015; 102: 24-36.
Yunos NM, Bellomo R, Hegarty C, Story D, Ho L, Bailey M. Association between a chloride-liberal vs chloride-restrictive intravenous fluid administration strategy and kidney injury in critically ill adults. JAMA 2012; 308: 1566-72.
Yunos NM, Bellomo R, Glassford N, Sutcliffe H, Lam Q, Bailey M. Chloride-liberal vs. chloride-restrictive intravenous fluid administration and acute kidney injury: an extended analysis. Intensive Care Med 2015; 41: 257-64.
McCluskey SA, Karkouti K, Wijeysundera D, Minkovich L, Tait G, Beattie WS. Hyperchloremia after noncardiac surgery is independently associated with increased morbidity and mortality: a propensity-matched cohort study. Anesth Analg 2013; 117: 412-21.
Semler MW, Self WH, Wanderer JP, et al. Balanced crystalloids versus saline in critically ill adults. N Engl J Med 2018; 378: 829-39.
Lee YS. Clinical significance of strong ion gap: between ICU and hemodialysis patients with metabolic acidosis. Electrolyte Blood Press 2007; 5: 1-8.
McCluskey SA, Bartoszko J. The chloride horse and normal saline cart: the association of crystalloid choice with acid base status and patient outcomes in kidney transplant recipients. Can J Anesth 2020; 67: 403-7.
Aronson S, Nisbet P, Bunke M. Fluid resuscitation practices in cardiac surgery patients in the USA: a survey of health care providers. Perioper Med (Lond) 2017; DOI: https://doi.org/10.1186/s13741-017-0071-6.
PRODUCT MONOGRAPH PLASBUMIN®-5. Grifols Therapeutics LLC; 2018. Available from URL: https://www.grifols.com/documents/17006/133313/Plasbumin-5-en.pdf/ab42326e-cfac-4a43-87df-d74b069fe06a (accessed March 2021).
PRODUCT MONOGRAPH PLASBUMIN®-25. Grifols Therapeutics LLC; 2018. Available from URL: https://www.grifols.com/documents/17006/133313/Plasbumin-25-en.pdf/75af1bb0-76c7-4af9-8cf6-583d69b23c36 (accessed March 2021).
PRODUCT MONOGRAPH Alburex 5 and Alburex 25. CSL Behring LLC; 2016. Available from URL: https://labeling.cslbehring.ca/PM/CA/Alburex/EN/Alburex-Product-Monograph.pdf (accessed March 2021).
Author contributions
All authors supported manuscript conception, content, and writing, and review of the final paper.
Disclosures
None.
Funding statement
Keyvan Karkouti, MD, MSc is in part supported by a merit award from the Department of Anesthesia and Pain Medicine, University of Toronto; and has received research support, honoraria, or consultancy for speaking engagements from Octapharma, Instrumentation Laboratory, and Bayer. Jeannie Callum, MD has received research support from CSL Behring, Octapharma, and Canadian Blood Services.
Editorial responsibility
This submission was handled by Dr. Stephan K.W. Schwarz, Editor-in-Chief, Canadian Journal of Anesthesia/Journal canadien d’anesthésie.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Hanley, C., Callum, J., Karkouti, K. et al. Albumin in adult cardiac surgery: a narrative review. Can J Anesth/J Can Anesth 68, 1197–1213 (2021). https://doi.org/10.1007/s12630-021-01991-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12630-021-01991-7