Abstract
Purpose
Rapid response systems (RRSs) have been introduced into hospitals to help reduce the incidence of sudden cardiopulmonary arrest (CPA). This study evaluated whether an RRS reduces the incidence of in-hospital postoperative CPA.
Methods
This retrospective before-and-after analysis evaluated data collected from electronic medical records during a pre-intervention (January 2008 to September 2012) and post-intervention (implementation of an RRS) interval (October 2012 to December 2016) at a single tertiary care institution. The primary outcome was a change in the rate of CPA in surgical patients recovering in a general ward. A Poisson regression analysis adjusted for the Charlson Comorbidity Index (CCI) was used to compare CPA rates during these two intervals.
Results
Of the 207,054 surgical procedures performed during the study period, mean (95% confidence interval [CI]) CPA events per 10,000 cases of 7.46 (5.72 to 9.19) and 5.19 (3.85 to 6.52) were recorded before and after RRS intervention, respectively (relative risk [RR], 0.73; 97.5% CI, 0.48 to 1.13; P = 0.103). Cardiopulmonary arrest incidence was reduced during RRS operational hours of 07:00–22:00 Monday-Friday and 07:00–12:00 Saturday (RR, 0.56; 97.5% CI, 0.31 to 1.02; P = 0.027) but was unchanged when the RRS was not operational (RR, 0.86; 97.5% CI, 0.52 to 1.40; P = 0.534). The CCI-adjusted RR of CPA after RRS implementation was lower than before RRS intervention (0.63; 97.5% CI, 0.41 to 0.98; P = 0.018) but this reduction was still only apparent during RRS operational hours (RR, 0.48; 97.5% CI, 0.27 to 0.89; P = 0.008 vs RR, 0.85; 97.5% CI, 0.45 to 1.58; P = 0.55).
Conclusion
Implementation of an RRS reduced the incidence of postoperative CPA in patients recovering in a general ward. Furthermore, this reduction was observed only during RRS operational hours.
Résumé
Objectif
Les systèmes de réponse rapide (SRR) ont été introduits dans les hôpitaux pour contribuer à diminuer l’incidence des arrêts cardiorespiratoires (ACR) subits. Cette étude a évalué si un SRR réduit l’incidence des ACR postopératoires à l’hôpital.
Méthodes
Cette analyse rétrospective d’impact a évalué les données collectées à partir des dossiers médicaux électroniques au cours d’une période pré-intervention (janvier 2008 à septembre 2012) et d’une période post-intervention (mise en place d’un RRS : octobre 2012 à décembre 2016) dans un seul établissement de soins tertiaires. Le critère d’évaluation principal était la modification du taux d’ACR chez les patients chirurgicaux en post-opératoire dans une unité de chirurgie générale. Une analyse de régression de Poisson ajustée pour l’indice de comorbidités de Charlson (CCI) a été utilisée pour comparer les taux d’ACR pendant ces deux périodes.
Résultats
Sur les 207 054 procédures chirurgicales pratiquées au cours de l’étude, le nombre moyen d’événements d’ACR (intervalle de confiance [IC] à 95 %]) par 10 000 cas enregistrés, respectivement avant et après la mise en place du SRR, était de 7,46 (5,72 à 9,19) et 5,19 (3,85 à 6,52) avec un risque relatif [RR] : 0,73; IC à 97,5 % : 0,48 à 1,13; P = 0,103). L’incidence des arrêts cardiorespiratoires a diminué pendant les heures d’activité du SRR de 7 h à 22 h du lundi au vendredi et de 7 h à midi le samedi (RR : 0,56; IC à 97,5 % : 0,31 à 1,02; P = 0,027), mais elle est restée inchangée quand le SRR n’était pas opérationnel (RR : 0,86; IC à 97,5 % : 0,52 à 1,40; P = 0,534). Le RR d’ACR ajusté pour le CCI après la mise en place du SRR a été inférieur à ce qu’il était avant l’intervention (0,63; IC à 97,5 % : 0,41 à 0,98; P = 0,018), mais cette réduction n’était détectable que pendant les heures d’activité du SRR (RR : 0,48; IC à 97,5 % : 0,27 à 0,89; P = 0,008 contre RR : 0,85; IC à 97,5 % : 0,45 à 1,58; P = 0,55).
Conclusion
La mise en œuvre d’un SRR a diminué l’incidence des ACR postopératoires chez les patients récupérant dans un service de chirurgie générale. En outre, cette réduction n’a été observée que pendant les heures d’activité du SRR.
Similar content being viewed by others
Hospitalized patients may experience sudden cardiopulmonary arrest (CPA) at any time,1 and approximately 60–84% of cases exhibit pre-arrest alarms (i.e., abnormal clinical signs/test results).2,3 Therefore, in-hospital systems that respond rapidly to these alarms (rapid response systems, RRSs) have been introduced with the goal of reducing the incidence of sudden CPA.4,5 By design, patients with pre-arrest alarms detected by the RRS receive immediate and appropriate interventions, including medical treatment and/or transfer to an intensive care unit (ICU). The RRS alert may also provide an opportunity to assess end-of-life planning, including the aggressiveness of resuscitation efforts. Although the effectiveness of RRSs remains controversial,6 these systems are being used with increasing frequency.7
Although considerable efforts have been made to assess the benefit associated with implementation of evidence-based surgical pathways,8 relatively little information is available regarding the benefits of implementing an RRS for postoperative surgical patients recovering in a general hospital ward. One prospective study suggests that medical emergency teams may improve postoperative mortality and morbidity rates,9 but it did not consider the incidence of CPA. We previously showed that the RRS established at the Seoul National University Bundang Hospital (SNUBH) was associated with a reduction in CPA in hospitalized patients.10 The purpose of the present study was to assess whether the implementation of the RRS at our institution was associated with a reduced incidence of postoperative CPA in patients recovering in a general ward.
Methods
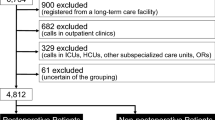
This study protocol was approved by the institutional review board of SNUBH (B-1703-388-106). The RRS was established at our hospital in October 2012, with active periods of 07:00–22:00 on weekdays and 07:00–12:00 on Saturdays. The pre-intervention period (pre-RRS) of 57 months was from October 2008 to September 2012, and the post-intervention period (post-RRS) of 51 months was from October 2012 to December 2016. Cardiopulmonary arrest-related data were collected from the electronic medical records of surgical patients treated during the study periods. The inclusion criteria were adult surgical patients (age ≥18 yr) requiring general or regional anesthesia. Surgical patients were excluded if their CPA occurred in the ICU, emergency department, operating room, procedure room, or outpatient clinic. Nevertheless, patients were included if the CPA occurred after transfer from the ICU to the general ward. Additionally, patients experiencing CPA during the terminal stages of a fatal disease with “do-not-resuscitate” orders were excluded.
The SNUBH and RRS
The SNUBH is a 1,360-bed tertiary care hospital and teaching centre. The RRS uses screening criteria for ten parameters11 (systolic blood pressure, heart rate, respiratory rate, body temperature, oxygen saturation, pH, partial pressure of carbon dioxide (PaCO2), partial pressure of oxygen, lactic acid, and total CO2 – Appendix 1) which are collected using the BESTboard® (Seongnam-si, Republic of Korea), an electronic medical record screening dashboard system developed by SNUBH and Ezcaretech (Appendix 2).12 Vital signs and laboratory values are automatically refreshed on the BESTboard® every five minutes or by a manual click of the update button by a user. Typically, vital signs are recorded every several hours but higher-risk patients may be monitored more frequently.
One of four experienced nurses is dedicated to using this system, which continuously monitors patients in all wards, and one of 12 multi-disciplinary critical care specialists (e.g., internal medicine, anesthesiology, emergency medicine, and thoracic surgery) is immediately notified if a patient develops ≥ one alarm sign. In parallel, the critical care physicians also provide clinical care in their respective ICUs (surgical, emergency, medical, and neurologic ICUs). The RRS nurses are alerted by automatic alarms from the BESTboard® or by direct telephone calls from nurses and attending doctors.
After examining the identified patient and/or reviewing their medical chart, the RRS nurse then notifies the on-duty RRS critical care specialist who in turn formulates a treatment plan that may include patient transfer to the ICU. This process typically takes place within 30 min (Fig. 1).
Schematic flow of the rapid response system. The central monitoring computer program (BESTboard®) filters vital sign data and laboratory values from the electronic medical records. A pop-up window and alarm (beeping sound) automatically notify the RRT nurse (see Appendices 1 and 2). Ward nurses and physicians can also contact the RRT nurse directly by telephone. Once contacted, the RRT nurse immediately evaluates the identified patient to assess the risk level. As appropriate, the RRT nurse then contacts the RRT physician. ICU = intensive care unit; RRT = rapid response team
Data collection and outcomes
The primary outcome of interest was the rate of CPA in postoperative patients recovering in a general ward during the pre-RRS (January 2008–September 2012) compared with the post-RRS interval (October 2012–December 2016). As CPA was a relatively infrequent event, we calculated the CPA incidence per 10,000 sequential surgical procedures. Furthermore, we compared the rate of CPA during RRS operational and non-operational hours during the two study intervals. The following medical record data for all patients included in this study were collected from the electronic medical chart (BESTCare®; SNUBH and Ezcaretech, Seongnam-si, Republic of Korea): age, height, weight, American Society of Anesthesiologists (ASA) class, type of surgery, ratio of ward patients to nurses and to physicians, and any alarms signaled by the RRS during the postoperative period.12 The Charlson Comorbidity Index (CCI) for each patient was calculated by a Medical Informatics Team technician and two critical care specialists who were blinded to patient grouping (pre- vs post-implementation of the RRS).13 The date and time of the CPAs were tracked, and any alarm signs within 24 hr of the event were evaluated, as these may be correlated with the occurrence of CPA.14
Statistical analysis
Data were analyzed using R software (version 3.3.2, R Development Core Team, Vienna, Austria). Continuous data are presented as means (standard deviation), and categorical data are presented as numbers and percentages. Differences between the pre-RRS and post-RRS periods were assessed using the independent t test (normally distributed data), Wilcoxon signed-rank test (non-normally distributed data), Chi-square test (categorical variables), or Fisher’s exact test (rare events). The relative risk (RR) of CPA incidence (ratio of the proportions of CPA during the pre-RRS and post-RRS periods) and 97.5% confidence interval (CI) were evaluated following a Bonferroni correction.
Finally, we compared the patients (pre- vs post- RRS implementation) regarding age, sex, CCI, ASA class, and emergency vs elective surgery status during the periods of interest and estimated the CCI-adjusted relative risk of CPAs using a Poisson regression analysis.
To assess whether the incidence of CPAs during either period showed a periodicity or correlation by time that might be a confounding influence, counts of occurrences per three months were analyzed using autocorrelation and partial autocorrelation functions (ACF, PACF), and significance was assessed using a portmanteau test. The ACF and PACF represent the covariance and correlation among time series by time lags. By analyzing these patterns, we can identify whether the time series are correlated. A periodic pattern, spike, or cut-off at a specific time suggests a correlation.
While three variables—age, CCI, and ASA class—were shown to be statistically different during the pre- vs post-RRS intervals, only the CCI was selected for risk adjustment because it also accounted for ASA and age. Statistical significance was defined as P < 0.025 after Bonferroni correction.
Results
During the study period, 207,054 surgeries were performed (pre-RRS: 95,197 cases; post-RRS: 111,857 cases, Table 1). Compared with the post-RRS period, surgical patients treated within the pre-RRS period were slightly younger (P < 0.001) and had relatively lower ASA (P < 0.001) and lower CCI (P < 0.001) scores. Nevertheless, the two groups could not be distinguished by the type of surgery (Appendix 3), emergency vs elective procedure, or the ratio of patient to ward nurses or physicians (Table 1).
Postoperative CPA not adjusted for risk
During the study period, 141 cases of sudden CPA were identified that included 75 cases during the pre-RRS period (0.079% incidence; 7.46/10,000 surgeries; 95% CI, 5.72 to 9.19) and 66 cases during the post-RRS period (0.059% incidence; 5.19/10,000 surgeries; 95% CI, 3.85 to 6.52). The relative risk of CPA in the post-RRS compared with the pre-RRS interval was 0.73 (97.5% CI, 0.48 to 1.13; P = 1.03), as shown in Table 2 and Fig. 2. Regarding the incidence of CPA during RRS operational (07:00–22:00 Monday–Friday; 07:00–12:00 Saturday) and non-operational hours, CPA was only less likely to occur during the operational hours following the implementation of the RRS (RR, 0.56; 97.5% CI, 0.31 to 1.02; P = 0.027, Table 2). The ACF and PACF analyses indicated a lack of correlation between CPA events (Appendix 4).
Incidence of postoperative CPA before and after RRS implementation. The blue diamonds and lines represent the incidence of CPA/10,000 surgical cases/3-month intervals regardless of operational hours, before and after the implementation of the RRS (7.46 per 10,000 cases pre-RRS vs 5.19 per 10,000 cases post-RRS, P = 0.06). The orange squares and lines indicate the incidence of CPA during RRS operational hours (4.52 per 10,000 cases pre-RRS vs 2.77 per 10,000 cases post-RRS, P = 0.049). The gray triangles and lines indicate the incidence during RRS non-operational hours (2.94 per 10,000 cases pre-RRS vs 2.41 per 10,000 cases post-RRS, P = 0.534). CPA = cardiopulmonary arrest; RRS = rapid response system
Charlson Comorbidity Index risk-adjusted CPA
Using a Poisson regression, the CCI-adjusted incidence of postoperative CPA deceased by 37% post-RRS implementation compared with the pre-RRS period (RR, 0.63; 97.5% CI, 0.41 to 0.98; P = 0.018). Furthermore, during RRS operational hours, there was a 52% reduction in the CPA incidence (RR, 0.48; 97.5% CI, 0.27 to 0.89; P = 0.008) although there was still no evidence for a reduction in the CPA incidence during non-operational hours (Table 2).
Patient characteristics and postoperative CPA outcomes
Amongst the patients who experienced postoperative CPAs, we observed no differences in age, sex, body mass index, ASA classification, cause of CPA, and time from surgery to CPA between the pre-RRS and post-RRS periods. Furthermore, there were no differences in the ten- and 30-day survival rates (Table 3). Lower rates of pre-arrest alarms within 24 hr before CPA were observed during the post-RRS period (45.5% vs 76%; P < 0.0001; Table 3), and this difference was observed during both RRS operational and non-operational hours (Table 3).
Discussion
We have shown that the implementation of an RRS is associated with a reduced rate of postoperative CPA in patients recovering in a general ward. The reduced incidence of CPA occurred only during RRS operational hours. Moreover, patients experiencing CPA after implementation of the RRS were less likely to show pre-arrest alarms. Nevertheless, patients experiencing CPA during the pre- and post-RRS periods could not be differentiated by their ten- and 30-day survival rates. These findings are consistent with our previous observations in hospitalized medical (non-surgical) patients admitted to an internal medicine ward.10
Postoperative mortality is influenced by the patient’s underlying preoperative medical status as well as surgery- and anesthesia-related factors.15,16 It is assumed that postoperative CPA may be prevented (or delayed) by providing early interventions in response to pre-arrest alarms alerting to potential postoperative cardiovascular or respiratory compromise.17,18 Early warning scores calculated from vital signs have been used to activate emergency response teams in hospitals in the United Kingdom, Australia, and the United States.19 In our hospital, the automatic electronic dashboard system (BESTboard®) tracks vital signs, in addition to blood chemistry tests including pH, PaCO2, PaO2, lactic acid, and total CO2. These are used to help detect metabolic or respiratory derangements that may be harbingers of cardiorespiratory collapse.20 In our previous study involving hospitalized medical (non-surgical) patients, pre-alarm laboratory abnormalities were observed in 11% of patients experiencing CPA compared with 35.5% of the postoperative patients experiencing CPA in the present study.10 Currently, the relative value of laboratory tests vs vital signs when assessing pre-arrest alarms remains controversial. We surmise that these laboratory test are useful indicators of impeding deterioration as they comprise components of the APACHE and sequential organ failure assessment (SOFA) scores.19
Hypotension, decreased oxygen saturation (SpO2), and increased PaCO2 were the first, second, and third most frequent pre-arrest alarms within 24 hr before CPA. Similarly, in our previous study involving hospitalized medical (non-surgical) patients, hypotension, decreased SpO2, and an abnormal respiratory rate were the most frequent pre-arrest alarm triggers.10,21
In our hospital, the automatic electronic dashboard system (BESTboard®) is refreshed every five minutes, but for most of the postoperative patients recovered in the general ward, vital signs were obtained intermittently at four to eight-hour intervals. While it seems reasonable to assume that more frequent monitoring of vital signs would result in a greater decrease in the incidence of CPA, there is some evidence to suggest that this may not be the case.22,23 Moreover, while continuous monitoring of vital signs is feasible with today’s technology, which permits real-time transmission of physiologic data, there are still major hurdles to overcome regarding frequent false alarms.19
Due to limited resources at our institution, the RRS is only operational for approximately 50% of the time, in contrast to other institutions that can offer this service full time. We speculate that a full-time RRS would yield a further reduction in the rate of CPA. Nevertheless, the present study and our previous study of hospitalized patients10 indicate that a part-time RRS may be a viable alternative when resources are limited. Future studies regarding the cost-effectiveness of an RRS should evaluate quality-adjusted survival years as an outcome when considering the associated medical costs and strain on hospital resources.24
The limitations of this study include its retrospective design and associated risk of bias. Additionally, we only collected data from a single tertiary care hospital, and therefore it is not known whether these observations are applicable to other institutions. We acknowledge that over the nine-year study period, technologic and medical advances and personnel changes may have contributed to a confounding effect on the CPA incidence. Our study also did not account for the likely effect of a learning curve during the transition period between pre-and post- implementation of the RRS, which may have influenced our findings.
In conclusion, the implementation of an RRS reduced the incidence of postoperative CPA among patients recovering in a general ward. This reduction was observed only during the RRS operational hours.
References
Kim HC, Yoo JW, Lim SY, et al. Mortality after in-hospital cardiopulmonary resuscitation: multicenter analysis in Korea. J Crit Care 2013; 28: 942-6.
Franklin C, Mathew J. Developing strategies to prevent inhospital cardiac arrest: analyzing responses of physicians and nurses in the hours before the event. Crit Care Med 1994; 22: 244-7.
Schein RM, Hazday N, Pena M, Ruben BH, Sprung CL. Clinical antecedents to in-hospital cardiopulmonary arrest. Chest 1990; 98: 1388-92.
Buist MD, Moore GE, Bernard SA, Waxman BP, Anderson JN, Nguyen TV. Effects of a medical emergency team on reduction of incidence of and mortality from unexpected cardiac arrests in hospital: preliminary study. BMJ 2002; 324: 387-90.
Calzavacca P, Licari E, Tee A, et al. The impact of rapid response system on delayed emergency team activation patient characteristics and outcomes–a follow-up study. Resuscitation 2010; 81: 31-5.
Wendon J, Hodgson C, Bellomo R. Rapid response teams improve outcomes: we are not sure. Intensive Care Med 2016; 42: 599-601.
Chen J, Ou L, Flabouris A, Hillman K, Bellomo R, Parr M. Impact of a standardized rapid response system on outcomes in a large healthcare jurisdiction. Resuscitation 2016; 107: 47-56.
Landoni G, Pisano A, Lomivorotov V, et al. Randomized evidence for reduction of perioperative mortality: an updated consensus process. J Cardiothorac Vasc Anesth 2017; 31: 719-30.
Bellomo R, Goldsmith D, Uchino S, et al. Prospective controlled trial of effect of medical emergency team on postoperative morbidity and mortality rates. Crit Care Med 2004; 32: 916-21.
Kim Y, Lee DS, Min H, et al. Effectiveness analysis of a part-time rapid response system during operation versus nonoperation. Crit Care Med 2017; 45: e592-9.
DeVita MA, Smith GB, Adam SK, et al. “Identifying the hospitalised patient in crisis”–a consensus conference on the afferent limb of rapid response systems. Resuscitation 2010; 81: 375-82.
Yoo S, Hwang H, Jheon S. Hospital information systems: experience at the fully digitized Seoul National University Bundang Hospital. J Thorac Dis 2016; 8: S637-41.
D’Hoore W, Sicotte C, Tilquin C. Risk adjustment in outcome assessment: the Charlson comorbidity index. Methods Inf Med 1993; 32: 382-7.
Trinkle RM, Flabouris A. Documenting rapid response system afferent limb failure and associated patient outcomes. Resuscitation 2011; 82: 810-4.
Brennan MF. Postoperative complication reporting: more than mortality and morbidity. Ann Surg 2013; 258: 8-9.
Arozullah AM, Henderson WG, Khuri SF, Daley J. Postoperative mortality and pulmonary complication rankings: how well do they correlate at the hospital level? Med Care 2003; 41: 979-91.
Sessler DI, Meyhoff CS, Zimmerman NM, et al. Period-dependent associations between hypotension during and for four days after noncardiac surgery and a composite of myocardial infarction and death: a substudy of the POISE-2 trial. Anesthesiology 2018; 128: 317-27.
Pignaton W, Braz JR, Kusano PS, et al. Perioperative and anesthesia-related mortality: an 8-year observational survey from a tertiary teaching hospital. Medicine (Baltimore) 2016; 95: e2208.
DeVita MA, Hillman K, Bellomo R, et al. Textbook of Rapid Response Systems: Concept and Implementation. Springer; 2017.
Jo S, Lee JB, Jin YH, et al. Modified early warning score with rapid lactate level in critically ill medical patients: the ViEWS-L score. Emerg Med J 2012; 30: 123-9.
Ting PC, Chou AH, Yang MW, Ho AC, Chang CJ, Chang SC. Postoperative reintubation after planned extubation: a review of 137,866 general anesthetics from 2005 to 2007 in a medical center of Taiwan. Acta Anaesthesiol Taiwan 2010; 48: 167-71.
Cardona-Morrell M, Prgomet M, Turner R, Nicholson M, Hillman K. Effectiveness of continuous or intermittent vital signs monitoring in preventing adverse events on general wards: a systematic review and meta-analysis. Int J Clin Pract 2016; 70: 806-24.
Ludikhuize J, Borgert M, Binnekade J, Subbe C, Dongelmans D, Goossens A. Standardized measurement of the modified early warning score results in enhanced implementation of a rapid response system: a quasi-experimental study. Resuscitation 2014; 85: 676-82.
Bravo Vergel Y, Sculpher M. Quality-adjusted life years. Pract Neurol 2008; 8: 175-82.
Acknowledgements
We sincerely thank the members of the RRT (Jong Sun Park, Dong Jung Kim, You-hwan Jo, Se-joong Kim, Ji-Won Kim, Yeonyee Yoon, Jin-Won Kim, Jung-Won Suh, Joonghee Kim, Jae-Hyuk Lee, Young-Jae Cho, and RRT nurse Da-Yun Lee), the intensivists, all nurses working in the ward and ICU, and CPR team. We also acknowledge the members of the medical informatics team, which prepared the screening system (BESTboard®) used by the SNUBH Medical Alert First Responder team (SAFER) at Seoul National University Bundang Hospital.
Conflicts of interest
None declared.
Editorial responsibility
This submission was handled by Dr. Steven Backman, Associate Editor, Canadian Journal of Anesthesia.
Author contributions
Tak Kyu Oh contributed to the study design and drafted the first version of the manuscript. Dong Seon Lee, Hyunju Min, Yun Young Choi, Eun Young Lee, Mi-Ae Yun, Yeon Joo Lee, Sang Hon Park, and Kyuseok Kim contributed to the data acquisition. Sooyeon Kim analyzed the data. Sang-Hwan Do and Jung-Won Hwang critically revised the manuscript. In-Ae Song contributed to the study design and provided critical revision of the manuscript. All authors approved the final version of the manuscript
Financial disclosures
None.
Author information
Authors and Affiliations
Corresponding author
Appendices
Appendix 1 Alarms for triggering the RRS
Alarm 1: SBP < 90 mmHg |
Alarm 2: HR < 50 or > 140·min−1 |
Alarm 3: RR < 10 or > 30·min−1 |
Alarm 4: BT > 39°C or < 36°C |
Alarm 5: SpO2 < 90% |
Alarm 6: pH < 7.25 |
Alarm 7: PaCO2 > 50 mmHg |
Alarm 8: PaO2 < 55 mmHg |
Alarm 9: Lactic acid > 4 mmol·L−1 |
Alarm 10: Total CO2 < 15 mmol·L−1 |
Appendix 2 Example of BESTboard® electronic dashboard

Appendix 3 Surgical procedures preceding CPA before and after RRS implementation
Postoperative CPA | Pre-RRS (01/2008–09/2012) n = 75 | Post-RRS (10/2012–12/2016) n = 66 | P value |
|---|---|---|---|
Cardiovascular surgery | 23 (30.7%) | 21 (31.8%) | 1.00a |
CABG - valve | 5 | 3 | |
Aortocoronary bypass − valve | 2 | 4 | |
Aortocoronary bypass + valve | 1 | 2 | |
Valve surgery | 3 | 4 | |
Major vascular surgery + valve | 4 | 5 | |
Major vascular surgery - valve | 2 | 2 | |
Vascular surgery in the extremities | 6 | 1 | |
General surgery | 14 (18.7%) | 14 (21.2%) | 0.87a |
Gastrectomy | 3 | 1 | |
Liver resection | 2 | 2 | |
Bowel | 3 | 4 | |
Exploration | 6 | 4 | |
Cholecystectomy | 0 | 2 | |
PPPD | 0 | 1 | |
Neurosurgery | 7 (9.3%) | 6 (9.1%) | 1.00a |
Brain | 3 | 2 | |
Decompression | 3 | 2 | |
Aneurysm clipping | 1 | 2 | |
Thoracic surgery | 14 (18.7%) | 14 (21.2%) | 0.87a |
Lung resection | 6 | 5 | |
Decortication | 2 | 3 | |
Esophageal resection | 1 | 1 | |
Pulmonologic procedure | 4 | 3 | |
Bleeding control | 1 | 1 | |
Mediastinal tumour resection | 0 | 1 | |
Orthopedic surgery | 9 (12.0%) | 7 (10.6%) | 1.00a |
Lower extremity | 3 | 3 | |
Upper extremity | 1 | 1 | |
Major joint | 4 | 2 | |
Spine surgery | 1 | 1 | |
ENT surgery | 3 (4.0%) | 2 (3.0%) | 1.00b |
Thyroidectomy | 1 | 1 | |
Laryngectomy | 1 | 1 | |
Neck dissection | 1 | 0 | |
Gynecologic surgery | 0 (0.0%) | 2 (3.0%) | 0.22b |
Debulking surgery | 0 | 2 | |
Plastic surgery | 1 (1.3%) | 0 (0.0%) | 0.50b |
Breast + free flap | 1 | 0 | |
Transplantation | 2 (2.7%) | 0 (0.0%) | 0.50b |
Kidney | 1 | 0 | |
Liver | 1 | 0 | |
Urologic surgery | 2 (2.7%) | 0 (0.0%) | 0.50b |
Radical cystectomy | 1 | 0 | |
Nephrectomy | 1 | 0 |
Appendix 4 Autocorrelation (ACF) and partial autocorrelation (PACF) function plots of CPA events per three-month intervals

The red line indicates the 95% confidence interval (CI) used to test for autocorrelation between events/three-month intervals. If the ACF or PACF exceeds the CI, the events may be correlated. Neither the ACF nor PACF exhibits a “spike” exceeding the CI or a pattern that suggests autocorrelation. Therefore, the events are considered to be independent and randomly distributed. CPA = cardiopulmonary arrest
Rights and permissions
About this article
Cite this article
Oh, T.K., Kim, S., Lee, D.S. et al. A rapid response system reduces the incidence of in-hospital postoperative cardiopulmonary arrest: a retrospective study. Can J Anesth/J Can Anesth 65, 1303–1313 (2018). https://doi.org/10.1007/s12630-018-1200-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12630-018-1200-5