Abstract
Purpose
The aim of this review was to provide a meta-analysis of all five of the most popular systems for arterial pulse contour analysis compared with pulmonary artery thermodilution, the established reference method for measuring cardiac output (CO). The five investigated systems are FloTrac/Vigileo®, PiCCO®, LiDCO/PulseCO®, PRAM/MostCare®, and Modelflow.
Source
In a comprehensive literature search through MEDLINE®, Web of Knowledge (v.5.11), and Google Scholar, we identified prospective studies and reviews that compared the pulse contour approach with the reference method (n = 316). Data extracted from the 93 selected studies included range and mean cardiac output, bias, percentage error, software versions, and study population. We performed a pooled weighted analysis of their precision in determining CO in various patient groups and clinical settings.
Principal findings
Results of the majority of studies indicate that the five investigated systems show acceptable accuracy during hemodynamically stable conditions. Forty-three studies provided adequate data for a pooled weighted analysis and resulted in a mean (SD) total pooled bias of −0.28 (1.25) L·min−1, percentage error of 40%, and a correlation coefficient of r = 0.71. In hemodynamically unstable patients (n = 8), we found a higher percentage error (45%) and bias of −0.54 (1.64) L·min−1.
Conclusion
During hemodynamic instability, CO measurement based on continuous arterial pulse contour analysis shows only limited agreement with intermittent bolus thermodilution. The calibrated systems seem to deliver more accurate measurements than the auto-calibrated or the non-calibrated systems. For reliable use of these semi-invasive systems, especially for critical therapeutic decisions during hemodynamic disorders, both a strategy for hemodynamic optimization and further technological improvements are necessary.
Résumé
Objectif
Le but de cette revue était de fournir une méta-analyse des cinq systèmes les plus connus d’analyse de contour du pouls artériel comparativement à la thermodilution artérielle pulmonaire, la méthode de référence actuelle de mesure du débit cardiaque (DC). Les cinq systèmes étudiés sont: FloTrac/Vigileo®, PiCCO®, LiDCO/PulseCO®, PRAM/MostCare® et Modelflow.
Source
Une recherche étendue des publications dans les bases de données MEDLINE®, Web of Knowledge (v.5.11), et Google Scholar, nous a permis d’identifier les études prospectives et les analyses qui comparaient l’approche par le contour de pouls avec la méthode de référence (n = 316). Les données extraites de 93 études sélectionnées incluaient les valeurs de l’étendue et de la moyenne du débit cardiaque, les biais de mesure, les erreurs de pourcentages, les versions des logiciels et la population des études. Nous avons réalisé une analyse groupée et pondérée de leur précision à déterminer le DC chez différents groupes de patients et dans divers contextes cliniques.
Constatations principales
Les résultats de la majorité des études indiquent que les cinq systèmes analysés affichent une précision acceptable dans les situations hémodynamiquement stables. Quarante-trois études ont fourni des données convenables pour une analyse groupée et pondérée; elles ont abouti à un biais groupé total moyen (É.T.) de −0,28 (1,25) L·min−1, une erreur de pourcentage de 40 % et un coefficient de corrélation r = 0,71. Chez des patients hémodynamiquement instables (n = 8), nous avons trouvé une plus grande erreur de pourcentage (45 %) et un biais de −0,54 (1,64) L·min−1.
Conclusion
Au cours d’un épisode d’instabilité hémodynamique, la mesure du DC basée sur l’analyse continue du contour du pouls artériel ne montre qu’une concordance limitée avec la thermodilution par bolus intermittents. Les systèmes calibrés semblent procurer des mesures plus précises que les systèmes auto-calibrés ou les systèmes non calibrés. Pour une utilisation fiable de ces systèmes semi-invasifs, en particulier pour des décisions thérapeutiques critiques au cours des troubles hémodynamiques, il est nécessaire de définir une stratégie d’optimisation hémodynamique et de bénéficier d’améliorations technologiques.
Similar content being viewed by others
A pulmonary artery catheter (PAC) is a device utilized in intensive care units (ICU) to measure the pressures in the superior vena cava, right heart, and pulmonary artery. It also enables the invasive assessment of cardiac output (COPAC) or stroke volume (SV) by thermodilution (TD). The use of a PAC is declining1 as significant complications have been associated with the procedure2,3 which have resulted in an increase in mortality4,5 and have raised doubts about its possible benefits.5 In contrast, a recent report concluded that the use of a PAC did not alter the mortality, general ICU or hospital length of stay, or cost for adult patients in intensive care.6 Furthermore, it has been emphasized that inappropriate clinical decisions and/or inaccurate hemodynamic data may well constitute a greater risk to the patient than all other PAC-related complications.7 Thus, for many investigators, measuring cardiac output (CO) using a PAC still represents the clinical reference method of choice8-11 when evaluating the accuracy or trending capability of less invasive techniques for measurement of CO.
Less invasive CO techniques are mostly based on arterial pulse contour analysis (PCA), which has been investigated for more than a century12 as a method for estimating and monitoring the SV on a beat-to-beat basis. In 1904,13 it was pointed out that SV is proportional to pulse pressure (the difference between systolic and diastolic blood pressure). At present, systems based on the pulse contour concept14,15 are far from being generally accepted as a reference method because other factors influence the pulse wave (e.g., underdamping/resonance artifacts frequently affect blood pressure measurement)16 and because of technical problems (e.g., proper calibration).17
For the assessment of CO by arterial pulse contour analysis (COPCA), an arterial catheter is required (usually already in place in critically ill patients). The invasiveness of these systems depends on the different calibration requirements.18 So-called calibrated pulse pressure analysis systems have to be referenced to another accepted (invasive or non-invasive) method. Calibration via transpulmonary (TP) TD (PiCCO/PiCCOplus),11 lithium indicator dilution (LiDCO), or bolus TD (Modelflow) requires central venous access. The Edwards FloTrac/Vigileo needs no invasive calibration but refers to an autocalibration algorithm based on the patient’s demographic data, as detailed in patent applications,Footnote 1 , Footnote 2 with the aim of adjusting for different hemodynamic situations. With the LiDCO system, the new LiDCOrapid also offers the possibility of autocalibration via a patient-specific scaling factor.Footnote 3 In contrast, the PRAM/MostCare system provides a quasi continuous cardiac output (CCO) readout requiring only a catheter in the radial or femoral artery without any calibration. An overview is presented in Table 1 (see Appendix 1 for further technical details).
In this work, we present an extensive review of five semi-invasive systems, tested over a span of 20 years, their underlying technologies, and how they correspond with COPAC. Other recent reviews9,10,18-26 focused on only a single system or excluded at least one of the systems based on arterial pulse contour analysis. This review includes all of the five most popular commercially available systems and also provides technical details (based on their underlying patents) of the individual CO measurement systems. Furthermore a comprehensive pooled weighted analysis of their precision in various patient groups and clinical settings was performed and compared with that of COPAC. In previously published studies, meta-analyses were performed for only a single system,22 or the data of different pulse contour systems were analysed as a pooled unit.23 Our systematic analysis also explores possible differences between calibrated and non-calibrated systems, software generations, and performance differences during hemodynamically stable and unstable conditions. Nevertheless, because of incomplete data in the studies, not all of the reviewed studies were included in the analysis.
Methods
This systematic review was carried out in accordance with recommended methods as established by the Cochrane Methods Group on Screening and Diagnostic Tests, and this review also fulfils the criteria as set by the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) group (http://www.prisma-statement.org/).
A literature search covering the topic of semi-invasive CO measurement was performed using the keywords “cardiac output, (pulmonary) thermodilution CO, semi-invasive and minimally invasive CO, Vigileo, FloTrac, PiCCO, PRAM, LiDCO, PulseCO, Modelflow, and CO gold standard”. We searched electronic data bases up to August 2013, including MEDLINE (from 1990), Web of Knowledge (v.5.11) (from 1990), and Google Scholar. The search strategy included the following free-text and index terms: “arterial pressure-based cardiac output” or “arterial pressure waveform cardiac output” or “cardiac output” or “FloTrac” or “pulmonary artery thermodilution” or “thermodilution” and not “experimental” and not “pediatric” and not “animal”. In review articles, the bibliography was screened additionally for clinical reports and investigations of COPAC vs COPCA.
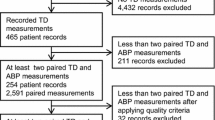
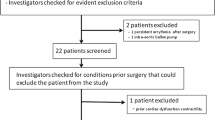
Two of the authors (T.S. and H.G.) carefully evaluated the search results (n = 416) to select the eligible articles for inclusion (see Appendix 2). First, obviously irrelevant items were excluded by reviewing the title and/or abstract of the records. Next, the full-text articles of the remaining papers (n = 238) were retrieved and checked to determine if they met the following eligibility criteria: 1) The study was published in a peer-reviewed journal written in English or German; 2) It was not retracted for any reason (n = 3); 3) It was performed in adults; 4) The study described a clinical investigation using one or more semi-invasive CO measurement systems to compare simultaneous measurements of CO or cardiac index with measurements using intermittent bolus right heart TD; and 5) Studies that did not use continuous CO measurements (e.g., Vigilance, Edwards Lifesciences) instead of COPAC as the reference method. After additionally screening the full-text articles as described, 108 clinical studies were selected for the review (see Fig. 1).
As the intention of this work was to focus on CO data based on arterial pulse contour analysis, we did not analyse derived parameters (e.g., systemic vascular resistance) or volumetric parameters (e.g., extravascular lung water) offered by the EV1000/Volume View from Edwards Lifesciences or by the PiCCO systems or LiDCOrapid for perioperative SV optimization and fluid administration. Other methods, like the Fick principle applied to carbon dioxide re-breathing techniques, esophageal Doppler velocimetry, or CO measured by bioimpedance, were excluded as well. The newly introduced Nexfin (BMEYE, The Netherlands), a photoplethysmographic technology which also offers the ability to measure CO noninvasively, was excluded because only two studies27,28 were found that supplied adequate data. In addition, noninvasive blood pressure monitoring with Nexfin did not seem to be sufficiently accurate to replace intra-arterial invasive blood pressure measurements in critically ill patients,29 a result that a priori questions its usefulness for noninvasive CO assessment.
Finally, out of these 108 studies, 80 publications with multiple (93) comparisons were analysed to assess the agreement of any of the five semi-invasive systems with intermittent bolus TD CO. In five publications, two or more systems were simultaneously compared with COPAC, and in five publications, two different software versions/generations were used. The five systems, PiCCO, LiDCO, Modelflow, PRAM and FloTrac, contributed 25, 12, 7, 9, and 40 trials, respectively, to the 93 comparisons. The following data were collected from the 80 publications: number of patients, age range and data points for each study, mean CO (SD), CO range, bias (SD) (semi-invasive system vs intermittent bolus TD), percentage error (PE), correlation coefficient (r), software version, study population, arterial access site, study design (blinded or non-blinded observers), and study limitations reported by the authors of the publications. In addition, we collected our own observations of study limitations. In case certain values (e.g., PE) were not reported, they were calculated from other values where possible. To fulfil the Critchley and Critchley criterion (C&Cc),30 a PE of ≤ 30% between the new CO measurement technique and COPAC had to be achieved. The PE was calculated as twice the SD of the bias divided by the mean CO.30 If the mean CO or the range of CO measurements was not stated explicitly in tables or text, it was estimated from the graphs. In seven studies, only the cardiac index was quoted, and we calculated CO from the body surface area (BSA). If BSA was not provided by the authors, a value of 1.9 m2 was assumed.
Statistical analysis
For each of the five semi-invasive CO measuring systems, mean CO, bias, SD of the bias, and correlation coefficient (r) were included in a pooled weighted analysis and weighted according to equation 1 23 and equation 2 31 on the number of measurements in each trial (see Appendix 3).
The pooled weighted PE was calculated as twice the pooled weighted SD of the bias over the mean pooled weighted CO. The pooled weighted analysis was done for all semi-invasive systems and separately for each system. In the FloTrac/Vigileo (COFT) studies, sub-group analysis of the three different software releases – first generation (V1.0-V1.03), second generation (V1.07-V1.14), and third generation (V3.0 and higher) – was performed to investigate whether software modifications are reflected in performance improvements. The PiCCO system is initially calibrated with TP TD. The performance of the PiCCO system strongly depends on the re-calibration interval;32,33 on the one hand, the interval is not always given by the authors, and on the other hand, different intervals have been suggested depending on the investigating group.34-36 Therefore, studies comparing PiCCO with TP TD as the reference method were excluded to avoid false positive distortion of the results relating to precision.
To verify whether the studies selected for the pooled weighted analysis are a representative selection of all 93 studies, the PE distribution of the studies in the pooled weighted analysis and that of all studies (if reported or at least calculable) were compared with a two-sample Kolmogorov-Smirnov test.
Additionally, a forest plot was drawn in order to provide further information for 14 studies dealing with hemodynamically unstable conditions. The 14 studies could not be included in the pooled weighted analysis because of incomplete data.
The statistical analysis was performed with SPSS® for Windows Release 20.0.0 (SPSS Inc., Chicago, IL, USA). Data are presented as mean (SD) or bias (SD) with a value of P < 0.05 considered significant.
Results
All 93 trials investigating the agreement of the five semi-invasive CO systems with intermittent bolus TD are listed in Appendix 4. The systems are grouped according to their different calibration methods (auto-calibrated, calibrated, and non-calibrated). Studies examining the same system are sorted by publication date in descending order.
FloTrac/Vigileo system
First-generation software (N = 10)
Nine out of ten studies investigated the performance of the first FloTrac generation (COFTg1) in cardiac surgery patients during fairly stable hemodynamic conditions. Although eight trials (80%) referred to the C&Cc, only four authors stated the mean or range of CO measurements. In five studies, different arterial access sites were used and the data were pooled.
Six studies37-42 classified the performance of the COFTg1 as not satisfactory and demonstrated poor accuracy, with the PE (40-55%) clearly exceeding the 30% limit of acceptability. Only three studies43-45 reported a PE < 40%, and the smallest PE of 33% with a bias of 0.55 (0.98) L·min−1 was reported in a study of 50 postoperative cardiac surgery patients.43 The only study46 using solely femoral arterial access found a bias of −0.15 (0.33) L·min−1 with COFTg1, and neither mean CO nor PE was mentioned. None of the ten studies fulfilled the C&Cc.
Second-generation software (n = 24)
Most of the FloTrac studies (n = 24) used the second-generation software (COFTg2). In 21 (88%) of the studies, PE was presented or calculable. In contrast with the COFTg1 evaluations, the second-generation studies were performed in various patient cohorts. Two authors45,47 consider modifications between the first- and second-generation software to have resulted in better accuracy in the CO measurements. Only six studies (four studies in cardiac surgery, one in liver transplant, and one in septic shock patients)45,48-52 using the second-generation software reported acceptable precision with a PE < 30%. During/after cardiac surgery,53-57 liver transplantation,58 and during septic shock,59 PE was < 50% (32-48%) with correlation coefficients ranging from r = 0.32-0.90. On the other hand, a high PE > 60% during cardiac surgery,60,61 in hyperdynamic cirrhotics,62 and in patients undergoing liver transplantation63 points to the fact that COFTg2 may deviate considerably from COPAC.
Up to now, four studies51,58,62,64 have reported a (logarithmic) relationship between the bias of COFTg2 and systemic vascular resistance (SVR), with the observation, the higher the bias, the lower the SVR.
Third-generation software (n = 6)
In two studies evaluating the FloTrac third-generation software (COFTg3), only poor agreement with COPAC was found during liver transplantation65,66 and in one study with septic shock patients.67 In contrast, in another study with septic patients51 and with cardiac surgery,68 COFTg3 and the COPAC reference agreed, with a PE of 29% and 22%, respectively.
When compared with the second generation, the third-generation software seems to be less sensitive to a changing SVR, thus resulting in improved overall precision and trending ability.51,66 Nevertheless, after living-donor liver transplantation, the bias between COFTg3 and COPAC still became apparent when SVR was < 1,000 dyne·sec·cm−5.69
According to the manufacturer,Footnote 4 the site of arterial access55 should not affect FloTrac/Vigileo results. Almost all studies investigated FloTrac performance via radial artery access (see Appendix 4). Five studies compared the radial vs the femoral access site. The results of two studies43,60 point to a modest but not negligible influence of the arterial access site. With a PE difference < 5%,51,55,68 arterial site-independent results were observed with COFTg2 and COFTg3. Two other studies using femoral access70,71 reported only limited agreement with COPAC during cardiac surgery.
PiCCO/PiCCOplus system (n = 25)
Twenty-five studies were identified that supplied adequate data in terms of bias and precision, and 21 of them were in cardiac surgery patients. The PE was revealed by the authors or calculable on the basis of other values in only 14 trials (58%). Range and mean CO were quoted in eight trials (32%). In 21 (88%) trials, the PiCCO catheter was inserted via the femoral artery.
The recalibration interval and the influence of the SVR on PiCCO-derived CO (COPiCCO) are still discussed controversially in the literature. According to two studies,70,72 changes in SVR do not affect the accuracy of COPiCCO if a recalibration is performed every four hours. Another study in hemodynamically stable patients73 emphasizes that recalibration of PiCCO is not necessary more often than every three hours and that COPiCCO is clinically acceptable (PE not stated). Nevertheless, the same authors recommend additional studies with PiCCO in septic shock patients or during the use of vasoactive drugs. Three studies34-36 concluded that recalibration of the PiCCO is necessary at least after marked changes in SVR. The requirement of frequent recalibration, especially in the presence of vasopressors, is also discussed by other authors.74,75 Remarkably, excellent results were found when COPiCCO and COPAC were compared in stable cardiac surgery patients,76 as long as there were no significant changes in SVR36 [bias (SD) of 0.23 (0.50) L·min−1 and PE 20%]. When the whole study period was evaluated, however, the PE of 36% exceeded clinical acceptability. Without any recalibration, a high bias > 1.0 L·min−1 and SD > 2.0 L·min−1 of COPiCCO was observed.77,78 When initial calibration was performed with COPAC instead of TP TD CO (COTPTD), PiCCO results were not comparable with the reference method: COPiCCO was underestimated and low correlation coefficients (r < 0.40) were found and, if calculable, PE was beyond clinical acceptability.21,46,71,79
In hemodynamically stable cardiac surgery patients, comparable but not interchangeable results (PE 34-43%) were observed. The PiCCO system was acknowledged to be useful to monitor trends, but intermittent bolus TD remained the method of choice for measuring CO.55,80,81 In similar patients,82,83 COPAC and COPiCCO did not agree and showed large discrepancies (PE > 50%). Just a few authors reported a PE < 30%, indicating interchangeable results of COPiCCO and COPAC.45,76,84-86
Several studies35,46,47,87-89 performed only in cardiac surgery patients reported a small bias < 0.5 L·min−1 with a SD > 0.5 L·min−1 and correlation coefficients up to r = 0.93. Although the authors argue that COPiCCO is a reliable alternative to COPAC, it has to be emphasized that important information (PE and mean) is not given.
LiDCO/PulseCO system (n = 12)
Nine of 12 studies comparing LiDCO-derived CO (COLI) with COPAC reported the PE. Eighty-three percent of the investigators used radial artery access to measure the arterial lithium concentration. Up to now, the new LiDCOrapid system has been evaluated only in animal studies or compared with other CO measurement methods but not with bolus COPAC, therefore, the studies were not included in our analysis. COLI showed good agreement with COPAC during hemodynamically stable conditions post cardiac surgery,90-93 after liver transplantation,94 and in patients with severe pre-eclampsia.95 Three studies showed clinical acceptability of LiDCO (PE < 30%), although initial calibration was performed with intermittent bolus TD instead of the manufacturer recommended lithium dilution technique.21,71,96 Nevertheless, with initial COPAC calibration and without any recalibration, COLI overestimated COPAC during cardiac surgery.97 Two studies (22%) postulated that LiDCO cannot be used interchangeably with COPAC in liver transplant patients63 or in a mixed study population, including septic patients42 COLI clearly failed to show acceptable accuracy (PE of 76% and 40%, respectively).
Modelflow system (n = 7)
In six of the studies evaluating CO with the Modelflow system (COMF), the PE was stated or at least calculable, and met the 30% limit. All studies but two98,99 were performed in rather small patient groups (n < 30 patients). After calibration with COPAC, COMF showed high accuracy with pressure signals obtained from a radial or femoral artery and was able to replace intermittent bolus TD during cardiac surgery21,99,100 and in septic shock patients.101 Nevertheless, the C&Cc was not fulfilled during liver transplantation.98 After aortic diameter calibration102 instead of TD calibration, COMF showed clinical acceptability (PE = 12%). Interestingly, even with noninvasive pressure signal monitoring after ultrasound calibration, a small bias and small SD was reported in critically ill ICU patients.103
PRAM/MostCare system (n = 9)
The nine studies suitable for analysis can be divided into studies with excellent and comparable results for CO measured by PRAM (COPRAM) and COPAC and into studies which show only poor agreement between the two methods. The PRAM technique was reliable in patients undergoing left or right heart catheterization.104,105 Pressure in both studies was recorded via an aortic catheter and not from a peripheral arterial line. Excellent performance of COPRAM was also reported during106,107 and after cardiac surgery108 and in patients with an intra-aortic balloon pump.109 Despite these findings, differences between COPAC and COPRAM became evident at extremely high or low CO values.105,106 In septic shock patients,110 there appeared to be no correlation between SVR and bias, and the C&Cc was met (PE = 25%). The results of two post cardiac surgery studies111,112 are in clear contrast with those of other studies.104-110 It should be pointed out that the latter studies were performed either by the same group or by authors cooperating with this group. The reason for the enormous discrepancy between these two groups of studies (PE > 73%) is not clear, especially since study sizes and participants were comparable.
Pooled weighted analysis
Forty-three (46%) of 93 trials listed in Appendix 4 provided adequate data for a pooled weighted analysis of mean CO, bias (SD), and PE: eight (32%) studies on PiCCO, five (42%) studies on LiDCO/PulseCO, seven studies (100%) on Modelflow, five studies (56%) on PRAM, and 18 studies (45%) on FloTrac/Vigileo (n = 4/9/5 trials with the first/second/third-generation software, respectively).
The PE distribution of the 43 selected studies for the pooled analysis (Table 1) and of all studies compiled in Appendix 4 showed no significant differences (P = 0.96) across the percentile ranking (two-sample Kolmogorov-Smirnov test).
The calculated mean weighted pooled data are presented in Table 3. The 43 studies (5,780 measurements in total) resulted in a pooled weighted bias of −0.28 (1.25) L·min−1 and a pooled weighted PE of 40%. Thus, our findings are in concordance with another meta-analysis23 reporting a pooled PE of 42.1% in 21 studies with pulse contour systems. The pooled bias points to underestimation of COPAC in all systems with the exception of PRAM (Fig. 2A). Worth highlighting, the widest range in bias was observed with COFTg3. The pooled PE was lowest for COLI (27%) and highest for COFT (52%; in subgroup FTg2 59%). Only LiDCO fulfilled the C&Cc; PiCCO and Modelflow exceeded it marginally (PE = 32%), FloTrac/Vigileo (third-generation software) and PRAM grossly exceeded the 30% limit (PE 47% and 44%, respectively), as also shown in Fig. 2B. In the COFT subgroup analysis (see Table 3 and Fig. 3), the lowest bias of 0.06 (1.31) L·min−1 and the lowest PE (45%) in this group were found in the first-generation software.
Pooled weighted bias (A) and percentage error (B) showing agreement of cardiac output measured by five semi-invasive systems (FTg3: n = 5; LiDCO: n = 5 Modelflow: n = 7; PiCCO: n = 8; PRAM: n = 5) and intermittent bolus thermodilution. º Mean pooled weighted bias and PE (cardiac output [CO]method vs COPAC); bars indicate range of bias and PE, respectively. Broken lines represent zero bias (A) and the 30% Critchley & Critchley criterion (C&Cc) (B). COPAC = cardiac output assessed using a pulmonary artery catheter; PE = percentage error
Pooled weighted bias (A) and percentage error (B) showing agreement of cardiac output measured by FloTrac, first, second, and third (n = 4/9/5, respectively) software generation and intermittent bolus thermodilution. º Mean pooled weighted bias and percentage error (PE) (COFT vs COPAC); bars indicate range of bias and PE, respectively. Broken lines represent zero bias (A) and the 30% Critchley & Critchley criterion (C&Cc) (B). COFT = cardiac output assessed using the FloTrac system; COPAC = cardiac output assessed using a pulmonary artery catheter
Eight of these 43 studies were performed in liver transplant and septic shock patients and used for a sub-analysis to investigate the differences in performance in hemodynamically unstable situations (Fig. 4). With 1,911 measurements in total, the five semi-invasive systems (PiCCO/ LiDCO/ Modelflow/ PRAM/ FloTrac) contributed with n = 0/1/2/0/5 trials, respectively, to the hemodynamically unstable cohort. This cohort yielded a pooled weighted bias of −0.54 (1.64) L·min−1 (Fig. 4A) and a pooled weighted PE of 45.3% (Fig. 4B) with r = 0.75. Compared with all studies included in the analysis, hemodynamic instability results in a slightly higher PE (5% higher) and bias. The exclusion of the eight studies performed in unstable patients yielded a smaller bias of −0.15 (1.04) L·min−1 and a smaller PE (38%) compared with all studies in the pooled analysis (Table 2).
Pooled weighted bias (A) and percentage error (B) showing agreement of all studies included in the analysis (n = 43); studies excluding hemodynamically unstable conditions (n = 35); and those studies referring to hemodynamically unstable conditions (n = 8). º Mean pooled weighted bias and percentage error (PE) (cardiac output [CO]method vs COPAC); bars indicate range of bias and PE, respectively. Broken lines represent zero bias (A) and the 30% Critchley & Critchley criterion. COPAC = cardiac output assessed with a pulmonary artery catheter
Thirty-nine studies (Table 4) met the criteria for pooled weighted analysis of the correlation between the five systems and bolus TD. The highest correlation was found for COLI (r = 0.88) and the lowest for COFT (r = 0.54; in the subgroup FTg1 r = 0.50). A correlation coefficient was given in only one study with COFTg3 (r = 0.67). For all semi-invasive studies, the pooled weighted correlation resulted in r = 0.71 and was slightly lower than in a recently published analysis including only 12 pulse contour studies (r = 0.75).23
In order to show the results obtained in hemodynamically unstable patients, we also analysed the bias and confidence intervals in those studies; however, because of incomplete data, the results could not be included in the pooled analysis. These results are compiled in the forest plot (Fig. 5) covering FloTrac (n = 5, second generation and n = 4, third generation), PiCCO (n = 1), LiDCO (n = 2), and Modelflow (n = 2). All but two pulse contour systems underestimated CO compared with COPAC.
Forest plot showing the agreement of cardiac output measured by five semi-invasive systems with intermittent bolus thermodilution in 14 studies referring to hemodynamically unstable conditions. ■ bias (cardiac output [CO]method vs COPAC); bars indicate the 95% confidence interval. COPAC = cardiac output assessed with a pulmonary artery catheter. *Cardiac index converted to cardiac output with body surface area of 1.9 (L·min−1·m−2). The 14 selected studies include the eight from Fig. 4 designated as unstable plus those six studies in which neither the mean cardiac output (CO) nor the number of data points were stated. Notice that studies with septic patients and with liver transplant patients characterized as “hemodynamically stable” by the author or studies in which the bias was given in % are excluded (see Appendix 4)
Discussion
For monitoring in the perioperative period and in the critical care setting, systems based on pulse contour measurement have recently been offered as a more-or-less accurate and safe alternative113 to the highly invasive Swan-Ganz PAC. Despite continued efforts to introduce improved products to the market, the main outcome of our analysis is that a clear recommendation cannot be given for any single system that can accurately monitor hemodynamically unstable patients. This limitation also applies to reliable intraoperative monitoring during surgery accompanied by hemodynamic instability. The informative value of COPCA-based monitoring during hemodynamically stable conditions should be questioned, since CO data provided by these monitors parallel the arterial pressure as long as the compliance and resistance remain unaffected.
From the technical point of view, it is important to be aware of the inherent limitations of the mathematical models/algorithms implemented. Important model parameters might have been derived from patient cohorts that might not always fully match the critical care patients to be monitored. It is therefore necessary to readjust these parameters, especially during hemodynamic instability. We found no explicit evidence that suggested calibration intervals were strictly followed. If this were the case, it seems clear that the calibrated systems would provide more accurate CO data than the non-calibrated or auto-calibrated systems.
This is in line with our results showing the calibrated systems to be more accurate (LiDCO, Modelflow, and PiCCO) than the auto-calibrated FloTrac or the non-calibrated PRAM (see Fig. 2). It is noteworthy that almost all systems failed to fulfil the C&Cc in both hemodynamically stable and hemodynamically unstable scenarios (Table 3).
COPAC as reference method of choice
Although COPAC was long the “gold standard” and is still widely accepted as the reference method of choice for CO determination,114,115 the method itself suffers from several limitations. Besides its invasiveness and the concomitant risks, the accuracy of the method also depends on external factors, e.g., overestimates have been reported at low CO levels.116 Other factors that may influence the accuracy of bolus TD are valve insufficiency, fluid discontinuation and shunting,117 ventilation,118 transition from cardiopulmonary bypass,119 and operator experience. Triplicate injections are recommended to achieve acceptable accuracy,117,120 although it has also been shown that four CO measurements in series must be averaged in order to be 95% confident that the result is within 5% of the “true” CO.121 When all these factors are taken into account, the overall accuracy of the TD reference COPAC may be ± 15% at best (in a recent in vitro study, the PE was shown to range from 13-15.3%).122 In light of this basic limitation, the question of clinically acceptable error has to be raised. When C&C analysed 34 studies (23 bioimpedance vs COPAC, 11 Doppler vs either COPAC or Fick CO2 rebreathing),30 they found differences between the methods, i.e., up to 37% in the PE for PAC/Fick and up to 65% higher for Doppler measurements. The authors considered an error of 20% acceptable for clinical practice. When methods with a 20% error are compared, a deviation of up to 28.3% will result. Therefore, C&C30 concluded that a deviation of < 30% would still be acceptable when comparing a new CO measurement system with COPAC. This position has also been challenged123 because quoting the PE as an adequate criterion without reporting the precision of the reference technique124 or the confidence intervals125 could lead to erroneous conclusions. It has been proposed to enlarge the acceptable PE to 45%,123 which would mean that the tested method would show a precision of only 42.4% and 40.3%, respectively, when assuming a precision of 15% or 20% for the reference method.
Limitations with respect to the accuracy of the chosen reference method
When aiming at a sufficiently close estimate of the “true” precision of the tested method, it is important to be clear about the accuracy of the reference method. We were not able to define the averaged precision of the reference method for the pooled 43 studies, as the relevant data on the reference were only sparsely described or not reported. If the reference technique had been performed with less precision than the generally accepted 20%, then this would have resulted in a smaller PE for the tested semi-invasive method124 and in the acceptance of the studied technique based on a questionable level of precision. None of the investigators stated the predicted level of precision for the tested technique at the start of their study.
Limitations in our analysis with regard to available data
First, with respect to our analysis, we appreciate that the number of studies varied considerably for the different systems (from seven Modelflow up to 40 FloTrac/Vigileo studies). No more than 43 reports (46%) out of 93 trials in our extensive literature search provided adequate data for a pooled weighted analysis, a fact which considerably reduced the available data pool for a thorough evaluation and thus weakened the statistical power. Furthermore, due to shortage of data we could not perform a detailed sub-analysis regarding the influence of vasoactive drugs, reasons for hemodynamic instability, or differences with respect to peri-, intra-, and postoperative CO conditions.
Second, the significant heterogeneity in the number of data pairs evaluating the different CO devices impairs the strength of our analysis.
Third, in seven papers cardiac index but not CO data were reported. Assuming a body surface area of 1.9 m2 could possibly have modified our overall results; however, we consider such modification to be insignificant.
Fourth, studies that compare these systems with other reference methods were explicitly excluded (as outlined in our Methods section), reducing the available body of knowledge on the performance of COPCA methods. For example, we excluded several studies comparing the FloTrac/Vigileo with CCO69,123,126-130 as well as with TP TD131-133 or esophageal Doppler.134 We also excluded the few available studies comparing LiDCO with TP TD135 or CCO136 as well as an evaluation of the PRAM system vs CCO.109 A single study evaluated the Modelflow device using graded lower body negative pressure.137
Comparison of systems
For the FloTrac/Vigileo system, 18 applicable studies using different software versions were selected, and only two studies48,65 met the C&Cc. If the software version was not stated, we inferred the version from another study.22 Remarkably, the smallest PE (45%) in the pooled analysis of FloTrac data was found in the studies using devices with first-generation software but in hemodynamically stable conditions (see Fig. 3B). The highest pooled PE (59%) was found in studies using the second-generation software, but these investigations were performed in patients in hemodynamically less stable conditions. When the manufacturer introduced the third-generation software, it was claimed to take enhanced account of changing hemodynamic conditions.Footnote 5 Though there is a modestly smaller bias in the third-generation software than in the second (see Figs. 3 and 5); nevertheless, it is important to be aware that COFTg3 may grossly deviate from COPAC or CCO during hemodynamic instability138 and particularly in extreme conditions of vasoconstriction or vasodilation.123 As yet, the FloTrac/Vigileo algorithm for autocalibration apparently adjusts insufficiently for gross changes.
For the PiCCO system, only eight of 25 studies included sufficient data to be included in the pooled weighted analysis. The lowest reported PE was 20%;36 however, this was measured in the pre-induction phase of anesthesia. In the pooled analysis, PiCCO exceeded the PE criterion only marginally (PE = 32%). Since almost all data were obtained in hemodynamically stable conditions, it must be concluded, based on the available data, that it is not possible to judge the reliability of PiCCO under hemodynamically unstable conditions.
Many studies assessing the three other CO measurement systems (LiDCO, PRAM, and Modelflow) show a PE of 30%; however, one should note that most of these studies were performed in only three centres (Modelflow as well as PRAM). For the PRAM system, two studies from external centres report high PEs of 87%111 and 73%,112 respectively, yielding a pooled weighted PE of 44%. The PRAM device was the only system showing a pooled bias overestimation (0.14 L·min−1), while all other devices underestimated COPAC. Remarkably, with a pooled PE of 27% (LiDCO), just one of the five semi-invasive systems fulfilled the C&Cc, and the highest pooled correlation coefficient was found with LiDCO (r = 0.88). On the other hand, a most recent LiDCO study performed in animals139 highlights a large bias between COLI and COPAC and identifies a number of drugs used in perioperative medicine that influence the accuracy of the LiDCO sensor in vitro.140 As we found no comparisons with COPAC in humans, LiDCOrapid studies were not included in our analysis. This auto-calibrated systemC was validated against the commonly used LiDCO indicator dilution-based calibration and a correlation of r = 0.88 was reported. According to the manufacturer, the scaling factor estimate may not be as precise as an independent calibration with a well-performed indicator dilution method. It therefore remains highly questionable whether the auto-calibrated LiDCOrapid system would successfully replace the lithium indicator calibrated measurement. Special care should be taken when using LiDCOrapid, especially in patients with severe peripheral vasoconstriction with the particular requirement of high-fidelity pressure recording.C
Tracking changes
With respect to measuring trends in CO, the capabilities of various CO measurement devices (Vigileo, PiCCO, bioimpedance, Doppler sound, and pulse contour) were carefully analysed in a recent review.141 If these devices are used to track changes in CO, induced for instance by preload changes, care must be taken to ensure there are no additional influences from altered vascular tone.24 A most recent study142 emphasizes the rather poor performance of the Vigileo system in tracking changes in CO induced by increased vasomotor tone: the concordance rates between COPAC- and COPCO-changes were 67.5%, 28.8%, and 7.7% in the low, normal, and high SVRI states, respectively.
A recent report143 emphasizes that, in clinical practice, the dynamic response (trending) to interventions is more important and critical than absolute values of CO. More serious consideration should be given to the ability to track (induced) CO changes144 as well as the impacts of time and repetitive measurements over time.145 Accordingly, future studies should include the analysis of trending ability using three different statistical techniques:66 by correlation coefficients between the system under evaluation and the particular reference method, by a modified Bland and Altman analysis using ΔCO data (ΔCO representing the change between sequential readings), and by plotting Δsemi-invasive CO against ΔCOPAC on a four-quadrant plot.146
When to use semi-invasive PCA systems?
Unstable hemodynamics appears to be a general problem for pulse contour analysis.38 In unstable conditions, intraoperatively, and in the ICU, our results show a 7% higher PE and a larger bias (−0.54 vs −0.15 L·min−1) than in the hemodynamically stable cohort (Fig. 4). In such situations, a more reliable and invasive technology (COPAC)143 or CCO123 should be considered.
The pulse contour measurement of CO is strongly influenced by factors independent of true changes in CO such as those affecting the arterial pressure (e.g., vascular tone, compliance, and the arterial site).24 Further validation studies, particularly covering a wide CO range, are required147 to assess the reliability of the currently implemented algorithms which tend to either under- or overcompensate for prominent increases (or decreases) in vascular tone and compliance. The algorithms implemented in these devices are primarily based on the model described by Wesseling.100 Besides age, sex, and body mass index, this model is based on a strict mathematical relationship between (aortic) compliance and pressure and can hardly take into account real changes in vessel compliance due to vasoactive drugs or mediators. This rather inflexible model will fail during hemodynamic instability. The deficiency in the model can be compensated by repeated calibration. To date, studies are lacking that explicitly provide the calibration intervals needed to maintain the accuracy of the COPCA measurements. This information would be helpful for proper analysis, particularly since the producers of semi-invasive monitoring systems market them as having signal stability over time.
Physicians should keep in mind the limitations of these technologies, especially in unstable critically ill patients. Although a recent study concluded that only 39% of patients undergoing surgical procedures met the criteria for semi-invasive hemodynamic monitoring,148 COPCA systems may have their place in postoperative intensive care medicine when the administration of fluids and vasopressors is guided to specific therapeutic endpoints (“goal-directed therapy”). Nevertheless, only a few studies showed reduced mortality and morbidity149,150 or reduced length of hospital stay151,152 (but not reduced ICU stay)152 when hemodynamic monitoring and therapy were coordinated.
Positive reports on the clinical suitability of presently available semi-invasive pulse contour systems for continuous CO measurement are increasingly found in the literature. These systems are gaining in popularity despite the fact that the measured CO in various clinical situations shows only limited agreement with intermittent bolus TD. Further improvements and validation studies are required. There is also a need to show whether there is a resulting healthcare benefit if these monitors are used in regular clinical practice. In the interim, the physician should be aware of the inaccuracy of currently available CO monitoring devices based on PCA and should not be guided solely by CO data. The physician providing care must also adhere to a hemodynamic optimization strategy that includes all relevant clinical parameters for secure therapeutic decision-making.
Notes
Hatib F, Roteliuk L, Pearce J (inventors). Pulse contour method and apparatus for continuous assessment of a cardiovascular parameter. International patent publication WO 2006/113337 A2, 2006 Oct. 26.
Roteliuk L (inventor). Arterial pressure-based automatic determination of a cardiovascular parameter. International patent publication WO2005/055825 A1, 2005 June 23.
LiDCO Ltd. User’s Manual LiDCO Rapid-Fluid management just got easier. http://www.lidcorapid.co.uk/pdfs/english-rapid-v1.04-user-manual.pdf (accessed February 2014).
Edwards. Lifesciences Inc. FloTrac System 3rd Generation Software. Available from URL: http://www.edwards.com/eu/products/mininvasive/Pages/flotrac3g.aspx (accessed February 2014).
Edwards. FloTrac Sensor. Available from URL: http://ht.edwards.com/scin/edwards/sitecollectionimages/products/mininvasive/flotracbrochurear05917.pdf (accessed February 2014).
Edwards Lifesciences Inc. EV1000 Clinical Platform 510(k) Summary. Available from URL: http://www.accessdata.fda.gov/cdrh_docs/pdf10/K100709.pdf (accessed February 2014).
Joeken S, Fahle M, Pfeiffer UJ (inventors). Devices for in-vivo determination of the compliance function and the systemic blood flow of a living being. US patent US 6315735 B1.
Band DM, Linton RA, O’Brien TK (inventors). Method and apparatus for the measurement of cardiac output. International patent publication WO 97/24982 A.
Band MS, Linton WM, Linton RA, O’Brien KT (inventors). Verfahren und Vorrichtung zum Messen der Herzleistung. DE patent 697 23 847 T2. 2004 Jun. 03.
Romano S (inventor). Method and apparatus for measuring cardiac output. US patent US 6758822 B2.
References
Koo KK, Sun JC, Zhou Q, et al. Pulmonary artery catheters: evolving rates and reasons for use. Crit Care Med 2011; 39: 1613-8.
Sandham JD, Hull RD, Brant RF, et al. Canadian Critical Care Clinical Trials Group: a randomized, controlled trial of the use of pulmonary-artery catheters in high-risk surgical patients. N Engl J Med 2003; 348: 5-14.
Evans DC, Doraiswamy VA, Prosciak MP, et al. Complications associated with pulmonary artery catheters: a comprehensive clinical review. Scand J Surg 2009; 98: 199-208.
Connors AF, Speroff T, Dawson NV, et al. The effectiveness of right heart catheterization in the initial care of critically ill patients. JAMA 1996; 276: 889-97.
Schwann NM, Hillel Z, Hoeft A, et al. Lack of effectiveness of the pulmonary artery catheter in cardiac surgery. Anesth Analg 2011; 113: 994-1002.
Rajaram SS, Desai NK, Kalra A, et al. Pulmonary artery catheters for adult patients in intensive care. Cochrane Database Syst Rev 2013; 2: CD003408.
Balk E, Raman G, Chung M, et al. Evaluation of the evidence on benefits and harmfulness of pulmonary artery catheter use in critical care settings. Agency for Healthcare Research and Quality. 2008. Available from URL: http://www.cms.gov/Medicare/Coverage/DeterminationProcess/downloads/id55TA.pdf (accessed 26 November 2013).
Benington S, Ferris P, Nirmalanc M. Emerging trends in minimally invasive haemodynamic monitoring and optimization of fluid therapy. Eur J Anaesth 2009; 26: 893-905.
Campos MML, Sellés FA, de Vera GG, et al. Techniques available for hemodynamic monitoring. Advantages and limitations. Med Intensiva 2012; 36: 434-44.
Drummond KE, Murphy M. Minimally invasive cardiac output monitors. Continuing Education in Anaesthesia, Crit Care Pain 2012; 12: 5-10.
Litton E, Morgan M. The PiCCO Monitor: a review. Anaesth Intensive Care 2012; 40: 393-409.
Frank O. Die Grundform des arteriellen Pulses. Erste Abhandlung. Mathematische Analyse. Zeitschrift für Biologie 1899; 37: 485-526.
Erlanger J, Hooker DR. An experimental study of blood pressure and of pulse pressure in man. John Hopkins Hospital Records 1904; 12: 145-378.
Rhodes A, Sunderland R. Arterial pulse power analysis: the LiDCO™ plus system. In: Pinsky MR, Payen D, editors. Functional Hemodynamic Monitoring-Update in Intensive Care and Emergency Medicine 42. Berlin, Heidelberg: Springer; 2005. p. 183-92.
Maus TM, Lee DE. Arterial pressure-based cardiac output assessment. J Cardiothorac Vasc Anesth 2008; 22: 468-73.
Romagnoli S, Romano SM, Bevilacqua S, et al. Dynamic response of liquid-filled catheter systems for measurement of blood pressure: precision of measurements and reliability of the pressure recording analytical method with different disposable systems. J Crit Care 2011; 26: 415-22.
Thiele RH, Durieux ME. Arterial waveform analysis for the anesthesiologist: past, present, and future concepts. Anesth Analg 2011; 113: 766-76.
Alhashemi JA, Cecconi M, Hofer CK. Cardiac output monitoring: an integrative perspective. Crit Care 2011; 15: 214.
Morgan P, Al-Subaie N, Rhodes A. Minimally invasive cardiac output monitoring. Curr Opin Crit Care 2008; 14: 322-6.
Funk DJ, Moretti EW, Gan TJ. Minimally invasive cardiac output monitoring in the perioperative setting. Anesth Analg 2009; 108: 887-97.
de Wilde RBP, Schreuder JJ, van den Berg PC, Jansen JR. An evaluation of cardiac output by five arterial pulse contour techniques during cardiac surgery. Anaesthesia 2007; 62: 760-8.
Mayer J, Boldt J, Poland R, et al. A continuous arterial pressure waveform-based cardiac output using the FloTrac/Vigileo: a review and meta-analysis. J Cardiothorac Vasc Anesth 2009; 23: 401-6.
Peyton PJ, Chong SW. Minimally invasive measurement of cardiac output during surgery and critical care: a meta-analysis of accuracy and precision. Anesthesiology 2010; 113: 1220-35.
Camporota L, Beale R. Pitfalls in haemodynamic monitoring based on the arterial pressure waveform. Crit Care 2010; 14: 124.
Marik PE. Noninvasive Cardiac Output Monitors: a State-of the-Art Review. J Cardiothorac Vasc Anesth 2013; 27: 121-34.
Montenij LJ, de Waal EE, Buhre WF. Arterial waveform analysis in anesthesia and critical care. Curr Opin Anaesthesiol 2011; 24: 651-6.
Stover JF, Stocker R, Lenherr R, et al. Noninvasive cardiac output and blood pressure monitoring cannot replace an invasive monitoring system in critically ill patients. BMC Anesthesiol 2009; 9: 6.
Bogert LW, Wesseling KH, Schraa O, et al. Pulse contour cardiac output derived from non-invasive arterial pressure in cardiovascular disease. Anaesthesia 2010; 65: 1119-25.
Hohn A, Defosse JM, Becker S, Steffen C, Wappler F, Sakka SG. Non-invasive continuous arterial pressure monitoring with Nexfin® does not sufficiently replace invasive measurements in critically ill patients. Br J Anaesth 2013; 111: 178-84.
Critchley LA, Critchley JA. A meta-analysis of studies using bias and precision statistics to compare cardiac output measurement techniques. J Clin Monit Comput 1999; 15: 85-91.
Hunter JE, Schmidt FL. Methods of Meta-analysis: correcting error and Bias in Research Findings. 2nd ed. Newbury Park, CA: Sage; 2004: 89.
Gruenewald M, Renner J, Meybohm P, Hocker J, Scholz J, Bein B. Reliability of continuous cardiac output measurement during intra-abdominal hypertension relies on repeated calibrations: an experimental animal study. Critical Care 2008; 12: R132.
Gruenewald M, Meybohm P, Renner J, et al. Effect of norepinephrine dosage and calibration frequency on accuracy of pulse contour-derived cardiac output. Crit Care 2011; 15: R22.
Rodig G, Prasser C, Keyl C, Liebold A, Hobbhahn J. Continuous cardiac output measurement: pulse contour analysis vs TD technique in cardiac surgical patients. Br J Anaesth 1999; 82: 525-30.
Godje O, Höke K, Goetz AE, et al. Reliability of a new algorithm for continuous cardiac output determination by pulse-contour analysis during hemodynamic instability. Crit Care Med 2002; 30: 52-8.
Sujatha P, Mehta Y, Dhar A, Sarkar D, Meharwal ZS, Trehan N. Comparison of cardiac output in OPCAB: bolus thermodilution technique versus pulse contour analysis. Ann Card Anaesth 2006; 9: 44-8.
McGee WT, Horswell JL, Calderon J, et al. Validation of a continuous, arterial pressure-based cardiac output measurement: a multicenter, prospective clinical trial. Crit Care 2007; 11: R105.
Zimmermann A, Kufner C, Hofbauer S, et al. The accuracy of the Vigileo/FloTrac continuous cardiac output monitor. J Cardiothorac Vasc Anesth 2008; 22: 388-93.
Sander M, Spies CD, Grubitzsch H, Foer A, Muller M, von Heymann C. Comparison of uncalibrated arterial waveform analysis in cardiac surgery patients with thermodilution cardiac output measurements. Crit Care 2006; 10: R164.
Opdam HI, Wan L, Bellomo R. A pilot assessment of the FloTrac™ cardiac output monitoring system. Intensive Care Med 2007; 33: 344-9.
Prasser C, Bele S, Keyl C, et al. Evaluation of a new pressure-based cardiac output device requiring no external calibration. BMC Anesthesiol 2007; 7: 9.
Cecconi M, Dawson D, Casaretti R, Grounds RM, Rhodes A. A prospective study of the accuracy and precision of continuous cardiac output monitoring devices as compared to intermittent thermodilution. Minerva Anestesiol 2010; 76: 1010-7.
Manecke GR Jr, Auger WR. Cardiac output determination from the arterial pressure wave: clinical testing of a novel algorithm that does not require calibration. J Cardiothorac Vasc Anesth 2007; 21: 3-7.
Breukers RM, Sepehrkhouv S, Spiegelenberg SR, Groeneveld J. Cardiac output measured by a new arterial pressure waveform analysis method without calibration compared with thermodilution after cardiac surgery. J Cardiothorac Vasc Anesth 2007; 21: 632-5.
Senn A, Button D, Zollinger A, Hofer CK. Assessment of cardiac output changes using a modified FloTrac/Vigileo™ algorithm in cardiac surgery patients. Crit Care 2009; 13: R32.l.
Chakravarthy M, Jayaprakash K, Kalligudd P, Prabhakumar D, Jawali V. Comparison of simultaneous estimation of cardiac output by four techniques in patients undergoing off-pump coronary artery bypass surgery—a prospective observational study. Ann Card Anaesth 2007; 10: 121-6.
Button D, Weibel L, Reutehbuch O, Genoni M, Zollinger A, Hofer CK. Clinical evaluation of the FloTrac/Vigileo™ system and two established continuous cardiac output monitoring devices in patients undergoing cardiac surgery. Br J Anaesth 2007; 99: 329-36.
Mehta Y, Kumar R, Sawhney R, Bhise M, Singh A, Trehan N. Cardiac output monitoring: comparison of a new arterial pressure waveform analysis to the bolus thermodilution technique in patients undergoing off-pump coronary artery bypass surgery. J Cardiothorac Vasc Anesth 2008; 22: 394-9.
Prasser C, Trabold B, Schwab A, Keyl C, Ziegler S, Wiesenack C. Evaluation of an improved algorithm for arterial pressure-based cardiac output assessment without external calibration. Intensive Care Med 2007; 33: 2223-5.
Della Rocca G, Costa MG, Chiarandini P, et al. Arterial pulse cardiac output agreement with thermodilution in patients in hyperdynamic conditions. J Cardiothorac Vasc Anesth 2008; 22: 681-7.
De Backer D, Marx G, Tan A, et al. Arterial pressure-based cardiac output monitoring: a multicenter validation of the third-generation software in septic patients. Intensive Care Med 2011; 37: 233-40.
Zimmermann A, Steinwendner J, Hofbauer S, et al. The accuracy of the Vigileo/FloTrac system has been improved-follow-up after a software update: a blinded comparative study of 30 cardiosurgical patients. J Cardiothorac Vasc Anesth 2009; 23: 929-31.
Cannesson M, Attof Y, Rosamel P, Joseph P, Bastien O, Lehot JJ. Comparison of FloTrac™ cardiac output monitoring system in patients undergoing coronary artery bypass grafting with pulmonary artery cardiac output measurements. Eur J Anaesthesiol 2007; 24: 832-9.
Staier K, Wiesenack C, Günkel L, Keyl C. Cardiac output determination by thermodilution and arterial pulse waveform analysis in patients undergoing aortic valve replacement. Can J Anesth 2008; 55: 22-8.
Hofer CK, Button D, Weibel L, Genoni M, Zollinger A. Uncalibrated radial and femoral arterial pressure waveform analysis for continuous cardiac output measurement: an evaluation in cardiac surgery patients. J Cardiothorac Vasc Anesth 2010; 24: 257-64.
Vetrugno L, Costa MG, Spagnesi L, et al. Uncalibrated arterial pulse cardiac output measurements in patients with moderately abnormal left ventricular function. J Cardiothorac Vasc Anesth 2011; 25: 53-8.
Maxeiner H, Wenzel S, Weigand MA, Mueller M. Cardiac output measured by FloTrac/Vigileo system: does the “plug and play” principle work? Applied Cardiopulmonary Pathophysiology 2010; 14: 131-8.
Biais M, Nouette-Gaulain K, Cottenceau V, et al. Cardiac output measurement in patients undergoing liver transplantation: pulmonary artery catheter versus uncalibrated arterial pressure waveform analysis. Anesth Analg 2008; 106: 1480-6.
Slagt C, Beute J, Hoeksema M, Malagon I, Mulder JW, Groeneveld JA. Cardiac output derived from arterial pressure waveform analysis without calibration vs. thermodilution in septic shock: evolving accuracy of software versions. Eur J Anaesthesiol 2010; 27: 550-4.
Schramm S, Albrecht E, Frascarolo P, Chassot PG, Spahn DR. Validity of an arterial pressure waveform analysis device: does the puncture site play a role in the agreement with intermittent pulmonary artery catheter TD measurements? J Cardiothorac Vasc Anesth 2010; 24: 250-6.
Saraceni E, Rossi S, Persona P, et al. Comparison of two methods for cardiac output measurement in critically ill patients. Br J Anaesth 2011; 106: 690-4.
Biancofiore G, Critchley LA, Lee A, et al. Evaluation of an uncalibrated arterial pulse contour cardiac output monitoring system in cirrhotic patients undergoing liver surgery. Br J Anaesth 2009; 102: 47-54.
Krejci V, Vannucci A, Abbas A, Chapman W, Kangrga IM. Comparison of calibrated and uncalibrated arterial pressure-based cardiac output monitors during orthotopic liver transplantation. Liver Transpl 2010; 16: 773-82.
Junttila EK, Koskenkari JK, Ohtonen PP, Ala-Kokko TI. Uncalibrated arterial pressure waveform analysis for cardiac output monitoring is biased by low peripheral resistance in patients with intracranial haemorrhage. Br J Anaesth 2011; 107: 581-6.
Tsai YF, Su BC, Lin CC, Liu FC, Lee WC, Yu HP. Cardiac Output derived from arterial pressure waveform analysis: validation of the third-generation software in patients undergoing orthotopic liver transplantation. Transplant Pro 2012; 44: 433-7.
Biancofiore G, Critchley LA, Lee A, et al. Evaluation of a new software version of the FloTrac/Vigileo (Version 3.02) and a comparison with previous data in cirrhotic patients undergoing liver transplant surgery. Anesth Analg 2011; 113: 515-22.
Slagt C, de Leeuw MA, Beute J, et al. Cardiac output measured by uncalibrated arterial pressure waveform analysis by recently released software version 3.02 versus thermodilution in septic shock. J Clin Monit Comput 2013; 27: 171-7.
Vasdev S, Chauhan S, Choudhury M, Hote MP, Malik M, Kiran U. Arterial pressure waveform derived cardiac output FloTrac/Vigileo system (third generation software): comparison of two monitoring sites with the thermodilution cardiac output. J Clin Monit Comput 2012; 26: 115-20.
Akiyoshi K, Kandabashi T, Kaji J, et al. Accuracy of arterial pressure waveform analysis for cardiac output measurement in comparison with thermodilution methods in patients undergoing living donor liver transplantation. J Anesth 2011; 25: 178-83.
Eleftheriadis S, Galatoudis Z, Didilis V, et al. Variations in arterial blood pressure are associated with parallel changes in FlowTrac/Vigileo®-derived cardiac output measurements: a prospective comparison study. Crit Care 2009; 13: R179.
Hadian M, Kim HK, Severyn DA, Pinsky MR. Cross-comparison of cardiac output trending accuracy of LiDCO, PiCCO, FloTrac and pulmonary artery catheters. Crit Care 2010; 14: R212.
Buhre W, Weyland A, Kazmaier S, Hanekop, et al. Comparison of cardiac output assessed by pulse-contour analysis and TD in patients undergoing minimally invasive direct coronary artery bypass grafting. J Cardiothorac Vasc Anesth 1999; 13: 437-40.
Zollner C, Haller M, Weis M, et al. Beat-to-beat measurement of cardiac output by intravascular pulse contour analysis: a prospective criterion standard study in patients after cardiac surgery. J Cardiothorac Vasc Anesthesia 2000; 14: 125-9.
Hamzaoui O, Monnet X, Richard C, Osman D, Chemla D, Teboul JL. Effects of changes in vascular tone on the agreement between pulse contour and transpulmonary TD cardiac output measurements within an up to 6-hour calibration-free period. Crit Care Med 2008; 36: 434-40.
Bein B, Meybohm P, Cavus E, et al. The reliability of pulse contour-derived cardiac output during hemorrhage and after vasopressor administration. Anesth Analg 2007; 105: 107-13.
Staier K, Wilhelm M, Wiesenack Ch, et al. Pulmonary artery vs. transpulmonary thermodilution for the assessment of cardiac output in mitral regurgitation: a prospective observational study. Eur J Anaesthesiol 2012; 29: 431-7.
Tzenkov IG, Velasco DA, Perez Pena JM, Olmedilla Arnal L, Garutti Martınez I, Sanz Fernandez J. Cardiac output by femoral arterial thermodilution-calibrated pulse contour analysis during liver transplantation: comparison with pulmonary artery thermodilution. Transplant Proc 2003; 35: 1920-2.
Wouters PF, Quaghebeur B, Sergeant P, Van Hemelrijck J, Vandermeersch E. Cardiac output monitoring using a brachial arterial catheter during off-pump coronary artery bypass grafting. J Cardiothorac Vasc Anesth 2005; 2: 160-4.
Rauch H, Müller M, Fleischer F, Bauer H, Martin E, Bottiger BW. Pulse contour analysis versus thermodilution in cardiac output surgery patients. Acta Anaesthesiol Scand 2002; 46: 424-9.
Mielck F, Buhre W, Hanekop G, Tirilomis T, Hilgers R, Sonntag H. Comparison of continuous cardiac output measurements in patients after cardiac surgery. J Cardiothorac Vasc Anesth 2003; 17: 211-6.
Halvorsen PS, Sokolov A, Cvancarova M, Hol PK, Lundblad R, Tonnessen TI. Continuous cardiac output during off-pump coronary artery bypass surgery: pulse contour analysis vs pulmonary artery thermodilution. Br J Anaesth 2007; 99: 484-92.
Sander M, von Heymann C, Foer A, et al. Pulse contour analysis after normothermic cardiopulmonary bypass in cardiac surgery patients. Crit Care 2005; 9: R729.
Ostergard M, Nielsen J, Rasmussen JP, Berthelsen PG. Cardiac output – pulse contour analysis vs. pulmonary artery thermodilution. Acta Anaesthesiol Scand 2006; 50: 1044-9.
Della Rocca G, Costa MG, Coccia C, et al. Cardiac output monitoring: aortic transpulmonary thermodilution and pulse contour analysis agree with standard thermodilution methods in patients undergoing lung transplantation. Can J Anesth 2003; 50: 707-11.
Yamashita K, Nishiyama T, Yokoyama T, Abe H, Manabe M. The effects of vasodilation on cardiac output measured by PiCCO. J Cardiothorac Vasc Anesth 2008; 22: 688-92.
Della Rocca G, Costa MG, Pompei L, Coccia C, Pietropaoli P. Continuous and intermittent cardiac output measurement: pulmonary artery catheter versus aortic transpulmonary technique. Br J Anaesth 2002; 88: 350-6.
Irlbeck M, Forst H, Briegel J, Haller M, Peter K. Continuous measurement of cardiac output with pulse contour analysis. Anaesthesist 1995; 44: 493-500.
Felbinger TW, Reuter DA, Eltzschig HK, Moerstedt K, Goedje O, Goetz AE. Comparison of pulmonary arterial TD and arterial pulse contour analysis: evaluation of a new algorithm. J Clin Anesth 2002; 14: 296-301.
Goedje O, Hoeke K, Lichtwarck-Aschoff M, Faltchauser A, Lamm P, Reichart B. Continuous cardiac output by femoral arterial thermodilution calibrated pulse contour analysis: comparison with pulmonary arterial thermodilution. Crit Care Med 1999; 27: 2407-12.
Linton R, Band D, O’Brien T, Jonas M, Leach R. Lithium dilution cardiac output measurement: a comparison with TD. Crit Care Med 1997; 25: 1796-800.
Garcia-Rodriquez C, Pittman J, Cassell C, et al. Lithium dilution cardiac output measurement: a clinical assessment of central venous and peripheral venous indicator injection. Crit Care Med 2002; 30: 2199-204.
Hamilton TT, Huber LM, Jessen ME. PulseCO: a less-invasive method to monitor cardiac output from arterial pressure after cardiac surgery. Ann Thorac Surg 2002; 74: 1408-12.
Mora B, Ince I, Birkenberg B, et al. Validation of cardiac output measurement with the LiDCOTM pulse contour system in patients with impaired left ventricular function after cardiac surgery. Anaesthesia 2011; 66: 675-81.
Costa MG, Della Rocca G, Chiarandini P, et al. Continuous and intermittent cardiac output measurement in hyperdynamic conditions: pulmonary artery catheter vs. lithium dilution technique. Intensive Care Med 2008; 34: 257-63.
Dyer RA, Piercy JL, Reed AR, et al. Comparison between pulse waveform analysis and thermodilution cardiac output determination in patients with severe pre-eclampsia. Br J Anaesth 2011; 106: 77-81.
Missant C, Rex S, Wouters PF. Accuracy of cardiac output measurements with pulse contour analysis (PulseCOTM) and Doppler echocardiography during off-pump coronary artery bypass grafting. Eur J Anaesthesiol 2008; 25: 243-8.
Yamashita K, Nishiyama T, Yokoyama T, Abe H, Manabe M. Cardiac output by PulseCO is not interchangeable with thermodilution in patients undergoing OPCAB. Can J Anesth 2005; 52: 530-4.
Nissen P, Van Lieshout JJ, Novovic S, Bundgaard-Nielsen M, Secher NH. Techniques of cardiac output measurement during liver transplantation: arterial pulse wave versus thermodilution. Liver Transpl 2009; 15: 287-91.
Jansen JRC, Schreuder JJ, Mulier JP, Smith NT, Settels JJ, Wesseling KH. A comparison of cardiac output derived from the arterial pressure wave against thermodilution in cardiac surgery patients. Br J Anaesth 2001; 87: 212-22.
Wesseling KH, Jansen JRC, Settels JJ, Schreuder JJ. Computation of aortic flow from pressure in humans using a nonlinear, three-element model. J Appl Physiol 1993; 74: 2566-73.
Jellema WT, Wesseling KH, Groeneveld AB, Stoutenbeek CP, Thijs LG, van Lieshout JJ. Continuous cardiac output in septic shock by simulating a model of the aortic input impedance. Anesthesiology 1999; 90: 1317-28.
de Vaal HB, de Wilde RB, van den Berg PC, Schreuder JJ, Jansen JR. Less invasive determination of cardiac output from the arterial pressure by aortic diameter-calibrated pulse contour. Br J Anaesth 2005; 95: 326-31.
Hirschl MM, Kittler H, Woisetschlager C, et al. Simultaneous comparison of thoracic bioimpedance and arterial pulse waveform-derived cardiac output with thermodilution measurement. Crit Care Med 2000; 28: 1798-802.
Romano SM, Pistolesi M. Assessment of cardiac output from systemic arterial pressure in humans. Crit Care Med 2002; 30: 1834-41.
Romano SM, Conti AA, Giglioli C, et al. Blood flow assessment by arterial pressure wave without external calibration. Computers in Cardiology 2006; 33: 293-6.
Giomarelli P, Biagioli B, Scolletta S. Cardiac output monitoring by pressure recording analytical method in cardiac surgery. Eur J Cardiothorac Surg 2004; 26: 515-20.
Romano SM, Scolletta S, Olivotto I, et al. Systemic arterial waveform analysis and assessment of blood flow during extracorporeal circulation. Perfusion 2006; 21: 109-16.
Zangrillo A, Maj G, Monaco F, et al. Cardiac index validation using the pressure recording analytic method in unstable patients. J Cardiothorac Vasc Anesth 2010; 24: 265-9.
Scolletta S, Franchi F, Taccone FS, Donadello K, Biagioli B, Vincent JL. An uncalibrated pulse contour method to measure cardiac output during aortic counterpulsation. Anesth Analg 2011; 113: 1389-95.
Franchi F, Silvestri R, Cubattoli L, et al. Comparison between an uncalibrated pulse contour method and thermodilution technique for cardiac output estimation in septic patients. Br J Anaesth 2011; 107: 202-8.
Paarmann H, Groesdonk HW, Sedemund-Adib B, Hanke T, Heinze H, Heringlake M. Lack of agreement between pulmonary arterial thermodilution cardiac output and the pressure recording analytical method in postoperative cardiac surgery patients. Br J Anaesth 2011; 106: 475-81.
Maj G, Monaco F, Landoni G, et al. Cardiac index assessment by the pressure recording analytic method in unstable patients with atrial fibrillation. J Cardiothorac Anesth 2011; 25: 476-80.
Belda FJ, Aguilar G, Teboul JL, et al. Complications related to less-invasive haemodynamic monitoring. Br J Anaesth 2011; 106: 482-6.
Reuter DA, Huang C, Edrich T, Shernan SK, Eltzschig HK. Cardiac output monitoring using indicator-dilution techniques: basics, limits, and perspectives. Anesth Analg 2010; 110: 799-811.
Richard C, Monnet X, Teboul JL. Pulmonary artery catheter monitoring in 2011. Current Opinion in Critical Care 2011; 17: 296-302.
van Grondelle A, Ditchey RV, Groves BM, Wagner WW, Reeves JT. Thermodilution method overestimates low cardiac output in humans. Am J Physiol 1983; 245: H690-2.
Nishikawa T, Dohi S. Errors in the measurement of cardiac output by thermodilution. Can J Anaesth 1993; 40: 142-53.
Jansen JR, Schreuder JJ, Bogaard JM, van Rooyen W, Versprille A. The thermodilution technique for measurement of cardiac output during artificial ventilation. J Appl Physiol 1981; 51: 584-91.
Bazaral MG, Petre J, Novoa R. Errors in TD cardiac output measurements caused by rapid pulmonary artery temperature decreases after cardiopulmonary bypass. Anesthesiology 1992; 77: 31-7.
Jansen JR, Schreuder JJ, Punt KD, van den Berg PC, Alfieri O. Mean cardiac output by thermodilution with a single controlled injection. Crit Care Med 2001; 29: 1868-73.
Nilsson LB, Nilsson JC, Skovgaard LT, Berthelsen PG. Thermodilution cardiac output — are three injections enough? Acta Anaesthesiol Scand 2004; 48: 1322-7.
Yang X-X, Critchley LA, Joynt GM. Determination of the precision error of the pulmonary artery thermodilution catheter using an in vitro continuous flow test rig. Anesth Analg 2011; 112: 70-7.
Marque S, Gros A, Chimot L, et al. Cardiac output monitoring in septic shock: evaluation of the third-generation Flotrac-Vigileo. J Clin Monit Comput 2013; 27: 273-9.
Cecconi M, Rhodes A, Poloniecki J, Della Rocca G, Grounds RM. Bench-to-bedside review: the importance of the precision of the reference technique in method comparison studies—with specific reference to the measurement of cardiac output. Crit Care 2009; 13: 201.
Hamilton C, Stamey J. Using Bland Altman to assess agreement between two medical devices! J Clin Monit Comput 2007; 21: 331-3.
Hamm JB, Nguyen BV, Kiss G, et al. Assessment of a cardiac output device using arterial pulse waveform analysis, Vigileo, in cardiac surgery compared to pulmonary arterial TD. Anaesth Intensive Care 2010; 38: 295-301.
Jeong YB, Kim TH, Roh YJ, Choi IC, Suh JH. Comparison of uncalibrated arterial pressure waveform analysis with continuous thermodilution cardiac output measurements in patients undergoing elective off-pump coronary artery bypass surgery. J Cardiothorac Vasc Anesth 2010; 5: 767-71.
Haenggi M, Barthelmes D, Ulmer H, Takala J, Jakob SM. Comparison of non-calibrated pulse-contour analysis with continuous thermodilution for cardiac output assessment in patients with induced hypothermia after cardiac arrest. Resuscitation 2011; 82: 423-6.
Jo YY, Song JW, Yoo YC, Park JY, Shim JK, Kwak YL. The uncalibrated pulse contour cardiac output during offpump coronary bypass surgery: performance in patients with a low cardiac output status and a reduced left ventricular function. Korean J Anesthesiol 2011; 60: 237-43.
Su BC, Tsai YF, Chen CY, et al. Cardiac output derived from arterial pressure waveform analysis in patients undergoing liver transplantation: validity of a third-generation device. Transplant Proc 2012; 44: 424-8.
Monnet X, Anguel N, Jozwiak M, Richard C, Teboul JL. Third-generation FloTrac/Vigileo does not reliably track changes in cardiac output induced by norepinephrine in critically ill patients. Br J Anaesth 2012; 108: 615-22.
Metzelder S, Coburn M, Fries M, Reinges et al. Performance of cardiac output measurement derived from arterial pressure waveform analysis in patients requiring high-dose vasopressor therapy. Br J Anaesth 2011; 106: 776-84.
Monnet X, Anguel N, Naudin B, Jabot J, Richard C, Teboul JL. Arterial pressure-based cardiac output in septic patients: different accuracy of pulse contour and uncalibrated pressure waveform devices. Crit Care 2010; 14: R109.
Chatti R, de Rudniki S, Marque S, et al. Comparison of two versions of the Vigileo-FloTrac system (1.03 and 1.07) for stroke volume estimation: a multicentre, blinded comparison with oesophageal Doppler measurements. Br J Anaesth 2009; 102: 463-9.
Broch O, Renner J, Hocker J, et al. Uncalibrated pulse power analysis fails to reliably measure cardiac output in patients undergoing coronary artery bypass surgery. Crit Care 2011; 15: R76.
McCoy JV, Hollenberg SM, Dellinger RB, et al. Continuous cardiac index monitoring: a prospective observational study of agreement between a pulmonary artery catheter and a calibrated minimally invasive technique. Resuscitation 2009; 80: 893-7.
Reisner AT, Xu D, Ryan KL, Convertino VA, Rickards CA, Mukkamala R. Monitoring non-invasive cardiac output and stroke volume during experimental human hypovolaemia and resuscitation. Br J Anaesth 2011; 106: 23-30.
Singh S, Taylor MA. Con: the FloTrac device should not be used to follow cardiac output in cardiac surgical patients. J Cardiothorac Vasc Anesth 2010; 4: 709-11.
Ambrisko TD, Coppens P, Kabes R, Moens Y. Lithium dilution, pulse power analysis, and continuous thermodilution cardiac output measurements compared with bolus thermodilution in anaesthetized ponies. Br J Anaesth 2012; 109: 864-9.
Ambrisko TD, Kabes R, Moens Y. Influence of drugs on the response characteristics of the LiDCO sensor: an in vitro study. Br J Anaesth 2013; 110: 305-10.
Critchley LA, Lee A, Ho A. A critical review of the ability of continuous cardiac output monitors to measure trends in cardiac output. Anesth Analg 2010; 111: 1180-92.
Suehiro K, Tanaka K, Funao T, et al. Systemic vascular resistance has an impact on the reliability of the Vigileo-FloTrac system in measuring cardiac output and tracking cardiac output changes. Br J Anaesth 2013; 111: 170-7.
Chikhani M, Moppett IK. Minimally invasive cardiac output monitoring: what evidence do we need? Br J Anaesth 2011; 106: 451-3.
Geerts B, de Wilde R, Aarts L, Jansen J. Pulse contour analysis to assess hemodynamic response to passive leg raising. J Cardiothorac Vasc Anesth 2011; 25: 48-52.
Squara P, Cecconi M, Rhodes M, Singer M, Chiche JD. Tracking changes in cardiac output: methodological considerations for the validation of monitoring devices. Intensive Care Med 2009; 35: 1801-8.
Critchley LA, Yang XX, Lee A. Assessment of trending ability of cardiac output monitors by polar plot methodology. J Cardiothorac Vasc Anesth 2011; 25: 536-46.
Critchley LA. Self-calibrating pulse contour cardiac output: do validation studies really show its clinical reliability? Crit Care 2009; 13: 123.
Maquire S, Rinehart J, Vakharia S, Cannesson M. Respiratory variation in pulse pressure and plethysmographic waveform: intraoperative applicability in a North American academic center. Anesth Analg 2011; 112: 94-6.
Hamilton MA, Cecconi M, Rhodes A. A systematic review and meta-analysis on the use of preemptive hemodynamic intervention to improve postoperative outcomes in moderate and high-risk surgical patients. Anesth Analg 2011; 112: 1392-402.
Scheeren TW, Wiesenack C, Gerlach H, Marx G. Goal-directed intraoperative fluid therapy guided by stroke volume and its variation in high-risk surgical patients: a prospective randomized multicentre. J Clin Monit Comput 2013; 27: 225-33.
Pearse R, Dawson D, Fawcett J, Rhodes A, Grounds RM, Bennett ED. Early goal-directed therapy after major surgery reduces complications and duration of hospital stay. A randomised, controlled trial [ISRCTN38797445]. Crit Care 2005; 9: R687-93.
Mayer J, Boldt J, Mengistu AM, Rohm KD, Suttner S. Goal-directed intraoperative therapy based on autocalibrated arterial pressure waveform analysis reduces hospital stay in high-risk surgical patients: a randomized, controlled trial. Crit Care 2010; 14: R18.
Manecke GR. Edwards FloTrac® sensor and Vigileo® monitor: easy, accurate, reliable cardiac output assessment using the arterial pulse wave. Expert Rev Med Devices 2005; 2: 523-7.
Boulain T, Achard JM, Teboul JL, Richard C, Perrotin D, Ginies G. Changes in BP induced by passive leg raising predict response to fluid loading in critically ill patients. Chest 2002; 121: 1245-52.
Cecconi M, Wilson J, Rhodes A. Pulse pressure analysis. In: Vincent JL, editor. I Yearbook of Intensive Care and Emergency Medicine. Berlin/Heidelberg/New York: Springer; 2006. p. 176-83.
Langewouters GJ, Wesseling KH, Goedhard WJ. The pressure dependent dynamic elasticity of 35 thoracic and 16 abdominal human aortas in vitro described by a five component model. J Biomech 1985; 18: 613-20.
Wesseling KH, Smith NT, Nichols WW, Weber H, de Wit B, Beneken JE. Beat-to-beat cardiac output from the arterial pressure pulse contour. In: Feldman SA, Leigh JM, Spierdijk J, editors. Measurement in Anaesthesia. Leiden: Leiden University Press; 1974: 148-64.
Wesseling KH, de Wit B, Smith NT. A simple device for the continuous measurement of cardiac output. Adv Cardiovasc Phys 1983; 5: 16-52.
Jansen JR, van den Berg PC. Cardiac Output by thermodilution and arterial pulse contour techniques. In: Pinsky MR, Payen D, editors. Functional Hemodynamic Monitoring-Update in Intensive Care and Emergency Medicine 42. Berlin Heidelberg: Springer; 2005: 135-52.
Jonas MM, Tanser SJ. Lithium dilution measurement of cardiac output and arterial pulse waveform analysis: an indicator dilution calibrated beat-by-beat system for continuous estimation of cardiac output. Curr Opin Crit Care 2002; 8: 257-61.
Jonas MM, Hett D, Morgan J. Real time, continuous monitoring of cardiac output and oxygen delivery. Int J Intensive Care 2002; 9: 1-6.
Langewouters GJ, Wesseling KH, Goedhard WJ. The static elastic properties of 45 human thoracic and 20 abdominal aortas in vitro and the parameters of a new model. Journal Biomech 1984; 17: 425-35.
Bogert LWJ, Lieshout JJ. Non-invasive pulsatile arterial pressure and stroke volume changes from the human finger. Exp Physiol 2005; 90: 437-46.
Messiah A. Change of representation and perturbation treatment of a part of the Hamiltonian. In: Messiah A (Ed). Quantum Mechanics. Amsterdam: North Holland Physics Publishing; 1985; 2: 722-60.
Scolletta S, Romano SM, Biagioli B, Capannini G, Giomarelli P. Pressure recording analytical method (PRAM) for measurement of cardiac output during various haemodynamic states. Br J Anaesth 2005; 95: 159-65.
Acknowledgements
We thank Prof. E. Leonard, PhD (Columbia University) for extensive discussions and Prof. G. Heinz, MD (Medical University Vienna) for statistical advice. Jane Neuda provided excellent support in editing the manuscript.
Funding
This work was not supported by any company or third party funding.
Conflicts of interest
None declared.
Author information
Authors and Affiliations
Corresponding author
Additional information
This paper has been presented in part at the Joint Meeting of the German, Austrian, and Swiss Societies for Biomedical Engineering D-A-CH BMT2013 held September 19-21, 2013 in Graz, Austria.
The use of general descriptive names, registered names, or trademarks in this work does not imply, even in the absence of such a statement, that such names are exempt from the relevant protective laws and regulations and therefore free for general use.
Appendices
Appendix 1
FloTrac/Vigileo system
The FloTrac/Vigileo system (Edwards Lifesciences, Irvine, CA, USA) comprises the FloTrac pressure sensor attached to a radial or femoral arterial line using a standard arterial catheter and the Vigileo monitor. After the patient’s age, height, weight, and sex have been entered and the device connected to the artery, SV and arterial CO are continuously estimated. In general, the system is used without the Venous Arterial blood Management Protection (VAMP) blood sampling kit in the operating room. For intensive care application, the FloTrac sensor should be used with a special VAMP system.D
The algorithm is based on the premise that SV is proportional to pulse pressure and is inversely related to aortic compliance.153,154 The algorithm calculates arterial pulsatility (= standard deviation [SD] of the pressure wave).155 According to the patent, the algorithm accounts for vascular resistance and compliance on SV,47 and a variable κ is calculated without any external calibration. These parameters for calculation include 1) the aortic compliance described in the study by Langewouters et al. 156 2) the mean arterial pressure (providing information about resistance changes), 3) the variance of the pressure wave as pulsatility, 4) the skewness, and 5) the kurtosis.A,B The calibration factor κ was recalculated every ten minutes in the first-generation software. The interval of ten minutes was reduced to one minute in the second-generation software (first used in V1.07), and a larger human database was implemented. The newest third-generation software (since V3.0) claims a new dynamic tone technology with automatic factor adaptation to patient vascular tone and also claims to have been validated for hyperdynamic patient conditions, including sepsis59,137 and liver transplantation.62,63 It is also asserted that another key feature of the third-generation software is better performance during arrhythmia.124
The EV1000 Clinical Platform is indicated for use primarily for critical care patients to assess the balance between cardiac function, fluid status, and vascular resistance. Analysis of the intermittent and transpulmonary thermodilution curve provides data on intravascular and extravascular fluid volumes. Whereas the PULSION PiCCO System calculates the volume parameter based on a mean transit time algorithm, the Edwards EV1000 system relies on the decay time of the thermodilution curve. When the EV1000 Clinical Platform is used with the VolumeView System, it measures and/or calculates hemodynamic parameters such as systemic vascular resistance, manually calibrated CO, extravascular lung water, etc. When connected to a FloTrac sensor, the EV1000 Clinical Platform continuously measures/calculates arterial pressure CO.Footnote 6
PiCCO system
The PiCCO technology (PiCCO, PULSION Medical Systems, Munich, Germany) is a hemodynamic monitoring system combining a transpulmonary thermodilution technique for calibration and arterial pulse contour analysis. The PiCCO system consists of a monitor, an inline injectate temperature sensor connected to a central venous catheter, and a 4-French thermistor-tipped catheter for pressure and temperature measurement in a large peripheral artery (femoral, axillary, and brachial). The PiCCO algorithm has been described elsewhere.11 A central venous injection of a cold saline bolus and the time course of the temperature in a peripheral artery are used for the calibration of the system. In older software versions of the PiCCO device, an algorithm was used which was previously described for determination of CO.157,158 With this algorithm, the SV is computed by integrating the systolic area under the arterial pressure waveform. The specific aortic impedance is required for calibration, which is calculated by comparison between the systolic area and the CO measured by transpulmonary thermodilution.Footnote 7 The second-generation software uses an adapted algorithm which analyzes the shape of the pressure waveform, and it also claims to take into account the individual compliance and systemic vascular resistance. However, transpulmonary thermodilution is also needed with the new software version to assess the patient-specific compliance.35,159
LiDCOplus/PulseCO system and LiDCOrapid
The LiDCOplus/PulseCO system (LiDCO Ltd, Cambridge, UK) includes a minimally invasive lithium dilution technique for calibration. A central or peripheral venous access is required for indicator injection. A small dose of lithium chloride (0.002-0.004 mmol·kg−1) is injected. To avoid pharmacological or even toxic effects, the manufacturer recommends an upper limit of 3 mmol·day−1. Cardiac output is calculated from the amount of injected lithium and the arterial concentration time curve which is measured by an ion-selective electrode located in a peripheral artery.160,161 After calibration, the PulseCO performs a beat-to-beat estimate of the cardiac output. The algorithm is assumed to be independent of the arterial measurement site. For the analysis of the pressure trace, a three-step transformation is described.161 Briefly, the first step is the transformation of the arterial pressure signal into a standardized volume-time waveform (done by an algorithm “compliance” with a lookup table).Footnote 8 Second, in order to obtain cardiac output, the duration of the cardiac cycle and the SV are calculated by autocorrelation (the autocorrelation of the standardized volume waveform results in a net effective beat power factor which is proportional to the nominal stroke volume).14 Third, this result is calibrated by comparison with a LiDCO-measured value which the manufacturer recommends to be done every four to six hours.160 This calibration factor corrects for the arterial compliance for a given arterial blood pressure and for variations between individuals.14 Further details for the exact calculation are not provided, not even in the patent description.Footnote 9
The LiDCOrapid can be calibrated by entering a known value for CO (with dilution calibration) or with a nomogram-based estimate of a patient-specific calibration factor. This calibration factor was developed using in vivo calibration data from post-surgical patients providing radial arterial blood pressure waveform data. The nomogram estimate was then validated in an independent cohort of medical ICU patients. A correlation of r = 0.88, no bias, and acceptable limits of agreement (± 26%) were found when compared with indicator dilution-based calibration.C
Modelflow system
The Modelflow system (Finapres Medical Systems, Amsterdam, The Netherlands) computes the beat-to-beat CO from the radial artery pressure after an initial calibration (thermodilution or ultrasound for velocity and aortic diameter determination). The aortic flow pulsations from arterial blood pressure are computed by simulating a nonlinear time-varying three-element model of aortic input impedance (modified Windkessel model).100 The Modelflow system simulates the interaction between the cardiac ejection and the aortic and peripheral systemic input impedance and the resulting reflected pressure.159 The nonlinear characteristics of the model parameters were studied post-mortem in human aortae;162 however, considerable individual variations of the aortic cross-sectional area (up to 30%) were found.159 Therefore, calibration against thermodilution or an aortic diameter calibration101 is required. A more detailed description of the underlying model is to be found in the study by Bogert et al.163
PRAM/Mostcare
With PRAM (Mostcare FIAB SpA, Florence, Italy) beat-to-beat values of CO are calculated. This system is based on the mathematical analysis of changes in the arterial pressure profile.Footnote 10 The PRAM/Mostcare system includes a standard arterial radial or femoral catheter with no need for calibration. Pressure signals and estimated flow values are displayed on the monitor screen in real time. Calibration with other techniques is not required. The algorithm is based on the “principle of perturbations”164 with a beat-to-beat analysis of the whole arterial pressure wave morphology (instead of just the pulsatile systolic area) with a sampling rate of 1 kHz.155 The diastolic minimum, the systolic pressure, the dicrotic notch, and points of perturbance are evaluated. PRAM claims to consider aortic impedance, compliance, and systemic vascular resistance, which affect the pressure signal. For further details, see these references.104,155,165 ,J
Appendix 2
The following explicit search terms in Web of Science yielded 382 hits.
Title=(arterial pressure-based cardiac*) OR Title=(Arterial pressure waveform cardiac*) OR Title=(Vigileo) OR Title=(FloTrac) OR Title=(pulmonary artery thermodilution) OR Title=(thermodilution) NOT Topic=(experimental) NOT Topic=(pediatric) NOT Topic=(pediatric) NOT Topic=(animal) OR Topic=(PICCO) OR Topic=(LiDCO) OR Topic=(PRAM) AND Topic=(cardiac output*gold standard)
Refined by: Research Areas=(CARDIOVASCULAR SYSTEM CARDIOLOGY OR ANESTHESIOLOGY OR SURGERY OR CRITICAL CARE MEDICINE) AND Document Types=(ARTICLE) AND Research Domains=(SCIENCE TECHNOLOGY)
Timespan=1990-2013.
Search language=Auto
Appendix 3
Formulas used for calculating mean cardiac output, bias, standard deviation of the bias, and correlation coefficient
where ni is the number of measurements, xi is the variable for pooled calculation (bias, mean cardiac output, precision), and ri is the correlation coefficient to be pooled in the study i of total n studies for the analysis.
Appendix 4
References# | n | Age (yr) mean (SD) or range | Mean (SD) (L·min−1) | Range (L·min−1) | Bias (SD) (L·min−1) | PE (%) | r** | Software version | Cardiac output | Listed / obvious limitations explanatory notes | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
Population | Access site | Blinded observers | ||||||||||
Auto-calibrated | ||||||||||||
FloTrac/Vigileo | ||||||||||||
Sander et al.39 | 30/108 | 67 (8) | 5.5 (1.1) | x | −0.60 (1.40) | 54 | 0.53 | 1.03 | Cardiac surgery (OP/ICU) | rad | N/A | Range not given |
Button et al.47 | 31/185 | 46-85 | x | 2.4-9.3 | 0.25 (1.13) | x | x | 1.07 | Cardiac surgery (OP/ICU) | rad | N/A | Mean values, PE not given; only gold standard range mentioned |
Manecke and Auger43 | 50/295 | 61 (14) | x | 2.8-9.6 | 0.55 (0.98) | 33 | x | 1.03 | Post cardiac surgery (ICU) | rad/fem | N/A | Mean CO not given; hemodynamic stable patients; different access sites |
Opdam et al. 40 | 6/218 | 56-85 | x | x | 0.41 (1.00) | 40 | 0.35 | 1.03 | Post cardiac surgery (ICU) | rad/fem | N/A | Mean CO and range not given; small number of patients; varying replicates of CO determination |
Prasser et al. 41 | 20/164 | 16-74 | 5.9 (1.2) | 3.4-9.8 | −0.02 (1.48) | 49 | 0.58 | 1.03 | Neurosurgical (ICU) | rad/fem | N/A | Small and varying number of CO estimations performed for each patient; constant vascular tone |
Prasser et al. 49 | 20/158 | 64 (9) | x | x | −0.01 (0.82) | 27 | x | 1.10 | Post cardiac surgery (ICU) | rad | Yes | Mean and range values of CO not given |
Breukers et al. 44 | 20/56 | 72 (9) | 5.5 (0.9) | 3.3-8.8 | 0.14 (1.00) | 36 § | 0.74 | 1.03 | Post cardiac surgery (ICU) | rad | N/A | PE not given; rise in vascular tone over time cannot be excluded because of vasoactive drugs |
Chakravarthy et al. 46 | 15/438 | x | x | 1.0-6.9 | −0.15 (0.33) | x | 0.49 | N/A | Cardiac surgery (OP) | fem | N/A | Mean CO, software version, patient age, and PE not given; small number of patients |
Cannesson et al. 53 | 11/166 | 58-83 | 4.7 (1.0) | 1.9-8.2 | 0.26 (0.87) | 37 § | 0.66 | 1.07 | Cardiac surgery (OP/ICU) | rad | N/A | PE not given; small number of patients; no vasoactive drugs applied |
McGee et al. 37 | 84/561 | 24-84 | 5.9 (?) | 3.1-9.2 | 0.20 (1.28) | 43 | x | 1.01 | After cardiac surgery (ICU) | rad/fem | N/A | SD of mean CO not given; different access sites |
Staier et al. 54 | 30/120 | 45-81 | x | 3.9-4.9 | 0.02 (1.04) | 44 | x | 1.07 | Cardiac surgery (OP) | rad | N/A | Mean and range values of CO not given, therefore estimated from graphs |
Mehta et al. 48 | 12/? | 45-75 | 4.5 (1.3) | 2.8-7.7 | −0.26 (0.66) | 29 | x | 1.07 | Cardiac surgery (OP) | rad | Yes | Number of measurements not given; small sample size; only male patients; exclusion of study: peripheral vascular disease |
Biais et al. 58 | 20/400 | 51 (9) | 5.5 (1.0) | 2.1-9.5 | −0.80 (1.35) | 43 | x | 1.07 | Liver transplant (OP/ICU) | rad | Yes | Reference method: instantaneous TD instead of gold standard |
Zimmermann et al. 38 | 30/174 | 51-80 | x | 2.7-10.7 | −0.13 (1.53) | 46 | 0.56 | 1.01 | Cardiac surgery (OP/ICU) | rad/fem | Yes | Mean CO not given; 3 different monitors used for determination of TD CO |
Della Rocca et al. 50 | 18/126 | 36-67 | x | 3.1-11.5 | −0.95 (1.41) | 26 | 0.68 | 1.10 | Liver transplant (ICU) | rad | N/A | Mean CO not given; hemodynamic stable patients |
Biancofiore et al. 62* | 29/261 | 19-64 | 7.4 (1.7) | 5.8-15.2 | −2.47 (2.66) | 60 | 0.39 | 1.10 | Liver transplant (OP/ICU) | rad | N/A | Observers were not blinded; cardiac index values but BSA not mentioned |
Eleftheriadis et al. 70 | 16/80 | 62 (10) | x | 3.5-7.0 | 0.40 (0.87) | x | 0.51 | 1.14 | Cardiac surgery (OP) | fem | N/A | PE and mean CO not given; only male patients |
Senn et al. 45 | 25/100 | 65 (11) | x | 5.0-6.1 | −0.1 (1.12) | 38 | x | 1.03 | Post cardiac surgery (ICU) | rad | N/A | Low-risk cardiac surgical group; mean CO not given; 1.03 and 1.07 data obtained in different patients (CO differences up to 20%) |
25/100 | 67 (8) | x | 4.3-5.8 | −0.3 (0.71) | 22 | x | 1.07 | Post cardiac surgery (ICU) | rad | N/A | ||
Zimmermann et al. 52 | 24/138 | x | x | x | 0.04 (1.09) | x | x | 1.10 | Cardiac surgery (OP/ICU) | rad | N/A | Reported in a letter, therfore only limited information |
Hofer et al. 55 | 26/? | 67 (10) | x | 2.4-9.1 | 0.20 (1.05) | 40 § | x | 1.07 | Cardiac surgery (OP/ICU) | rad | N/A | Mean CO and PE not given; low risk cardiac surgical group; thermal influences |
Schramm et al. 60 | 20/78 | 64 (14) | x | 3.0-9.0 | −0.35 (1.88) | 76 | x | 1.07 | Cardiac surgery (OP) | rad | N/A | Small sample size (and only 3 female patients); mean and range values of CO not given; range estimated from graphs |
Slagt et al. 59 | 5/86 | 65 (6) | x | 3.6-7.1 | −1.60 (1.60) | 48 | 0.32 | 1.07 | Septic shock (ICU) | rad | N/A | Mean CO not given; small sample size; systemic vascular resistance varied by 30% / 47% during monitoring |
4/73 | 65 (6) | x | 3.3-10.8 | −1.20 (1.10) | 32 | 0.90 | 1.10 | Septic shock (ICU) | rad | N/A | ||
Maxeiner et al. 57 | 19/62 | 52-86 | 5.0 (1.0) | x | 0.87 (1.02) | 45 | 0.46 | 1.07 | Cardiac surgery (OP) | rad | N/A | No cardiac output range mentioned; left or right radial artery access |
15/60 | 52-86 | 4.7 (1.0) | x | 0.51 (0.82) | 36 | 0.72 | 1.10 | Cardiac surgery (OP) | rad | N/A | ||
Hadian et al. 71 | 17/? | 54-82 | 6.1 (1.9) | x | 0.43 (1.69) | 59 | 0.28 | 1.07 | Post cardiac surgery (ICU) | rad/fem | Yes | Number of measurement and CO range not given; calibration with PAC-TD; different access sites; reference method: CCO and TD-CO |
Cecconi et al. 42 | 29/203 | 24-83 | x | 3.7-10.8 | −1.10 (2.85) | 55 | x | 1.03 | Patients on ICU | rad | N/A | Mixed medical surgical population in which many were septic; no mean CO |
Krejci et al. 63 | 19/97 | 56 (9) | 7.2 (1.8) | x | −3.54 (?) | 69 | x | 1.10 | Liver transplant (OP) | rad | N/A | Range and SD of bias not given; study was limited to the dissection phase |
Saraceni et al. 61 | 15/96 | 31-80 | 6.56 (?) | 3.5-11.8 | 0.19 (2.50) | 76 § | 0.63 | 1.07 | Patients on ICU | rad | N/A | SD of mean CO and PE not given; heterogeneous patient group: trauma, septic, cardiac |
6/45 | 44-67 | 7.48 (?) | 5.4-10.4 | −0.97 (1.83) | 49 § | 0.72 | 1.10 | Patients on ICU | rad | N/A | SD of mean CO and PE not given; heterogeneous patient group: trauma, septic, cardiac | |
Vetrugno et al. 56 | 20/360 | 70 (9) | x | 2.4-7.7 | 0.50 (0.86) | 37 | x | 1.10 | Cardiac surgery (OP/ICU) | rad | Yes | Mean CO not given; left or right radial artery access |
Junttila et al. 64 | 16/407 | 54 (13) | 6.0 (1.7) | x | −1.50 (2.00) | 58 | x | 1.14 | Intracranial hemorrhage (ICU) | rad | N/A | Range not given; bolus TD performed by different persons |
Biancofiore et al. 66* | 21/210 | 32-60 | 8.2 (1.9) | 3.8-14.8 | −0.74 (1.60) | 52 | 0.67 | 3.02 | Liver transplant (OP/ICU) | rad | N/A | Single bolus TD measurement taken as CO reference |
De Backer et al. 51 | 58/401 | 62 (14) | 6.5 (1.5) | 2.5-14.4 | 0.2% (1.05) | 30 | x | 1.14 | Septic patients (ICU) | rad/fem | Yes | Bias stated in %; different access sites |
58/401 | 62 (14) | 7.3 (2.1) | 2.5-17.0 | −10.3% (1.10) | 29 | x | 3.02 | Septic patients (ICU) | rad/fem | Yes | Bias stated in %; different access sites | |
Akiyoshi et al. 69 | 20/138 | 55 (9) | 6.3 (?) | x | −0.89 (1.35) | 38 | x | 3.00 | Liver transplant (OP/ICU) | rad | N/A | SD of mean CO and range not given; single bolus TD taken as CO reference |
Tsai et al. 65 | 20/200 | x | 5.9 (1.8) | 2.8-10.9 | −0.22 (1.67) | 55 | x | 3.02 | Liver transplant (OP) | rad | Yes | Age not given; Asian study population, but Vigileo patient demographics have been derived mostly from western countries |
Vasdev et al. 68 | 38/342 | 58 (9) | 4.8 (?) | 2.0-8.5 | −0.14 (0.55) | 22 | x | 3.02 | Cardiac surgery (OP) | rad | No | Only 4 female patients; low-risk cardiac surgical group |
Slagt et al. 67 | 19/314 | 62 (15) | 6.8 (2.0) | 4.0-13.7 | −1.70 (2.40) | 53 | x | 3.02 | Septic shock (ICU) | rad/fem | N/A | Different access sites |
References # | n | Age (yr) Mean (SD) or Range | Mean (SD) (L·min−1) | Range (L·min−1) | Bias (SD) (L·min−1) | PE (%) | r** | Software version | Condition of the participants | Access site | Blinded observers | Listed /obvious limitations explanatory notes |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
Calibrated | ||||||||||||
PiCCO/PiCCOplus | ||||||||||||
Irlbeck et al.87 | 20/165 | x | x | x | −0.09 (0.85) | x | 0.93 | 1.x | Patients on ICU | rad/fem | N/A | Age, mean CO, range, and PE not given; different access sites |
Buhre et al.72 | 12/36 | 46-66 | 4.4 (?) | 1.6-9.2 | 0.003 (0.63) | 29 § | 0.88 | 1.x | Cardiac surgery (OP) | fem | N/A | SD of mean CO and PE not given; small number of patients and measurements |
Rödig et al.34 | 26/308 | 44-82 | x | 2.3-12.6 | 0.18 (1.24) | x | x | 1.x | Cardiac surgery (OP/ICU) | fem | N/A | Bias (SD) obtained from another study; mean CO and PE not given |
Gödje et al. 35 | 24/204 | 41-81 | x | 3.0-11.8 | 0.07 (0.70) | x | 0.92 | x | Post cardiac surgery (ICU) | fem | N/A | Mean CO, PE, and software version not given; no recalibration for 24hr |
Zöllner et al.73 | 19/228 | 34-76 | x | 3.0-15.7 | 0.31 (1.25) | x | 0.88 | x | Post cardiac surgery (ICU) | fem | N/A | Mean CO, PE, and software version not given; hemodynamically stable patients |
Rauch et al. 79 | 25/380 | 42-77 | x | 1.9-11.6 | −0.14 (1.16) | x | x | 1.x | Cardiac surgery (OP/ICU) | fem | N/A | Mean CO and PE not given; initial calibration with PAC TD, only one recalibration in 12 hours |
Mielck et al.80 | 22/96 | 49-74 | 6.6 (1.7) | 2.6-11.4 | −0.40 (1.30) | 39 | x | x | Post cardiac surgery (ICU) | fem | N/A | Software version not given; hemodynamically stable patients |
Gödje et al. 35 | 24/517 | 46-88 | x | 2.7-14.1 | −0.20 (1.15) | x | 0.88 | 4.1 | Post cardiac surgery (ICU) | fem | N/A | Mean CO and PE not given; influences of arrhythmias on the accuracy of PiCCO |
Della Rocca et al. 86 | 62/186 | 24-66 | 7.8 (?) | 3.0-13.0 | 0.04 (0.84) | 22 § | 0.94 | 4.1 | Liver transplant (OP) | fem | N/A | SD of mean CO and PE not given, stable hemodynamic conditions |
Felbinger et al. 88* | 20/360 | x | x | x | 0.27 (0.63) | x | 0.93 | x | Post cardiac surgery (ICU) | fem | No | Age, mean CO, range, PE, and software version not given |
Tzenkov et al.77 | 35/314 | x | x | 1.3-19.0 | 0.18 (2.41) | x | x | 4.1 | Liver transplant (OP) | fem | N/A | Age, mean CO and PE not given; no recalibration |
Della Rocca et al.84 | 58/318 | x | 6.1 (?) | 2.7-12.0 | 0.08 (0.72) | 24 § | x | 4.1 | Lung transplant (OP) | fem | N/A | SD of mean CO and age not given |
Sander et al. 82 | 45/? | 62 (1) | 6.5 (0.3) | 2.5-12.5 | −1.40 (1.70) | 52 § | 0.63 | 5.2.2 | Cardiac surgery (OP) | fem | N/A | PE, number of measurements and values of the total study period not given, therefore 15 min after aorta decannulation |
Wouters et al. 78 | 23/224 | 65 (?) | x | x | 1.08 (0.75) | x | 0.80 | x | Cardiac surgery (OP) | bra | N/A | SD of mean age, mean CO, range, PE, and software version not given; single bolus TD CO as reference method |
Sujatha et al.36 | 60/480 | 40-75 | 4.4 (?) | x | 0.42 (0.86) | 36 | x | x | Cardiac surgery (OP) | fem | N/A | Mean bias not given; stated bias was recalculated over total study period; range and software version not given |
Ostergaard et al. 83 | 25/? | 42-79 | 4.8 (?) | 3.8-6.1 | −0.07 (1.10) | 50 | x | x | Cardiac surgery (OP/ICU) | fem | N/A | Number of measurements, SD of mean CO, and software version not given; hemodynamically stable patients |
Halvorsen et al. 81 | 30/252 | 39-86 | 6.0 (?) | 5.0-7.1 | −0.76 (1.17) | 43 | x | 5.1 | Cardiac surgery (OP) | fem | N/A | SD of mean CO not given; stated values during period 1, as no values of total study period were given |
Chakravarthy et al. 46 | 15/438 | x | x | 1.0-6.9 | −0.13 (1.12) | x | 0.40 | x | Cardiac surgery (OP) | fem | N/A | Age, mean CO, PE, and software version not given; small number of patients; initial calibration with PAC TD |
de Wilde et al.21 | 24/199 | x | 4.7 (?) | 2.1-9.7 | −0.14 (0.87) | 37 § | x | x | Cardiac surgery (OP) | rad | N/A | Initial calibration with PAC TD; no age, SD of mean CO, PE, or software version mentioned |
Button et al. 47 | 31/185 | 46-85 | x | 2.4-9.3 | 0.28 (1.30) | x | x | 6.0 | Cardiac surgery (OP/ICU) | fem | N/A | Mean CO and PE not given |
Yamashita et al.85 | 20/? | 68 (7) | 3.0 (0.8) | x | −0.14 (0.34) | 23 § | 0.98 | x | Prior cardiac surgery (OP) | fem | N/A | Number of measurements, range, PE, and software version not given; stated values after prostaglandin administration |
Senn et al. 45 | 25/100 | 65 (11) | x | 4.9-5.8 | −0.20 (0.82) | 25.5 | x | 6.0 | Post cardiac surgery (ICU) | fem | N/A | Mean CO not given; low-risk cardiac surgical group |
Hofer et al. 55 | 26/? | 67 (10) | x | 2.4-9.1 | 0.20 (1.10) | 34 § | x | 5.2.2 | Cardiac surgery (OP/ICU) | fem | N/A | Number of measurements, mean CO, and PE not given; low-risk cardiac surgical group; thermal influences |
Hadian et al. 71 | 17/? | 54-82 | 5.4 (1.5) | x | −0.24 (1.10) | 41 | 0.33 | x | Post cardiac surgery (ICU) | rad/fem | N/A | Measurements, range and software version not given; calibration with PAC-TD; different access sites; reference method: CCO and TD-CO |
Staier et al.76 | 30/30 | 59 (11) | 4.1 (0.9) | x | 0.12 (?) | 28 | x | x | Cardiac surgery (OP) | fem | N/A | Range, bias SD, and software version not given; small sample size |
LiDCO/PulseCO | ||||||||||||
Linton et al. 90 | 40/160 | x | x | x | −0.25 (0.5) | x | 0.97 | x | Post cardiac surgery (ICU) | N/A | N/A | Age, range, mean CO, and PE not given; results from LiDCO but not PulseCO |
Garcia-Rodriguez et al.91 | 31/93 | 42-80 | 5.55 (?) | 2.4-11.5 | −0.5 (0.7) | 24 § | x | x | Post major surgery (ICU) | rad | N/A | SD of mean CO and PE not given; hemodynamically stable patients; results from LiDCO but not PulseCO |
Hamilton et al. 92 | 20/100 | 64 (2) | x | 3.4-8.5 | 0.05 (0.6) | x | 0.86 | x | Post cardiac surgery (ICU) | rad | N/A | Mean CO, and PE not given; low-risk cardiac surgical group |
Yamashita et al. 97 | 23/? | 68 (9) | x | 1.5-4.5 | 0.76 (1.93) | x | 0.74 | x | Cardiac surgery (OP) | rad | N/A | Mean CO not given; PAC TD used for initial calibration of PulseCO; no PE, no recalibration |
Costa et al. 94 | 23/151 | 37-68 | 7.7 (?) | 3.4-13.2 | −0.29 (1.09) | 17 | 0.85 | x | Liver transplant (ICU) | rad | N/A | SD of mean CO not given |
Missant et al.96 | 20/149 | 68 (12) | 4.9 (?) | x | −0.03 (0.65) | 29 | 0.84 | x | Cardiac surgery (OP) | rad | N/A | SD of mean CO and range not given; PAC TD (instead of LiDCO) used for initial calibration of PulseCO |
de Wilde et al.21 | 24/199 | x | 5.0 (?) | 2.5-8.9 | 0.17 (0.69) | 28 § | x | x | Cardiac surgery (OP) | rad | N/A | Age, SD of mean CO, and PE not given; PAC TD (instead of LiDCO) used for initial calibration of PulseCO |
Krejci et al. 63 | 19/107 | 56 (9) | 8.2 (?) | x | −1.97 (?) | 76 | x | x | Liver transplant (OP) | rad | N/A | SD of mean CO, SD of bias, and range not given; only one recalibration every 24 hours; calibration before induction of anesthesia |
Hadian et al. 71 | 17/? | 54-82 | 5.4 (1.6) | x | 0.18 (0.78) | 29 | 0.60 | x | Post cardiac surgery (ICU) | rad/fem | N/A | Measurements and range not given; calibration with PAC-TD; different access sites; reference method: CCO and TD-CO |
Cecconi et al. 42 | 29/203 | 24-83 | x | 3.5-13.6 | 0.50 (2.00) | 40 | x | x | Patients on ICU | rad | N/A | Mean CO not given; mixed medical surgical population including septic patients |
Dyer et al. 95 | 16/? | x | 5.0 (?) | 3.6-9.4 | −0.58 (0.77) | 22 § | x | x | Severe pre-eclampsia | rad | N/A | Measurements, SD of mean CO, age, and PE not given; central venous calibration; stable monitoring conditions |
Mora et al. 93 | 30/220 | 68 (13) | 6.2 (1.9) | 2.6-10.8 | −0.28 (0.84) | 27 | 0.86 | x | Post cardiac surgery (ICU) | rad | Yes | PAC TD and PulseCO values assessed with a small time delay |
Modelflow | ||||||||||||
Wesseling et al. 100 | 8/76 | x | 4.7 (0.4) | 3.1-6.9 | 0.09 (0.36) | 15 § | x | x | Cardiac surgery (OP) | N/A | N/A | Age and PE not given; small number of patients; TD calibration |
Jellema et al.101 | 15/137 | 19-74 | 8.9 (3.0) | x | −0.10 (0.80) | 18 § | x | x | Septic shock (ICU) | rad/fem | N/A | Range not given; no PE; PAC TD calibration |
Hirschl et al.103* | 29/175 | 61 (16) | 6.3 (?) | 2.5-13.9 | −0.65 (1.25) | 19 § | x | x | Critical ill patients (ICU) | ni | N/A | SD of mean CO and PE not given; PAC TD calibration |
Jansen et al. 99 | 54/436 | 43-78 | 4.9 (0.9) | 3.0-7.7 | −0.13 (0.47) | 19 § | x | x | Cardiac surgery (OP) | N/A | N/A | No PE; anesthesia regimen differed slightly; PAC TD calibration |
de Vaal et al. 102 | 24/24 | 35-79 | 5.4 (?) | 3.1-8.8 | −0.08 (0.70) | 12 | 0.83 | x | Post cardiac surgery (ICU) | ni | N/A | SD of mean CO not given; aortic diameter calibration with ultrasound echo system |
de Wilde et al. 21 | 24/199 | x | 4.8 (?) | 2.5-7.1 | 0.00 (0.37) | 15 § | x | x | Cardiac surgery (OP) | rad | N/A | Age, SD of mean CO and PE not given |
Nissen et al. 98 | 39/1309 | 23-66 | 7.8 (2.6) | 2.1-16.4 | 0.10 (1.50) | 39 § | 0.81 | x | Liver transplant (OP) | fem | N/A | No PE mentioned; PAC TD calibration |
References # | n | Age (yr) Mean (SD) or range | Mean (SD) (L·min−1) | Range (L·min−1) | Bias (SD) (L·min−1) | PE (%) | r** | Software version | Condition of the participants | Access site | Blinded observers | Listed / obvious limitations explanatory notes |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
Non-calibrated | ||||||||||||
PRAM | ||||||||||||
Romano and Pistolesi104* | 18 / ? | 32-48 | 4.9 (1.1) | 3.2-7.6 | −0.29 (0.67) | 27 § | 0.88 | x | Heart catheterization (ICU) | A | N/A | Number of measurements and PE not given; pressure signal recorded in the aorta not in the peripheral artery |
Giomarelli et al.106 | 28 / 112 | 66 (3) | x | 2.3-7.4 | 0.03 (0.89) | x | 0.88 | x | Cardiac surgery (OP) | rad | N/A | Mean (SD) CO and PE not given; low-risk patients during stable hemodynamic situations; hypothermia during ECC |
Romano et al.105* | 50 / ? | 62 (14) | 5.1 (1.1) | 3.0-8.0 | −0.06 (0.80) | 31 § | 0.85 | x | Heart catheterization (ICU) | A | N/A | Number of measurements and PE not given |
Romano et al.107 | 32 / 128 | 44-81 | 4.0 (0.7) | x | 0.07 (0.40) | 20 § | 0.87 | x | Cardiac surgery (OP) | rad | Yes | Range and PE not given; low-risk patients; hypothermia during extracorporeal circulation |
Zangrillo et al.108* | 28 / 28 | 63 (10) | 5.1 (1.1) | 3.0-8.3 | −0.13 (0.78) | 30 | 0.72 | x | Post cardiac surgery (ICU) | rad | N/A | Measurement with artefacts were excluded without definition of criteria on the signal quality |
Paarmann et al. 111 | 23 / 46 | 51-82 | x | 2.6-9.2 | 0.00 (2.26) | 87 | 0.31 | x | Post cardiac surgery (ICU) | rad | N/A | Mean (SD) CO not given; stable hemodynamic conditions |
Scolletta et al. 109 | 15 / 106 | x | x | x | 0.2 (0.98) | 24 | 0.90 | x | Post cardiac surgery (ICU) | N/A | N/A | Age, mean (SD) CO, and range not given; patients with intra-aortic balloon pump |
Franchi et al. 110 | 30 / 90 | 21-81 | 7.7 (?) | 4.5-13.5 | 0.26 (0.98) | 25 | 0.93 | x | Septic shock (ICU) | rad | N/A | SD of mean CO not given: stable hemodynamic conditions |
Maj et al. 112 | 41/123 | 66 (12) | 4.6 (?) | x | 0.25 (1.66) | 73 | 0.08 | x | Post cardiac surgery (ICU) | rad/fem | N/A | Different access sites; median instead of mean CO; range not given |
Rights and permissions
About this article
Cite this article
Schlöglhofer, T., Gilly, H. & Schima, H. Semi-invasive measurement of cardiac output based on pulse contour: a review and analysis. Can J Anesth/J Can Anesth 61, 452–479 (2014). https://doi.org/10.1007/s12630-014-0135-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12630-014-0135-8