Abstract
Purpose
The saphenous nerve block using a landmark-based approach has shown promise in reducing postoperative pain in patients undergoing arthroscopic medial meniscectomy. We hypothesized that performing an ultrasound-guided adductor canal saphenous block as part of a multimodal analgesic regimen would result in improved analgesia after arthroscopic medial meniscectomy.
Methods
Fifty patients presenting for ambulatory arthroscopic medial meniscectomy under general anesthesia were prospectively randomized to receive an ultrasound-guided adductor canal block with 0.5% ropivacaine or a sham subcutaneous injection of sterile saline. Our primary outcome was resting pain scores (numerical rating scale; NRS) upon arrival to the postanesthesia care unit (PACU). Secondary outcomes included NRS at six hours, 12 hr, 18 hr, and 24 hr; postoperative nausea; and postoperative opioid consumption.
Results
There was a statistically significant difference in mean NRS pain scores upon arrival to the PACU (P = 0.03): block group NRS = 1.71 (95% confidence interval [CI] 0.73 to 2.68) vs sham group NRS = 3.25 (95% CI 2.27 to 4.23). Cumulative opioid consumption (represented in oral morphine equivalents) over 24 hr was 71.8 mg (95% CI 56.5 to 87.2) in the sham group vs 44.9 mg (95% CI 29.5 to 60.2) in the block group (P = 0.016).
Conclusions
An ultrasound-guided block at the adductor canal as part of a combined multimodal analgesic regimen significantly reduces resting pain scores in the PACU following arthroscopic medial meniscectomy. Furthermore, 24-hr postoperative opioid consumption and pain scores were also reduced.
Résumé
Objectif
Le bloc du nerf saphène à l’aide d’une approche par repères anatomiques s’est avéré prometteur pour réduire la douleur postopératoire chez les patients subissant une méniscectomie médiale par arthroscopie. Nous avons émis l’hypothèse qu’en réalisant un bloc échoguidé du canal adducteur du nerf saphène dans le cadre d’un régime analgésique multimodal, l’analgésie serait plus efficace après une méniscectomie médiale par arthroscopie.
Méthode
Cinquante patients devant subir une méniscectomie médiale par arthroscopie en ambulatoire sous anesthésie générale ont été randomisés de façon prospective à recevoir un bloc échoguidé du canal adducteur avec de la ropivacaïne 0,5 % ou une injection sous-cutanée fictive de solution saline stérile. Notre critère d’évaluation principal était les scores de douleur au repos (échelle d’évaluation numérique; ÉÉN) à l’arrivée en salle de réveil. Les critères d’évaluation secondaires comprenaient l’ÉÉN à six heures, 12 h, 18 h et 24 h; les nausées postopératoires; et la consommation postopératoire d’opioïdes.
Résultats
Une différence statistiquement significative a été observée dans les scores de douleur moyens à l’arrivée en salle de réveil (P = 0,03): ÉÉN du groupe bloc = 1,71 (intervalle de confiance [IC] 95 % 0,73 à 2,68) vs. ÉÉN du groupe témoin = 3,25 (IC 95 % 2,27 à 4,23). La consommation cumulée d’opioïdes (représentée en équivalents morphine orale) sur 24 h était de 71,8 mg (IC 95 % 56,5 à 87,2) dans le groupe témoin vs. 44,9 mg (IC 95 % 29,5 à 60,2) dans le groupe bloc (P = 0,016).
Conclusion
Un bloc échoguidé au niveau du canal adducteur, dans le cadre d’un régime d’analgésie multimodale combiné, réduit significativement les scores de douleur au repos en salle de réveil après une méniscectomie médiale par arthroscopie. En outre, la consommation postopératoire d’opioïdes à 24 h et les scores de douleur sont également réduits.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Arthroscopic knee surgery can cause sufficient postoperative pain to potentially delay timely discharge from the ambulatory surgical setting. Analgesia after knee surgery can be provided by multiple non-systemic non-opioid-based methods, including local anesthetic infiltration, peripheral nerve blockade, neuraxial procedures, and intra-articular injections. The femoral nerve block has been shown to be superior to traditional intra-articular injection of local anesthetics in some knee surgeries,1 but motor blockade of the quadriceps with the potential risk for falls limits the value of femoral blocks for less invasive ambulatory surgery.2,3 Orthopedic surgery is increasingly being performed on an ambulatory basis where perioperative analgesia can improve timely discharge in the outpatient setting.4
A transsartorial landmark-based distal approach to the saphenous nerve block has been shown to reduce pain significantly by providing sensory block to the tissues around the medial meniscus.5 The saphenous nerve, a terminal branch of the femoral nerve, provides cutaneous sensation to the peripatellar region and the medial aspect of the lower extremity below the knee as well as to the articular branches to the medial aspect of the knee joint. The saphenous nerve separates from the femoral nerve in the proximal third of the thigh, courses through the adductor canal with the nerve to the vastus medialis, and emerges from the adductor hiatus to divide into the infrapatellar branch and the sartorial branch.6,7 Traditionally, saphenous nerve blocks have been performed as an anatomical landmark-based technique with marginal rates of success, as low as 33%.8 With ultrasound guidance, the feasibility of effective saphenous nerve block at the adductor canal has been shown.9 The adductor canal block may provide superior analgesia over traditional distal saphenous nerve blocks for surgical procedures of the knee because this block includes the saphenous nerve, the nerve to the vastus medialis, and potentially the articular contribution of the obturator nerve to the knee joint.10–13 Our primary hypothesis was that performing an adductor canal block as part of a multimodal analgesic regimen would result in improved analgesia immediately following arthroscopic medial meniscectomy.
Methods
The Institutional Review Board of the Benaroya Research Institute at Virginia Mason Medical Center approved the protocol on May 26, 2011. The study was conducted from June 2011 to June 2012. Written informed consent was obtained from 50 subjects (American Society of Anesthesiologists’ physical status I-III) scheduled for knee arthroscopy and primary unilateral medial meniscectomy. Exclusion criteria included age < 18 or > 70 yr, contraindications to peripheral nerve blockade (localized infection, sepsis, lower extremity neuromuscular disorder), allergy to opioids or local anesthetics, allergy to sulfa or nonsteroidal anti-inflammatory medications, chronic opioid use (more than one month of morphine 60 mg oral equivalents qd), and patient refusal. All participants were recruited at the Lindeman Surgery Center of Virginia Mason Medical Center in Seattle, WA, USA. Data were collected on the day of surgery and via telephone conversation by a blinded investigator 24 hr after the surgical procedure.
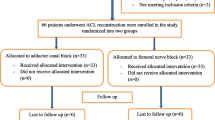
Patients were assigned by pre-randomized sealed envelopes to receive an ultrasound-guided saphenous nerve block at the adductor canal (n = 25) or a sham block (n = 25). All blocks were performed in the preoperative holding area < 30 min prior to surgery. All patients received celecoxib 400 mg orally 20 min prior to the surgical procedure.
A high-frequency linear array ultrasound transducer (SonoSite M-Turbo, Bothell, WA, USA or Philips HD11-XE, Andover, MA, USA) was used to identify the adductor canal.9 Exact block location was performed by first placing the transducer mid-thigh, half the distance between the inguinal crease and the patella. The superficial femoral artery was identified dorsal to the sartorius muscle in short-axis. At this level, the hyperechoic structure located lateral/anterior to the artery was identified containing the saphenous nerve and branches to the vastus medialis (Fig. 1). An injection of 1% lidocaine 1-3 mL was used for skin infiltration. Block sedation with propofol was provided in 10 mg doses, maximum 50 mg, if requested by the study subject.
In patients randomized to the nerve block group, a 21G 100-mm Stimuplex® needle (B Braun, Melsungen, Germany) was placed in proximity to the saphenous nerve under ultrasound guidance alone using an in-plane technique. An injection of 0.5% ropivacaine 15 mL with 1:400,000 epinephrine was then introduced within the adductor canal (Fig. 2). Patients randomized to the sham block group received an ultrasound-guided subcutaneous injection of normal saline solution 2 mL through a similar 21G 100-mm Stimuplex needle.14 All injections were performed either by one of the senior investigators or by a regional anesthesia fellow under the direct supervision of one of the senior investigators.
Sensory blockade was tested before and after completion of the procedure on a dichotomous scale: presence or absence of pinprick sensation along the distribution of the saphenous nerve. Two areas of saphenous nerve distribution were tested for sensory changes: the medial infrapatellar region and the medial malleolus. The lateral thigh and lateral malleolus were also assessed for sensation in the same fashion in an attempt to reduce the opportunity of subject bias or unblinding. Blocks were considered successful if either the infrapatellar region or the medial malleolus was insensitive to pinprick. A blinded investigator obtained these sensory assessments every five minutes after injection for a maximum of 20 min.
After placement and assessment of the block, general anesthesia was induced with propofol 1.5-2 mg·kg−1 to facilitate placement of a laryngeal mask airway device. Maintenance of anesthesia was accomplished with sevoflurane (2-4%). Fentanyl 1-2 μg·kg−1 was administered intraoperatively at the discretion of the blinded anesthesiologist. All anesthesia, surgical, and nursing personnel caring for the patient intraoperatively were blinded to the randomization of the subjects. Droperidol 0.625 mg iv was administered as a prophylactic antiemetic following induction. Subjects reporting a history of postoperative nausea and vomiting were also treated with dexamethasone 4 mg iv. At the completion of the procedure, the surgeon infiltrated each of the port sites with subcutaneous 0.25% bupivacaine 5 mL with epinephrine 1:200,000 prior to placement of the surgical dressing. At the conclusion of the surgery, all subjects were transferred to the postanesthesia care unit (PACU).
In the PACU, nurses blinded to the randomization of the study patients recorded the patients’ pain scores on an 11-point numerical rating scale (NRS), with 0 representing no pain at all and 10 representing the worst pain imaginable, and administered increments of fentanyl 25 μg every five minutes intravenously and/or oxycodone 5-10 mg orally as needed to reduce NRS to < 4. All results were converted to oral morphine equivalents (intravenous fentanyl 10 μg = oral morphine 3 mg = oral oxycodone 2 mg).15 For nausea or vomiting, subjects received ondansetron 4 mg intravenously. All subjects were asked to stand and bear weight prior to discharge. If necessary, patients were given crutches to assist with mobilization at home. For discharge, standard instructions of “activity as tolerated” and home use of multimodal analgesics (ibuprofen and acetaminophen) were given to each subject. No goals or limitations for physical activity were given in the discharge instructions specific to this study.
Intraoperative and postoperative administration of opioids was recorded. Any patient requesting or receiving additional antiemetics in the PACU was deemed to have postoperative nausea; however, no further inquiry was made on the issue of nausea once the patient was discharged. Subjects used the 11-point NRS to record their own pain scores upon discharge and after six, 12, 18, and 24 hr post-procedure. Additionally, subjects recorded their own postoperative 24-hr opioid consumption. After more than 24 hr post-procedure, an investigator collected the pre-recorded postoperative data from the subjects’ home study form and the PACU electronic medical record.
The study was designed to detect a clinically meaningful difference of 2 on the NRS from an expected 5 in the sham group to 3 in the block group.16 Using several prior studies on similar surgical procedures, our power analysis assumed a baseline NRS score of 5 without a peripheral nerve block.5,17,18 Therefore, in order for our study to detect a 40% reduction in NRS pain scores between groups immediately postoperatively, 24 subjects per group were required to provide the necessary power (90%) for this study. One additional patient per group was enrolled to account for patient drop-out or loss to follow-up. The primary outcome was mean resting NRS pain scores upon arrival to the PACU. Secondary endpoints included NRS scores at six hours, 12 hr, 18 hr, and 24 hr; opioid consumption, and postoperative nausea. This study was not powered to detect differences in secondary endpoints.
A random number generator determined the allocation sequence where odd numbers were placed into the block group and even numbers were placed into the sham group. The randomization assignment was concealed with individual envelopes and revealed only to the researcher performing the block just prior to the procedure. The principal investigator generated the randomized allocation sequence, but subjects were recruited and enrolled by the other authors. Aside from the study investigators performing the blocks, all other researchers, anesthesia personnel, surgeons, physician assistants, nurses, and the study participants were blinded to the randomization of each subject.
Statistical methodology
Baseline variables are summarized with the mean (SD) or the frequency and percent of the treatment group. The NRS scores and 24-hr opioid consumption were compared using analysis of variance, and these results are reported as least-square means and 95% confidence intervals. Prior to unblinding, the decision was made to exclude protocol violations that might affect pain or the evaluation of pain from the primary analysis. The primary analysis was repeated including these patients for comparison. As sensitivity analyses for the NRS findings, these models were repeated using log-transformed pain scores and with baseline pain scores included as a covariate. For 24-hr opioid consumption, which has a more pronounced skew, the least-square geometric mean (based on log-transformed morphine equivalents [MEQ] to reduce skew) was calculated for comparison.
No adjustments were made for multiple comparisons because these results are meant to describe the study results and are not intended for inference to other populations. All tests and confidence intervals are two-sided, and P values < 0.05 were considered to be statistically significant.
Results
Forty-eight subjects, 24 in each arm, completed the study protocol and were analyzed for the primary outcome. One subject from each arm had to be excluded for protocol violations (Fig. 3). One of the two excluded subjects inadvertently received ondansetron and one unintentionally became unblinded to the intraoperative anesthetic team. There were no significant differences between groups in terms of age, sex, body mass index, duration of surgery, or baseline NRS scores (Table). Onset of sensory blockade in the adductor-canal block group occurred in 83% of patients by 20 min. A single subject in the sham group reported sensory loss along the distribution of the saphenous nerve five minutes after injection. All subjects recruited for this study were contacted postoperatively and able to give a complete data set of pain scores and opioid consumption.
As regards primary outcome, resting NRS pain scores were lower in the block group (mean NRS = 1.71; 95% confidence interval [CI] 0.73 to 2.68) than in the sham group (mean NRS = 3.25; 95% CI 2.27 to 4.23) upon arrival to the PACU (P = 0.03). When the two patients with protocol violations were included in this analysis, the results were similar (mean NRS = 1.92; 95% CI 0.91 to 2.93 in the block group vs mean NRS = 3.40; 95% CI 2.39 to 4.41 in the sham group; P = 0.04). Inclusion of baseline pain scores as a covariate did not change these results appreciably. Our secondary outcomes of NRS pain scores at PACU discharge, 12, 18, and 24 hr after surgery completion also differed significantly between the block and sham groups (Fig. 4).
The sham group received more fentanyl [mean (SD)] than the block group [62 (35) μg vs 40 (47) μg, respectively; P = 0.011]. Total opioid consumption over 24 hr (reported in oral MEQs) was 72 mg (95% CI 56.5 to 87.2) in the sham group and 45 mg (95% CI 29.5 to 60.2) in the block group (P = 0.016). The only two instances of postoperative nausea occurred in the block group; none occurred in the sham group. One patient in each group received dexamethasone 4 mg iv for a history of postoperative nausea and vomiting. No other complications or unintended effects, including difficulty with weight bearing in the PACU or postoperative falls, were reported in either group at follow-up.
Discussion
This study shows that single injection ultrasound-guided block of the adductor canal for arthroscopic medial meniscectomy provides a significant reduction in resting NRS pain scores immediately following surgery when compared with general anesthesia alone. Additionally, pain scores in the block group were lower at most time points in the first 24 hr after the procedure. In conjunction with lower pain scores, the adductor canal nerve block resulted in a 38% reduction in cumulative intraoperative and postoperative opioid consumption.
All subjects in this study received preoperative oral celecoxib, a nonsteroidal anti-inflammatory drug that is effective in reducing pain after arthroscopic knee surgery.18 Despite the reduction in pain scores from the use of a nonsteroidal anti-inflammatory drug, this study shows that the addition of an adductor canal block further decreases postoperative pain while reducing opioid consumption. Multimodal analgesia with a nonsteroidal anti-inflammatory drug is becoming common practice; therefore, it is clinically relevant to include it in both arms of our study, even if the addition of this oral analgesic alone reduces baseline PACU pain scores.18
Arthroscopic knee surgery is a very common procedure in the United States with over 900,000 cases performed in 2006 alone.19 In Ontario, the rate of knee arthroscopies was almost 200 cases / 100,000 population in 2004, a rate almost 35% higher than in England in the same year.20 With this large number of arthroscopic knee surgeries being performed annually, even small improvements in these clinical metrics have the potential to result in major improvements in efficiency of resource utilization. Our results show that the sham group had higher PACU pain scores despite receiving over 50% more intraoperative fentanyl, which highlights the analgesic efficacy of this nerve block. Therefore, we find our reduction in mean PACU NRS pain scores from 3.25 to 1.71 potentially clinically relevant as the adductor canal block can be used as part of a multimodal analgesic clinical pathway to improve recovery after arthroscopic knee surgery. Several studies have validated improvements > 0.9 mm on a 100-mm scale as clinically significant, and our mean improvement in NRS scores exceeds these benchmarks for clinical relevance.21,22
A previous study on arthroscopic medial meniscectomy using landmark techniques for a more distal approach to the saphenous nerve block showed a greater clinical effect in the reduction of NRS scores when compared with our study.5 Nevertheless, we hypothesize that this larger clinical difference in pain score reduction was due to three important methodological differences: 1) subjects were not given intraoperative opioids; 2) subjects were not given preemptive multimodal analgesia; and 3) surgeons did not inject the arthroscopic port sites with local anesthetic. In our view, some, if not all, of these methods are becoming common practice and should be incorporated into any investigation that looks at differences in clinical outcomes for this surgery. The use of these interventions in concert may offer another explanation as to why there was not an even greater clinical difference in our NRS pain scores. Based on previous studies, we assumed the non-intervention group would have PACU NRS scores of approximately 5; however, our sham group showed a mean NRS pain score of 3.25 upon arrival to the PACU. Nevertheless, we still saw a significant reduction (47%) in the primary outcome, mean resting NRS pain scores in the PACU. Multimodal analgesic interventions, which include an adductor canal block for arthroscopic medial meniscectomy, may potentially improve other clinical outcomes, such as PACU length of stay. This, however, will require further investigation.
The placement of ultrasound-guided adductor canal blocks in our study population was at least 83% successful at 20 min. This is similar to other ultrasound-guided approaches to the saphenous nerve block.23 A limitation of this study was not taking this relatively low success rate into consideration when powering the study. The inclusion of the perceived block failures in the overall statistical analysis gives a true clinical reflection of the ability of this block to reduce postoperative pain scores in the PACU.
Another limitation in this study is the lack of an objective assessment of quadriceps strength. A complete femoral block can provide significant analgesia to the knee but is also associated with quadriceps weakness. Quadriceps weakness can limit mobility and place patients at risk of falls. The primary benefit of an adductor canal block is to provide analgesia while limiting loss of quadriceps strength, presumably by blocking only the saphenous nerve, the nerve to the vastus medialis, and potentially the articular contribution of the obturator nerve to the knee joint.10–12 We did not objectively measure quadriceps strength due to the outpatient nature of the primary surgical procedure. Indirectly, all patients were able to stand in the PACU, and no study participant mentioned subjective leg weakness or reported falls at the 24-hr follow-up interview.
Finally, these results based on a small sample size and a relatively homogeneous patient population treated at a single centre should be generalized with caution. Results for secondary analyses are included to give a complete clinical picture, but as there was no adjustment for multiple comparisons, these findings should be considered supportive only. Even so, this randomized comparison of adductor canal block vs placebo for arthroscopic medial meniscectomy provides evidence that adductor canal block is a practicable treatment option that could benefit a large number of patients undergoing arthroscopic knee surgery. In addition, the consistency of the primary findings across a broad range of statistical model assumptions bodes well for future studies that could bring this technique into widespread clinical use. Further randomized studies will be necessary to evaluate the adductor canal block for other common ambulatory lower extremity surgeries as these results are based on arthroscopic medial meniscectomy only.
In conclusion, we showed that there is significant improvement in mean resting NRS pain scores on PACU admission for those patients receiving ultrasound-guided adductor canal blocks for arthroscopic medial meniscectomy. Our secondary endpoints, 24-hr postoperative opioid consumption and pain scores up to 24 hr, were also reduced, but we did not power for these in the initial study design. The adductor canal block has become possible only since the introduction of ultrasound for regional anesthesia, so there are limited data on the benefits and risks. Currently, we have not seen reports in the literature of nerve injury or local anesthetic systemic toxicity from this nerve block, and we have not seen either of these effects at our institution.24 Based on the results of this study, the adductor canal block can be an important part of a multimodal approach to postoperative analgesia for arthroscopic knee surgery.
References
Iskandar H, Benard A, Ruel-Raymond J, Cochard G, Manaud B. Femoral block provides superior analgesia compared with intra-articular ropivacaine after anterior cruciate ligament reconstruction. Reg Anesth Pain Med 2003; 28: 29-32.
Ilfeld BM, Duke KB, Donohue MC. The association between lower extremity continuous peripheral nerve blocks and patient falls after knee and hip arthroplasty. Anesth Analg 2010; 111: 1552-4.
Muraskin SI, Conrad B, Zheng N, Morey TE, Enneking FK. Falls associated with lower-extremity-nerve blocks: a pilot investigation of mechanisms. Reg Anesth Pain Med 2007; 32: 67-72.
Fortier J, Chung F, Su J. Unanticipated admission after ambulatory surgery–a prospective study. Can J Anaesth 1998; 45: 612-9.
Akkaya T, Ersan O, Ozkan D, et al. Saphenous nerve block is an effective regional technique for post-menisectomy pain. Knee Surg Sports Traumatol Arthrosc 2008; 16: 855-8.
Kapoor R, Adhikary SD, Siefring C, McQuillan PM. The saphenous nerve and its relationship to the nerve to the vastus medialis in and around the adductor canal: an anatomical study. Acta Anaesthesiol Scand 2012; 56: 365-7.
Horn JL, Pitsch T, Salinas F, Benninger B. Anatomic basis to the ultrasound-guided approach for saphenous nerve blockade. Reg Anesth Pain Med 2009; 34: 486-9.
Benzon HT, Sharma S, Calimaran A. Comparison of the different approaches to saphenous nerve block. Anesthesiology 2005; 102: 633-8.
Manickam B, Perlas A, Duggan E, Brull R, Chan VW, Ramlogan R. Feasibility and efficacy of ultrasound-guided block of the saphenous nerve in the adductor canal. Reg Anesth Pain Med 2009; 34: 578-80.
Ishiguro S, Yokochi A, Yoshioka K, et al. Technical communication: anatomy and clinical implications of ultrasound-guided selective femoral nerve block. Anesth Analg 2012; 115: 1467-70.
Lund J, Jenstrup MT, Jaeger P, Sorensen AM, Dahl JB. Continuous adductor-canal-blockade for adjuvant post-operative analgesia after major knee surgery: preliminary results. Acta Anaesthesiol Scand 2011; 55: 14-9.
Horner G, Dellon AL. Innervation of the human knee joint and implications for surgery. Clin Orthop Relat Res 1994; 301: 221-6.
Jenstrup MT, Jaeger P, Lund J, et al. Effects of adductor-canal-blockade on pain and ambulation after total knee arthroplasty: a randomized study. Acta Anaesthesiol Scand 2012; 56: 357-64.
McGuirk S, Fahy C, Costi D, Cyna AM. Use of invasive placebos in research on local anaesthetic interventions. Anaesthesia 2011; 66: 84-91.
Shaheen PE, Walsh D, Lasheen W, Davis MP, Lagman RL. Opioid equianalgesic tables: are they all equally dangerous? J Pain Symptom Manage 2009; 38: 409-17.
Farrar JT, Young JP Jr, LaMoreaux L, Werth JL, Poole RM. Clinical importance of changes in chronic pain intensity measured on an 11-point numerical pain rating scale. Pain 2001; 94: 149-58.
Solheim N, Rosseland LA, Stubhaug A. Intra-articular morphine 5 mg after knee arthroscopy does not produce significant pain relief when administered to patients with moderate to severe pain via an intra-articular catheter. Reg Anesth Pain Med 2006; 31: 506-13.
Ekman EF, Wahba M, Ancona F. Analgesic efficacy of perioperative celecoxib in ambulatory arthroscopic knee surgery: a double-blind, placebo-controlled study. Arthroscopy 2006; 22: 635-42.
Kim S, Bosque J, Meehan JP, Jamali A, Marder R. Increase in outpatient knee arthroscopy in the United States: a comparison of National Surveys of Ambulatory Surgery, 1996 and 2006. J Bone Joint Surg Am 2011; 93: 994-1000.
Hawker G, Guan J, Judge A, Dieppe P. Knee arthroscopy in England and Ontario: patterns of use, changes over time, and relationship to total knee replacement. J Bone Joint Surg Am 2008; 90: 2337-45.
Todd KH, Funk KG, Funk JP, Bonacci R. Clinical significance of reported changes in pain severity. Ann Emerg Med 1996; 27: 485-9.
Kelly AM. Does the clinically significant difference in visual analog scale pain scores vary with gender, age, or cause of pain? Acad Emerg Med 1998; 5: 1086-90.
Tsai PB, Karnwal A, Kakazu C, Tokhner V, Julka IS. Efficacy of an ultrasound-guided subsartorial approach to saphenous nerve block: a case series. Can J Anesth 2010; 57: 683-8.
Henningsen MH, Jaeger P, Hilsted KL, Dahl JB. Prevalence of saphenous nerve injury after adductor-canal-blockade in patients receiving total knee arthroplasty. Acta Anaesthesiol Scand 2013; 57: 112-7.
Funding sources
None.
Conflict of interest
David Auyong has received honoraria for lectures and has carried out research with SonoSite, although not related to this study in any way. No other author has a conflict of interest to disclose.
Author information
Authors and Affiliations
Corresponding author
Additional information
Author contributions
Neil A. Hanson and Francis V. Salinas were involved in the study design. Neil A. Hanson, Ryan E. Derby, David B. Auyong, Christina Delucca, and Ryan Nagy were involved in enrolment of patients and data collection. Neil A. Hanson, Ryan E. Derby, David B. Auyong, Zhuoxin Yu, and April E. Slee were involved in data analysis. Neil A. Hanson, Ryan E. Derby, David B. Auyong, Francis V. Salinas, and April E. Slee were involved in manuscript preparation. Neil A. Hanson reviewed the original study data and data analysis and is the archival author.
Rights and permissions
About this article
Cite this article
Hanson, N.A., Derby, R.E., Auyong, D.B. et al. Ultrasound-guided adductor canal block for arthroscopic medial meniscectomy: a randomized, double-blind trial. Can J Anesth/J Can Anesth 60, 874–880 (2013). https://doi.org/10.1007/s12630-013-9992-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12630-013-9992-9