Abstract
Purpose
This study is a feasibility assessment to determine the ability of novice users to utilize an infrared (IR) sensor stylet as a guide to position the tip of the endotracheal tube (ETT) 40 mm proximal to the carina in the swine trachea.
Methods
We developed a stylet system using an IR sensor attached to the tip of a stylet to facilitate measuring the distance of the ETT from the carina. The indicator lamp of the IR sensor system turns on through calibration when the ETT tip arrives at a point 20 mm proximal to the carina. In order to place the ETT tip 40 mm (middle of 20-60 mm) from the carina after the indicator lamp turns on, the operator uses the ETT marker to withdraw the ETT 20 mm. For this study, five fresh swine airways were used in random order after drawing lots, and ten novices were recruited to attempt the procedure ten times on each swine’s airway.
Results
Five hundred endotracheal intubations were performed. For the target distance of 40 mm from the ETT tip to the carina, the mean (standard deviation) of the total data set was 37.9 (3.5) mm; all data were within a 20-60 mm range (500/500), and 98.2% (491/500) of the attempts fell within the 30-50 mm range.
Conclusions
The IR sensor stylet system can facilitate correct positioning of the ETT tip at an appropriate depth above the carina in the swine trachea. Evaluation of the IR sensor stylet methodology in human subjects is warranted.
Résumé
Objectif
Cette étude est une évaluation de faisabilité pour déterminer la capacité de novices de se servir d’un mandrin muni d’un capteur infrarouge (IR) comme guide pour placer l’extrémité d’une sonde endotrachéale (SET) à 40 mm de la carène dans la trachée d’un porc.
Méthode
Nous avons mis au point un système de mandrin en fixant un capteur IR à la pointe d’un mandrin pour faciliter la mesure de la distance entre la SET et la carène. Nous avons calibré le système de façon à ce que la lampe indicatrice du système de capteur IR s’allume lorsque la pointe de la SET atteint un point situé à 20 mm de la carène. Afin de placer la pointe de la SET à 40 mm (milieu de 20-60 mm) de la carène une fois que la lampe indicatrice s’est allumée, l’opérateur se sert du marqueur de la SET pour retirer la SET de 20 mm. Pour cette étude, nous avons utilisé cinq voies aériennes fraîches de porc de façon aléatoire après tirage au sort, et dix novices ont été recrutés afin de tenter l’intervention dix fois sur chacune des voies aériennes porcines.
Résultats
Cinq cents intubations endotrachéales ont été réalisées. Pour la distance cible de 40 mm entre la pointe de la SET et la carène, la moyenne (écart type) de l’ensemble total de données était de 37,9 (3,5) mm; toutes les données se situaient entre 20 et 60 mm (500/500), et 98,2 % (491/500) des tentatives se sont situées entre 30 et 50 mm.
Conclusion
Le système de mandrin muni d’un capteur IR peut faciliter le positionnement correct de l’extrémité de la SET à une profondeur adéquate au-dessus de la carène dans une trachée porcine. L’évaluation d’une méthodologie de mandrin muni d’un capteur IR chez l’humain est de mise.
Similar content being viewed by others
When performing endotracheal intubation, the distal tip of the endotracheal tube (ETT) should be placed in the trachea at the correct depth,1,2 i.e., in the middle third of the trachea approximately 20-60 mm from the carina in adult subjects.2 Bronchial intubation, which occurs when the ETT is placed too deeply, is the most common cause of arterial desaturation.3 If bronchial intubation is unrecognized, it can lead to collapse of the contralateral lung and hyperinflation of the intubated lung.4 If the ETT tip is placed in the first third of the trachea (i.e., too shallow placement), extubation may occur because of a change in the patient’s head position.5 Morray et al. 6 reported that bronchial intubation occurred in 1% of adverse claims in both pediatric and adult patients. They also found that inadvertent and premature extubation occurred in 6% of adverse claims in pediatric cases and 2% of adverse claims in adult cases.6
Widely used methods to ensure correct placement of the tip of the ETT include chest radiography, referencing the marks on the ETT (i.e., securing orally placed tracheal tubes at the upper incisor teeth or gums at the 22-cm mark in men and at the 20-cm mark in women of average build), capnography, auscultation, transtracheal illumination, and fibroscopy.7-14 Recently, ultrasound, video sensor, and radio-frequency identification (RFID) have been introduced as alternative methods.15-18 Chest radiography is considered the gold standard for confirming the correct depth of ETT placement; however, it is not possible to use chest radiography in a situation outside the hospital, and it is difficult to use it frequently in the intensive care unit because of the inherent radiation exposure.7,18 Capnography, which estimates end-tidal carbon dioxide (CO2) by using infrared rays, is one of the best methods to confirm ETT placement; however, it cannot calculate the distance from the tip of the ETT to the carina.10,11 Bilateral auscultation of the chest has been used most widely and is recommended to diagnose and prevent bronchial intubation.13 Sitzwohl et al. 14 reported that the sensitivity and specificity of auscultation were 65% and 93%, respectively. Additionally, because the proper depth of the ETT cannot be measured with auscultation, less experienced operators would probably need to rely more on referencing the marks on the tube than on auscultation.14
In this study, we introduce a novel stylet, the infrared (IR) sensor stylet that can be used to confirm the ETT position by calculating the distance from the carina to the tip of the ETT using an IR sensor. The IR sensors used extensively for measuring distance are less expensive and have faster response times than ultrasonic sensors. When compared with the ultrasonic sensor for distance measurement, the IR sensor can be used at a closer distance, and its size can be minimized more easily for insertion into the ETT.19 Further, IR sensors are not harmful in humans and can be used when available outside the hospital. Taking all of these factors into account, we considered the IR sensor stylet to be an appropriate instrument to use in a study designed to evaluate the proper placement of the ETT tip (20-60 mm from the carina). This study was designed to assess the ability of novice users to utilize the IR sensor stylet as a guide for positioning the tip of the ETT 40 mm proximal to the carina in a swine tracheal model.
Methods
The Institutional Review Board at Hanyang University Hospital approved this study. Fig. 1 shows the configuration of the stylet system that uses IR rays to measure the distance from the tip of the ETT (MM61110075; Unomedical Sdn. Bhd., Malaysia; inner-diameter 7.5 mm, outer diameter 10 mm, length 315 mm) to the carina. We used the IR sensor (TCRT5000; Vishay Technology Inc., PA USA) to measure the proper location of the ETT tip. The IR sensor is composed of an IR light-emitting diode that has a wavelength of 950 nm and a phototransistor that generates an electric current proportional to the incoming light intensity. We attached the IR sensor to the tip of the stylet that guides the ETT, and as a general rule, the stylet is inserted into the ETT during intubation. As the ETT tip enters through the trachea and approaches the carina, the reflected IR ray becomes stronger as the sensor position (i.e., ETT tip) comes closer to the carina. This increases the output signal level of the IR sensor system. When the distance from the ETT tip to the carina is less than the preset level (e.g., 20 mm), the sensor system turns on the indicator lamp (Fig. 2c), which alerts the operator that the ETT tip is positioned at the specific location relative to the carina. Fig. 2 shows the implementation of the sensor system and ETT.
(a) Overall shape of the infrared (IR) sensor stylet system. The IR sensor is attached to the stylet that is inserted into the endotracheal tube (ETT); (b) The ETT tip. The IR sensor is composed of an IR-emitting diode and phototransistor; (c) The electric circuit of the IR sensor stylet system. When the IR sensor reaches a specific position, the indicator lamp is turned on. The specific position can be adjusted with a potentiometer; (d) Outer shape of the ETT. A centimetre scale is marked on the surface of the ETT
When measuring distance using the IR sensor, the IR ray is emitted and the IR ray reflected from the surface of an object enters the phototransistor. The distance from the sensor to the object is inversely proportional to the incoming IR light intensity and is influenced by noise.19 Consequently, the distance measured using the IR sensor is dependent on the surface properties of the object, such as the spectral reflectance and the geometric shape of the surface. For this reason, the distance measurement system should be calibrated in the environment where it will be utilized. In this study, the IR sensor system was calibrated in a mannequin (Airway Management Trainer; Laerdal® Medical, Norway) and in an animal model separately and used in each environment separately. Thus, we expected that the IR sensor stylet system could be used after calibration and that the error would be within a small range.
The final goal of intubation is to place the tip of the ETT in a position in the middle (i.e., 40 mm from the carina) of the suggested location (i.e., 20-60 mm from carina) after calibration. Our IR sensor system showed stable operation at a shorter distance. As a result, we established procedures whereby the operator, after identifying a position 20 mm from the carina, withdrew the ETT 20 mm in order to place it 40 mm above the carina.
Prior to the animal experiment shown in Fig. 3a, we confirmed operation of the IR sensor system using the mannequin. The inner wall of the mannequin airway is made of red silicon. For the experiment on the mannequin, we calibrated the IR sensor stylet system using the potentiometer (Fig. 2c), which can adjust the ETT tip to a location 20 mm from the carina, and we checked the result with a vernier caliper. The process of calibration could then be set to find a position 20 mm above the carina during the mannequin study.
(a) Confirmation of the calibration process in the mannequin; (b) Confirmation of the distance from the tip of the endotracheal tube to the carina in animal experiments. To measure the distance, the wall of the trachea has a pi (Π)-shaped opening which is already incised. After measurement, the opening is closed
Since the reflective properties of a swine airway differ from those of a mannequin, the animal experiments were conducted after performing calibration for the swine airway.
Experimental setup
A convenience sample of ten student volunteers took part in this preliminary study. Participants were third-year residents in a department of biomedical engineering at one university who had no prior experience with tracheal intubation. The purpose of the study and details of the procedure were explained to each participant before they began the experiment. No incentives were offered for participation in this study.
For the experiment, we used five dissected fresh swine airways that consisted of anatomical structures from the thyroid cartilage to the mainstem bronchi. The mean (standard deviation) length from the vocal cord to the carina was 214 (27) mm. Each airway was mounted on a separate wooden board (200 mm × 300 mm × 15 mm) and labelled as A, B, C, D, and E. Each swine airway was then covered with a cloth so the operator could not recognize the characteristics of the swine trachea being used. Using the mannequin’s airway, each operator practiced the following steps five times:
-
1)
Insert the IR sensor (end of the stylet) to the end of the ETT tip.
-
2)
After locating the glottic area, insert the ETT through the glottic opening and advance the ETT forward.
-
3)
Stop advancing the ETT at the moment when the indicator lamp of the IR sensor system turns on.
-
4)
Using the markings on the ETT as a guide, withdraw the ETT a 20-mm distance (Fig. 2d).
-
5)
Secure the ETT with one hand and remove the stylet from the ETT.
Ten operators performed the above procedure on five cloth-covered swine airways in a random order after drawing lots (e.g., A → C → E → D → B). This set of intubations was repeated ten times with a different order (e.g., B → D → A → E → C). At the end of each procedure, two authors (Y. S. and Y. C.) uncovered the cloth, independently measured the distance from the ETT tip to the carina in mm using a vernier caliper through the pre-made incision (i.e., a pi (Π)-shaped opening) in the wall of the trachea, and reached consensus on the measurement (Fig. 3). After measurement, the opening in the wall of the trachea was closed. The total number of attempts was 500 (ten operators × five swine airways × ten intubations).
The means, standard deviations (SD), and 95% confidence intervals (CI) of the distances from the carina to the ETT tip were measured. We also calculated the percentage of data showing intubation depth within the ranges of 20-60 mm and 30-50 mm as surrogate outcomes for verification of the proper positioning of the ETT tip.
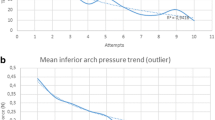
Results
All attempts were successfully completed within 20 sec. Combining all the data, the mean (SD) distance from the carina to the ETT tip was 37.9 (3.5) mm (95% CI 36.7 to 38.2). The minimum distance was 28 mm and the maximum distance was 55 mm. As shown in Fig. 4, all the results fell within the 20-60 mm range, and 98.2% of the values were in the 30-50 mm range (491/500). To determine if there was a learning effect, we calculated the mean (SD) of the first, sixth, and last set of trials of all operators with the following results: 38.0 (3.6) mm, 37.8 (3.2) mm, and 38.4 (3.9) mm, respectively.
Discussion
The incidence of mainstem bronchi and esophageal intubation, verified by chest radiography, is 12%.20 Rigini et al. 8 found 26/44 (59.1%) cases in which ETTs were not in the 30-50 mm range.8 In their study, the mean (SD) distance was 37.9 (3.5) mm, which was in accordance with the findings in our study. Their findings were possibly due to a difference in the reflection of IR rays from each sample. In addition, the 20-mm extraction of the ETT after the indicator lamp was turned on might be different in each case. Nevertheless, when performing endotracheal intubation using the IR sensor stylet, the ETT tip was located 20-60 mm above the carina in 100% of cases. The ETT was not located 30-50 mm above the carina in only 9/500 (1.9%) of the cases. In cases involving incorrect placement of the ETT, early detection and prompt correction of ETT positioning after intubation prevents its migration.8 Among the many methods for identifying the correct placement of the ETT, chest radiography and fibreoptic bronchoscopy may be the best techniques7,12; however, it can take several seconds to minutes to obtain the chest radiograph after ETT intubation. The IR sensor stylet is able to identify placement of the ETT instantly during and after intubation. Further, inexperienced operators may have difficulty using fibreoptic bronchoscopes, and both chest radiography and fibreoptic bronchoscopy are not available for use outside the hospital. In our view, the IR sensor stylet is useful for inexperienced operators, and it can also be used in non-hospital settings.
Although capnometry and capnography are widely used during and after intubation to detect whether or not the ETT is placed in the trachea, capnometry does not identify if the ETT tip is at the correct depth, and capnography waveforms usually show a normal pattern even if the ETT is placed in the main bronchus.21,22 While capnography can monitor the concentration of CO2 using IR spectrometry, the IR sensor stylet actually recognizes the specific distance from the sensor to the object by way of IR reflection near the carina. This method helps identify the proper location of the ETT in the bronchus.
Transtracheal illumination may facilitate appropriate placement of the tip of the ETT at a distance 40-60 mm above the carina;23 however, this technique is difficult to perform in a well-lit environment. In contrast, an IR sensor stylet can be used regardless of the level of light, and it may help adjust the position of the ETT without the use of chest radiography. This can be particularly useful in a critical care setting, such as in the intensive care unit where the body position of the patient is altered in order to avoid pressure sores or to allow for physiotherapy, and in situations that can lead to inappropriate positioning of the ETT despite it being secured.5 Shamir et al. 17 reported that automatic computerized analysis using a video imaging sensor is an accurate method for verifying the ETT position.16,17 It seems that placing the ETT in the middle-third of the trachea would be difficult using this method. Reicher et al. 18 suggested that RFID detectors and RFID tag-labelled ETTs can be used for easy monitoring of the ETT position18; however, it is not possible to place the tip of the ETT at the correct depth because it is only studied once the initial proper placement is confirmed.
Our study had several limitations. First, we assessed the airways obtained from recently dead swine which contained unperfused tissue that differs from the tissue in the human airway. This system should be calibrated in a human airway, i.e., x-ray. Second, the results would not be applicable for pediatric airway management. Third, the study did not evaluate the IR sensor stylet under conditions that interfere with reflected IR rays, such as pulmonary bleeding or edema, bronchial secretions, or the presence of an endotracheal mass. Fourth, we did not investigate the effects of using the IR sensor stylet to place the ETT in the human esophagus. If the IR sensor stylet were inserted into the human esophagus, it is possible that the reflection might occur within 20 mm from the esophageal wall, causing the indicator lamp to be turned on continuously.
In conclusion, the novel IR sensor stylet may be effective in positioning the tip of the ETT at an appropriate depth above the carina after ETT tube insertion in the swine trachea. Further evaluation of the utility of the IR sensor stylet in varying airway conditions and in the human trachea is warranted in order to determine its applicability to clinical situations.
References
Neumar RW, Otto CW, Link MS, et al. Part 8: Adult advanced cardiovascular life support: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 2010; 122: S729-67.
Salem MR. Verification of endotracheal tube position. Anesthesiol Clin North America 2001; 19: 813-39.
Szekely SM, Webb RK, Williamson JA, Russell WJ. The Australian Incident Monitoring Study. Problems related to the endotracheal tube: an analysis of 2000 incident reports. Anaesth Intensive Care 1993; 21: 611-6.
Owen RL, Cheney FW. Endobronchial intubation: A preventable complication. Anesthesiology 1987; 67: 255-7.
Kim JT, Kim HJ, Ahn W, et al. Head rotation, flexion, and extension alter endotracheal tube position in adults and children. Can J Anesth 2009; 56: 751-6.
Morray JP, Geiduschek JM, Caplan RA, Posner KL, Gild WM, Cheney FW. A comparison of pediatric and adult anesthesia closed malpractice claims. Anesthesiology 1993; 78: 461-7.
Brunel W, Coleman DL, Schwartz DE, Peper E, Cohen NH. Assessment of routine chest roentgenograms and the physical examination to confirm endotracheal tube position. Chest 1989; 96: 1043-5.
Rigini N, Boaz M, Ezri T, et al. Prompt correction of endotracheal tube positioning after intubation prevents further inappropriate positions. J Clin Anesth 2011; 23: 367-71.
Falzone E, Hoffmann C, Pasquier P, Boutonnet M, Tourtier JP. Proper depth placement of oral endotracheal tubes in adults: 21/23 cm or 20/22 cm? J Clin Anesth 2012; 24: 165-6.
Knapp S, Kofler J, Stoiser B, et al. The assessment of four different methods to verify tracheal tube placement in the critical care setting. Anesth Analg 1999; 88: 766-70.
Grmec S. Comparison of three different methods to confirm tracheal tube placement in emergency intubation. Intensive Care Med 2002; 28: 701-4.
Dietrich KA, Conrad SA, Romero MD, Lloyd JL, Fontenot EE. Accuracy of flexible fiberoptic endoscopy in identifying abnormal endotracheal tube positions. Pediatr Emerg Care 1990; 6: 257-9.
Stone DJ. Airway management. In: Miller R (Ed.). Anesthesia, 5th ed. Churchill Livingstone; 2000: 1431-2.
Sitzwohl C, Langheinrich A, Schober A, et al. Endobronchial intubation detected by insertion depth of endotracheal tube, bilateral auscultation, or observation of chest movements: randomised trial. BMJ 2010; 341: c5943.
Chun R, Kirkpatrick AW, Sirois M, et al. Where’s the tube? Evaluation of hand-held ultrasound in confirming endotracheal tube placement. Prehosp Disaster Med 2004; 19: 366-9.
Lederman D, Lampotang S, Shamir MY. Automatic endotracheal tube position confirmation system based on image classification - a preliminary assessment. Med Eng Phys 2011; 33: 1017-26.
Shamir MY, Lederman D, Gravenstein D. Automatic computerized endotracheal tube position verification: an animal model evaluation. Anesth Analg 2011; 113: 1411-5.
Reicher J, Reicher D, Reicher M. Use of radio frequency identification (RFID) tags in bedside monitoring of endotracheal tube position. J Clin Monit Comput 2007; 21: 155-8.
Mohammad T. Using ultrasonic and infrared sensors for distance measurement. World Academy of Science, Engineering and Technology 2009; 27: 293-8.
Schwartz DE, Matthay MA, Cohen NH. Death and other complications of emergency airway management in critically ill adults. A prospective investigation of 297 tracheal intubations. Anesthesiology 1995; 82: 367-76.
Hagberg CA. Benumof’s airway management. Principles and Practice, 2nd ed. Mosby: Elsevier; 2007: 1061-3.
Gilbert D, Benumof JL. Biphasic carbon dioxide elimination waveform with right mainstem bronchial intubation. Anesth Analg 1989; 69: 829-32.
Stewart RD, LaRosee A, Stoy WA, Heller MB. Use of a lighted stylet to confirm correct endotracheal tube placement. Chest 1987; 92: 900-3.
Acknowledgements
The authors acknowledge that the original and subsequently revised manuscripts underwent language editing by Editage, a division of Cactus Communications Pvt Ltd. Neither the research content nor the authors’ intentions were altered during this editing process. This work was supported by a National Research Foundation grant funded by the Korean Government (MEST) (2009-0064912).
Conflicts of interest
None declared.
Author information
Authors and Affiliations
Corresponding author
Additional information
Author contributions
Jaehoon Oh and Youngjoon Chee helped with study conception and design and obtained research funding. Youngjoon Chee, Hyunggoo Kang, and Yeongtak Song developed the sensor and recording system. Taeho Lim and Youngsuk Cho supervised the conduct of the trial and data collection. Jaehoon Oh, Youngjoon Chee, and Youngsuk Cho recruited the participants and managed the data, including quality control. Yeongtak Song drafted the manuscript. All authors read and contributed to the manuscript and approved the revisions. Jaehoon Oh assumes responsibility for the paper as a whole.
Rights and permissions
About this article
Cite this article
Song, Y., Oh, J., Chee, Y. et al. A novel method to position an endotracheal tube at the correct depth using an infrared sensor stylet. Can J Anesth/J Can Anesth 60, 444–449 (2013). https://doi.org/10.1007/s12630-013-9898-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12630-013-9898-6