Abstract
Purpose of Review
Upper extremity lymphedema is a much-feared complication of breast cancer treatment leading to significant impairments in patients’ quality of life. The mainstay of treatment for this debilitating chronic disease has been non-surgical modalities, namely complete decongestive therapies. Surgical treatment of lymphedema has emerged as an option for patients who have exhausted these conservative measures and consists of both physiologic procedures (vascularized lymph node transplant and lymphovenous bypass) which aim to reduce the burden of lymphatic fluid and reductive procedures to remove excess soft tissue.
Recent Findings
Opinions vary among surgeons regarding the appropriate surgical indications in patients with different stages of lymphedema for each type of surgery, as well as the optimal donor site for lymph node transplant, and recent studies are beginning to address these questions. Additionally, there is growing data regarding the benefits of preventative lymphatic surgery at the time of axillary lymph node dissection, as well as the cost effectiveness of this approach.
Summary
Surgical approaches for the prevention and treatment of breast cancer–related lymphedema are gaining popularity as a means of improving patients’ quality of life. There is an expanding body of literature demonstrating the effectiveness of these surgical procedures in terms of reduction in arm circumference, decreased cellulitis incidence, and overall quality of life, as well as emerging evidence of their cost effectiveness.

Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Silva AK, Chang DW. Vascularized lymph node transfer and lymphovenous bypass: novel treatment strategies for symptomatic lymphedema. J Surg Oncol. 2016;113(8):932–9.
Lawenda BD, Mondry TE, Johnstone PAS. Lymphedema: a primer on the identification and management of a chronic condition in oncologic treatment. CA Cancer J Clin. 2009;59:8–24.
Rockson SG, Rivera KK. Estimating the population burden of lymphedema. Ann N Y Acad Sci. 2008;1131:147–54.
DiSipio T, Rye S, Newman B, Hayes S. Incidence of unilateral arm lymphoedema after breast cancer: a systematic review and meta-analysis. Lancet Oncol. 2013;14(6):500–15.
• Johnson AR, Kimball S, Epstein S, Recht A, Lin SJ, Lee BT, et al. Lymphedema incidence after axillary lymph node dissection: quantifying the impact of radiation and the lymphatic microsurgical preventive healing approach. Ann Plast Surg. 2019;82(4S Suppl 3):S234–41. The authors look systematically at the outcomes of LYMPHA as a preventative approach to mitigating breast cancer-related lymphedema rates in the setting of axillary node dissection with or without radiation and show that it is significantly effective in decreasing lymphedema rates in both settings.
Taghian NR, Miller CL, Jammallo LS, O’Toole J, Skolny MN. Lymphedema following breast cancer treatment and impact on quality of life: a review. Crit Rev Oncol Hematol. 2014;92(3):227–34.
Shaitelman SF, Cromwell KD, Rasmussen JC, Stout NL, Armer JM, Lasinski BB, et al. Recent progress in the treatment and prevention of cancer-related lymphedema. CA Cancer J Clin. 2015;65:55–81.
Dean LT, Ransome Y, Frasso-Jaramillo L, Moss SL, Zhang Y, Ashing K, et al. Drivers of cost differences between US breast cancer survivors with or without lymphedema. J Cancer Surviv. 2019;13(5):804–14.
De Vrieze T, Nevelsteen I, Thomis S, De Groef A, Tjalma WAA, Gebruers N, et al. What are the economic burden and costs associated with the treatment of breast cancer-related lymphoedema? A systematic review. Support Care Cancer. 2020;28(2):439–49.
Chang DW, Masia J, Garza R, Skoracki R, Neligan PC. Lymphedema: surgical and medical therapy. Plast Reconstr Surg. 2016;138(3):209S–18S.
Rockson SG. Lymphedema after breast cancer treatment. N Engl J Med. 2018;379(20):1937–44.
Scaglioni MF, Fontein DBY, Arvanitakis M, Giovanoli P. Systematic review of lymphovenous anastomosis (LVA) for the treatment of lymphedema. Microsurgery. 2017;37(8):947–53.
Goldsmith HS. Long term evaluation of omental transposition for chronic lymphedema. Ann Surg. 1974;180(6):847–9.
Badash I, Gould DJ, Patel KM. Supermicrosurgery: history, applications, Training and the Future. Front Surg. 2018;5(March):1–13.
Granzow JW. Lymphedema surgery: the current state of the art. Clin Exp Metastasis. 2018;35(5–6):553–8. https://doi.org/10.1007/s10585-018-9897-7 [Internet].
Dayan JH, Ly CL, Kataru RP, Mehrara BJ. Lymphedema: pathogenesis and novel therapies. Annu Rev Med. 2018;69(1):263–76.
Suami H, Chang DW. Overview of surgical treatments for breast cancer-related lymphedema. Plast Reconstr Surg. 2010;126(6):1853–63.
Garza RM, Chang DW. Lymphovenous bypass for the treatment of lymphedema. J Surg Oncol. 2018;118(5):743–9.
Torrisi JS, Joseph WJ, Ghanta S, Cuzzone DA, Albano NJ, Savetsky IL, et al. Lymphaticovenous bypass decreases pathologic skin changes in upper extremity breast cancer-related lymphedema. Lymphat Res Biol. 2015;13(1):46–53.
Chen WF, Yamamoto T, Fisher M, Liao J, Carr J. The “octopus” lymphaticovenular anastomosis: evolving beyond the standard Supermicrosurgical technique. J Reconstr Microsurg. 2015;31(6):450–7.
Chang DW, Suami H, Skoracki R. A prospective analysis of 100 consecutive lymphovenous bypass cases for treatment of extremity lymphedema. Plast Reconstr Surg. 2013;132(5):1305–14.
AlJindan FK, Lin CY, Cheng MH. Comparison of outcomes between side-to-end and end-to-end lymphovenous anastomoses for early-grade extremity lymphedema. Plast Reconstr Surg. 2019;144(2):486–96.
Campisi C, Eretta C, Pertile D, Da Rin E, Campisi C, Maccio A, et al. BF. Microsurgery for treatment of peripheral lymphedema: long-term outcome and future perspectives. Microsurgery. 2007;27:333–8.
Koshima I, Nanba Y, Tsutsui T, Takahashi Y, Itoh S, Fujitsu M. Minimal invasive lymphaticovenular anastomosis under local anesthesia for leg lymphedema: is it effective for stage III and IV? Ann Plast Surg. 2004;53(3):261–6.
Garza RM, Ooi ASH, Falk J, Chang DW. The relationship between clinical and indocyanine green staging in lymphedema. Lymphat Res Biol. 2019;17(3):329–33.
Hara H, Mihara M, Seki Y, Todokoro T, Iida T, Koshima I. Comparison of indocyanine green lymphographic findings with the conditions of collecting lymphatic vessels of limbs in patients with lymphedema. Plast Reconstr Surg. 2013;132(6):1612–8.
• Coriddi M, Dayan J, Sobti N, Nash D, Goldberg J, Klassen A, et al. Systematic review of patient-reported outcomes following surgical treatment of lymphedema. Cancers (Basel). 2020;12(3):1–18. The authors emphasize the importance of patient-reported outcomes when determining the value of lymphatic surgery, more so than measures of volume or circumference, as these subjective and objective measures are not correlated. In their systematic review, they find significant benefit of LVB and VLNT when looking at patient-reported outcome measures.
Gould DJ, Mehrara BJ, Neligan P, Cheng MH, Patel KM. Lymph node transplantation for the treatment of lymphedema. J Surg Oncol. 2018;118(5):736–42.
Lin CH, Ali R, Chen SC, Wallace C, Chang YC, Chen HC, et al. Vascularized groin lymph node transfer using the wrist as a recipient site for management of postmastectomy upper extremity lymphedema. Plast Reconstr Surg. 2009;123(4):1265–75.
Becker C, Vasile JV, Levine JL, Batista BN, Studinger RM, Chen CM, et al. Microlymphatic surgery for the treatment of iatrogenic lymphedema. Clin Plast Surg. 2012;39(4):385–98.
Liu HL, Pang SY, Lee CC, Wong MMK, Chung HP, Chan YW. Orthotopic transfer of vascularized groin lymph node flap in the treatment of breast cancer-related lymphedema: clinical results, lymphoscintigraphy findings, and proposed mechanism. J Plast Reconstr Aesthet Surg. 2018;71(7):1033–40.
Suami H, Scaglioni MF, Dixon KA, Tailor RC. Interaction between vascularized lymph node transfer and recipient lymphatics after lymph node dissection—a pilot study in a canine model. J Surg Res. 2016;204(2):418–27.
Cheng MH, Chen SC, Henry SL, Tan BK, Chia-Yu Lin M, Huang JJ. Vascularized groin lymph node flap transfer for postmastectomy upper limb lymphedema: flap anatomy, recipient sites, and outcomes. Plast Reconstr Surg. 2013;131(6):1286–98.
Tzou CH, Meng S, Ines T, Reissig L, Pichler U, Steinbacher J, et al. Surgical anatomy of the vascularized submental lymph node flap: anatomic study of correlation of submental artery perforators and quantity of submental lymph node. J Surg Oncol. 2017;115(1):54–9.
Ooi ASH, Chang DW. 5-step harvest of supraclavicular lymph nodes as vascularized free tissue transfer for treatment of lymphedema. J Surg Oncol. 2017;115(1):63–7.
Inbal A, Teven CM, Chang DW. Latissimus dorsi flap with vascularized lymph node transfer for lymphedema treatment: technique, outcomes, indications and review of literature. J Surg Oncol. 2017;115(1):72–7.
Nguyen AT, Suami H, Hanasono MM, Womack VA, Wong FC, Chang EI. Long-term outcomes of the minimally invasive free vascularized omental lymphatic flap for the treatment of lymphedema. J Surg Oncol. 2017;115(1):84–9.
Coriddi M, Wee C, Meyerson J, Eiferman D, Skoracki R. Vascularized jejunal mesenteric lymph node transfer: a novel surgical treatment for extremity lymphedema. J Am Coll Surg. 2017;225(5):650–7.
Chang EI, Masià J, Smith ML. Combining autologous breast reconstruction and vascularized lymph node transfer. Semin Plast Surg. 2018;32(1):36–41.
Raju A, Chang DW. Vascularized lymph node transfer for treatment of lymphedema: a comprehensive literature review. Ann Surg. 2015;261(5):1013–23.
Pappalardo M, Patel K, Cheng MH. Vascularized lymph node transfer for treatment of extremity lymphedema: an overview of current controversies regarding donor sites, recipient sites and outcomes. J Surg Oncol. 2018;117(7):1420–31.
Ho OA, Lin CY, Pappalardo M, Cheng MH. Comparisons of submental and groin vascularized lymph node flaps transfer for breast cancer-related lymphedema. Plast Reconstr Surg Glob Open. 2018;6(12):1–9.
Ciudad P, Agko M, Perez Coca JJ, Manrique OJ, Chang WL, Nicoli F, et al. Comparison of long-term clinical outcomes among different vascularized lymph node transfers: 6-year experience of a single center’s approach to the treatment of lymphedema. J Surg Oncol. 2017;116(6):671–82.
Scaglioni MF, Arvanitakis M, Chen Y-C, Giovanoli P, Yang JC-S, Chang EI. Comprehensive review of vascularized lymph node transfers for lymphedema: outcomes and complications. Microsurgery. 2018;38:222–9.
Patel KM, Lin CY, Cheng MH. From theory to evidence: long-term evaluation of the mechanism of action and flap integration of distal vascularized lymph node transfers. J Reconstr Microsurg. 2015;31(1):26–30.
Ozturk CN, Ozturk C, Glasgow M, Platek M, Ashary Z, Kuhn J, et al. Free vascularized lymph node transfer for treatment of lymphedema: a systematic evidence based review. J Plast Reconstr Aesthet Surg. 2016;69(9):1234–47.
Hassan K, Chang DW. The Charles procedure as part of the modern armamentarium against lymphedema. Ann Plast Surg. 2020.
Brorson H. Liposuction in lymphedema treatment. J Reconstr Microsurg. 2016;32(1):56–65.
Brorson H. From lymph to fat: liposuction as a treatment for complete reduction of lymphedema. Int J Low Extrem Wounds. 2012;11(1):10–9. https://doi.org/10.1177/1534734612438550 [Internet].
Hoffner M, Ohlin K, Svensson B, Manjer J, Hansson E, Troëng T, et al. Liposuction gives complete reduction of arm lymphedema following breast cancer treatment—a 5-year prospective study in 105 patients without recurrence. Plast Reconstr Surg Glob Open. 2018;6(8):1–9.
Carl HM, Walia G, Bello R, Clarke-Pearson E, Hassanein AH, Cho B, et al. Systematic review of the surgical treatment of extremity lymphedema. J Reconstr Microsurg. 2017;33(6):412–25.
Ciudad P, Manrique OJ, Adabi K, Huang TCT, Agko M, Trignano E, et al. Combined double vascularized lymph node transfers and modified radical reduction with preservation of perforators for advanced stages of lymphedema. J Surg Oncol. 2019;119(4):439–48.
Leppäpuska IM, Suominen E, Viitanen T, Rannikko E, Visuri M, Mäki M, et al. Combined surgical treatment for chronic upper extremity lymphedema patients: simultaneous lymph node transfer and liposuction. Ann Plast Surg. 2019;83(3):308–17.
Agko M, Ciudad P, Chen HC. Staged surgical treatment of extremity lymphedema with dual gastroepiploic vascularized lymph node transfers followed by suction-assisted lipectomy—a prospective study. J Surg Oncol. 2018;117(6):1148–56.
Masia J, Pons G, Nardulli ML. Combined surgical treatment in breast Cancer-related lymphedema. J Reconstr Microsurg. 2016;32(1):16–27.
Thompson M, Korourian S, Henry-Tillman R, Adkins L, Mumford S, Westbrook KC, et al. Axillary reverse mapping (ARM): a new concept to identify and enhance lymphatic preservation. Ann Surg Oncol. 2007;14(6):1890–5.
Shao X, Sun B, Shen Y. Axillary reverse mapping (ARM): where to go. Breast Cancer. 2019;26(1):1–10.
Abdelhamid MI, Bari AA, Farid MI, Nour H. Evaluation of axillary reverse mapping (ARM) in clinically axillary node negative breast cancer patients—randomised controlled trial. Int J Surg [internet]. 2020;75(February):174–8. https://doi.org/10.1016/j.ijsu.2020.01.152.
Faisal M, Sayed MG, Antonious K, Abo Bakr A, Farag SH. Prevention of lymphedema via axillary reverse mapping for arm lymph-node preservation following breast cancer surgery: a randomized controlled trial. Patient Saf Surg. 2019;13(1):1–6.
Beek MA, Gobardhan PD, Klompenhouwer EG, Menke-Pluijmers MB, Steenvoorde P, Merkus JW, et al. A patient- and assessor-blinded randomized controlled trial of axillary reverse mapping (ARM) in patients with early breast cancer. Eur J Surg Oncol. 2019;46(1):59–64. https://doi.org/10.1016/j.ejso.2019.08.003 [Internet].
Yuan Q, Wu G, Xiao SY, Hou J, Ren Y, Wang H, et al. Identification and preservation of arm lymphatic system in axillary dissection for breast cancer to reduce arm lymphedema events: a randomized clinical trial. Ann Surg Oncol. 2019;26(11):3446–54.
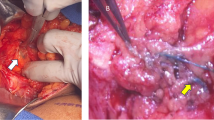
Johnson AR, Singhal D. Immediate lymphatic reconstruction. J Surg Oncol. 2018;118(5):750–7.
Agarwal S, Garza RM, Chang DW. Lymphatic microsurgical preventive healing approach (LYMPHA) for the prevention of secondary lymphedema. Breast J. 2019;(October):1–4.
Boccardo F, Casabona F, De Cian F, Friedman D, Villa G, Bogliolo S, et al. Lymphedema microsurgical preventive healing approach: a new technique for primary prevention of arm lymphedema after mastectomy. Ann Surg Oncol. 2009;16(3):703–8.
Boccardo F, Casabona F, DeCian F, Friedman D, Murelli F, Puglisi M, et al. Lymphatic microsurgical preventing healing approach (LYMPHA) for primary surgical prevention of breast cancer-related lymphedema: Over 4 Years Follow-up. Microsurgery. 2014;(34):421–4.
•• Johnson AR, Asban A, Granoff MD, Kang CO, Lee BT, Chatterjee A, et al. Is immediate lymphatic reconstruction cost-effective? Ann Surg. 2019;XX(Xx):1. First study to look at cost-effectiveness measures of performing prophylactic LVB surgery on patients undergoing axillary lymph node dissections. They provide evidence that this approach is in fact cost-effective.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Lymphedema Incidence, Prevention and Treatment
Rights and permissions
About this article
Cite this article
Rustad, K.C., Chang, D.W. Surgical Approaches to the Prevention and Management of Breast Cancer–Related Lymphedema. Curr Breast Cancer Rep 12, 185–192 (2020). https://doi.org/10.1007/s12609-020-00372-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12609-020-00372-1