Abstract
Purpose of Review
Here we aim to review the association between mammographic density, collagen structure, and breast cancer risk.
Recent Findings
While mammographic density is a strong predictor of breast cancer risk in populations, studies by Boyd show that mammographic density does not predict breast cancer risk in individuals. Mammographic density is affected by age, parity, menopausal status, race/ethnicity, and body mass index (BMI). New studies normalize mammographic density to BMI and this may provide a more accurate way to compare mammographic density in women of diverse race and ethnicity. Preclinical and tissue-based studies have investigated the role collagen composition and structure in predicting breast cancer risk. There is emerging evidence that collagen structure may activate signaling pathways associated with aggressive breast cancer biology.
Summary
Measurement of film mammographic density does not adequately capture the complex signaling that occurs in women with at-risk collagen. New ways to measure at-risk collagen potentially can provide a more accurate view of risk.



Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
•• Boyd NF, Martin LJ, Yaffe MJ, Minkin S. Mammographic density and breast cancer risk: current understanding and future prospects. Breast Cancer Res. 2011;13(6):223. https://doi.org/10.1186/bcr2942. Summary of studies on mammographic density.
Cecchini RS, Costantino JP, Cauley JA, Cronin WM, Wickerham DL, Bandos H, et al. Baseline mammographic breast density and the risk of invasive breast cancer in postmenopausal women participating in the NSABP study of tamoxifen and raloxifene (STAR). Cancer Prev Res. 2012;5(11):1321–9. https://doi.org/10.1158/1940-6207.CAPR-12-0273.
https://www.diagnosticimaging.com/breast-imaging/breast-density-notification-laws-state%2D%2Dinteractive-map. Accessed 03/11/2019.
http://www.nytimes.com/2012/10/25/health/laws-tell-mammogram-clinics-to-address-breast-density.html. Accessed 03/15/2019.
Saslow D, Boetes C, Burke W, Harms S, Leach MO, Lehman CD, et al. American Cancer Society guidelines for breast screening with MRI as an adjunct to mammography. CA Cancer J Clin. 2007;57(2):75–89.
Wolfe JN. Breast patterns as an index of risk for developing breast cancer. AJR Am J Roentgenol. 1976;126(6):1130–7. https://doi.org/10.2214/ajr.126.6.1130.
Yaffe MJ. Mammographic density. Measurement of mammographic density. Breast Cancer Res. 2008;10(3):209. https://doi.org/10.1186/bcr2102.
•• Boyd NF, Rommens JM, Vogt K, Lee V, Hopper JL, Yaffe MJ, et al. Mammographic breast density as an intermediate phenotype for breast cancer. Lancet Oncol. 2005;6(10):798–808. https://doi.org/10.1016/S1470-2045(05)70390-9. Demonstration that mammographic density can be used as an intermediate biomarker of risk in clinical trials.
Carney PA, Miglioretti DL, Yankaskas BC, Kerlikowske K, Rosenberg R, Rutter CM, et al. Individual and combined effects of age, breast density, and hormone replacement therapy use on the accuracy of screening mammography. Ann Intern Med. 2003;138(3):168–75.
Checka CM, Chun JE, Schnabel FR, Lee J, Toth H. The relationship of mammographic density and age: implications for breast cancer screening. AJR Am J Roentgenol. 2012;198(3):W292–5. https://doi.org/10.2214/AJR.10.6049.
Laya MB, Gallagher JC, Schreiman JS, Larson EB, Watson P, Weinstein L. Effect of postmenopausal hormonal replacement therapy on mammographic density and parenchymal pattern. Radiology. 1995;196(2):433–7. https://doi.org/10.1148/radiology.196.2.7617857.
Gierach GL, Loud JT, Chow CK, Prindiville SA, Eng-Wong J, Soballe PW, et al. Mammographic density does not differ between unaffected BRCA1/2 mutation carriers and women at low-to-average risk of breast cancer. Breast Cancer Res Treat. 2010;123(1):245–55. https://doi.org/10.1007/s10549-010-0749-7.
Byrne C, Schairer C, Wolfe J, Parekh N, Salane M, Brinton LA, et al. Mammographic features and breast cancer risk: effects with time, age, and menopause status. J Natl Cancer Inst. 1995;87(21):1622–9.
Vacek PM, Geller BM. A prospective study of breast cancer risk using routine mammographic breast density measurements. Cancer Epidemiol Biomark Prev. 2004;13(5):715–22.
Ziv E, Tice J, Smith-Bindman R, Shepherd J, Cummings S, Kerlikowske K. Mammographic density and estrogen receptor status of breast cancer. Cancer Epidemiol Biomark Prev. 2004;13(12):2090–5.
Eng-Wong J, Orzano-Birgani J, Chow CK, Venzon D, Yao J, Galbo CE, et al. Effect of raloxifene on mammographic density and breast magnetic resonance imaging in premenopausal women at increased risk for breast cancer. Cancer Epidemiol Biomark Prev. 2008;17(7):1696–701. https://doi.org/10.1158/1055-9965.EPI-07-2752.
Conroy SM, Butler LM, Harvey D, Gold EB, Sternfeld B, Oestreicher N, et al. Physical activity and change in mammographic density: the Study of Women’s Health Across the Nation. Am J Epidemiol. 2010;171(9):960–8. https://doi.org/10.1093/aje/kwq025.
Woolcott CG, Courneya KS, Boyd NF, Yaffe MJ, Terry T, McTiernan A, et al. Mammographic density change with 1 year of aerobic exercise among postmenopausal women: a randomized controlled trial. Cancer Epidemiol Biomark Prev. 2010;19(4):1112–21. https://doi.org/10.1158/1055-9965.EPI-09-0801.
Martin LJ, Li Q, Melnichouk O, Greenberg C, Minkin S, Hislop G, et al. A randomized trial of dietary intervention for breast cancer prevention. Cancer Res. 2011;71(1):123–33. https://doi.org/10.1158/0008-5472.CAN-10-1436.
•• Cuzick J, Warwick J, Pinney E, Duffy SW, Cawthorn S, Howell A, et al. Tamoxifen-induced reduction in mammographic density and breast cancer risk reduction: a nested case-control study. J Natl Cancer Inst. 2011;103(9):744–52. https://doi.org/10.1093/jnci/djr079. Demonstration that mammographic density declines in response to tamoxifen.
•• McCormack VA, dos Santos Silva I. Breast density and parenchymal patterns as markers of breast cancer risk: a meta-analysis. Cancer Epidemiol Biomark Prev. 2006;15(6):1159–69. https://doi.org/10.1158/1055-9965.EPI-06-0034. Analysis of breast density and parenchymal pattering as risk markers.
Egan RL, Mosteller RC. Breast cancer mammography patterns. Cancer. 2006;40(5):2087–90.
•• Boyd NF, Guo H, Martin LJ, Sun L, Stone J, Fishell E, et al. Mammographic density and the risk and detection of breast cancer. N Engl J Med. 2007;356(3):227–36. https://doi.org/10.1056/NEJMoa062790. Evidence of a masking effect from high density.
Chen Z, Wu AH, Gauderman WJ, Bernstein L, Ma H, Pike MC, et al. Does mammographic density reflect ethnic differences in breast cancer incidence rates? Am J Epidemiol. 2004;159(2):140–7.
Razzaghi H, Troester MA, Gierach GL, Olshan AF, Yankaskas BC, Millikan RC. Mammographic density and breast cancer risk in White and African American women. Breast Cancer Res Treat. 2012;135(2):571–80. https://doi.org/10.1007/s10549-012-2185-3.
Johns PC, Yaffe MJ. X-ray characterisation of normal and neoplastic breast tissues. Phys Med Biol. 1987;32(6):675–95.
Pollán M, Lope V, Miranda-García J, García M, Casanova F, Sánchez-Contador C, et al. Adult weight gain, fat distribution and mammographic density in Spanish pre-and post-menopausal women (DDM-Spain). Breast Cancer Res Treat. 2012;1–16.
Couto E, Qureshi SA, Hofvind S, Hilsen M, Aase H, Skaane P, et al. Hormone therapy use and mammographic density in postmenopausal Norwegian women. Breast Cancer Res Treat. 2012;132(1):297–305. https://doi.org/10.1007/s10549-011-1810-x.
Lope V, Pérez-Gómez B, Sánchez-Contador C, Santamariña MC, Moreo P, Vidal C, et al. Obstetric history and mammographic density: a population-based cross-sectional study in Spain (DDM-Spain). Breast Cancer Res Treat. 2012;1–10.
Boyd NF, Martin LJ, Stone J, Greenberg C, Minkin S, Yaffe MJ. Mammographic densities as a marker of human breast cancer risk and their use in chemoprevention. Curr Oncol Rep. 2001;3(4):314–21.
Conklin MW, Eickhoff JC, Riching KM, Pehlke CA, Eliceiri KW, Provenzano PP, et al. Aligned collagen is a prognostic signature for survival in human breast carcinoma. Am J Pathol. 2011;178(3):1221–32. https://doi.org/10.1016/j.ajpath.2010.11.076.
Riching KM, Cox BL, Salick MR, Pehlke C, Riching AS, Ponik SM, et al. 3D collagen alignment limits protrusions to enhance breast cancer cell persistence. Biophys J. 2014;107(11):2546–58. https://doi.org/10.1016/j.bpj.2014.10.035.
Arendt LM, Rudnick JA, Keller PJ, Kuperwasser C. Stroma in breast development and disease. Semin Cell Dev Biol. 2010;21(1):11–8. https://doi.org/10.1016/j.semcdb.2009.10.003.
Tamimi SO, Ahmed A. Stromal changes in invasive breast carcinoma: an ultrastructural study. J Pathol. 1987;153(2):163–70. https://doi.org/10.1002/path.1711530209.
Sahai E, Wyckoff J, Philippar U, Segall JE, Gertler F, Condeelis J. Simultaneous imaging of GFP, CFP and collagen in tumors in vivo using multiphoton microscopy. BMC Biotechnol. 2005;5:14. https://doi.org/10.1186/1472-6750-5-14.
Goswami S, Sahai E, Wyckoff JB, Cammer M, Cox D, Pixley FJ, et al. Macrophages promote the invasion of breast carcinoma cells via a colony-stimulating factor-1/epidermal growth factor paracrine loop. Cancer Res. 2005;65(12):5278–83. https://doi.org/10.1158/0008-5472.CAN-04-1853.
Wolf K, Mazo I, Leung H, Engelke K, von Andrian UH, Deryugina EI, et al. Compensation mechanism in tumor cell migration: mesenchymal-amoeboid transition after blocking of pericellular proteolysis. J Cell Biol. 2003;160(2):267–77. https://doi.org/10.1083/jcb.200209006.
Provenzano PP, Eliceiri KW, Campbell JM, Inman DR, White JG, Keely PJ. Collagen reorganization at the tumor-stromal interface facilitates local invasion. BMC Med. 2006;4(1):38. https://doi.org/10.1186/1741-7015-4-38.
Provenzano PP, Inman DR, Eliceiri KW, Knittel JG, Yan L, Rueden CT, et al. Collagen density promotes mammary tumor initiation and progression. BMC Med. 2008;6:11. https://doi.org/10.1186/1741-7015-6-11.
Maglione JE, Moghanaki D, Young LJ, Manner CK, Ellies LG, Joseph SO, et al. Transgenic Polyoma middle-T mice model premalignant mammary disease. Cancer Res. 2001;61(22):8298–305.
Lin EY, Jones JG, Li P, Zhu L, Whitney KD, Muller WJ, et al. Progression to malignancy in the polyoma middle T oncoprotein mouse breast cancer model provides a reliable model for human diseases. Am J Pathol. 2003;163(5):2113–26. https://doi.org/10.1016/S0002-9440(10)63568-7.
Wyckoff JB, Wang Y, Lin EY, Li JF, Goswami S, Stanley ER, et al. Direct visualization of macrophage-assisted tumor cell intravasation in mammary tumors. Cancer Res. 2007;67(6):2649–56. https://doi.org/10.1158/0008-5472.CAN-06-1823.
Wang W, Wyckoff JB, Frohlich VC, Oleynikov Y, Huttelmaier S, Zavadil J, et al. Single cell behavior in metastatic primary mammary tumors correlated with gene expression patterns revealed by molecular profiling. Cancer Res. 2002;62(21):6278–88.
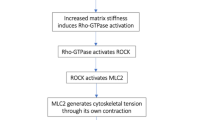
•• Provenzano PP, Inman DR, Eliceiri KW, Trier SM, Keely PJ. Contact guidance mediated three-dimensional cell migration is regulated by Rho/ROCK-dependent matrix reorganization. Biophys J. 2008;95(11):5374–84. https://doi.org/10.1529/biophysj.108.133116. Study demonstrating linkage between contact, migration, and signaling.
Campagnola PJ, Loew LM. Second-harmonic imaging microscopy for visualizing biomolecular arrays in cells, tissues and organisms. Nat Biotechnol. 2003;21(11):1356–60. https://doi.org/10.1038/nbt894.
Raub CB, Unruh J, Suresh V, Krasieva T, Lindmo T, Gratton E, et al. Image correlation spectroscopy of multiphoton images correlates with collagen mechanical properties. Biophys J. 2008;94(6):2361–73. https://doi.org/10.1529/biophysj.107.120006.
Reiser KM, Bratton C, Yankelevich DR, Knoesen A, Rocha-Mendoza I, Lotz J. Quantitative analysis of structural disorder in intervertebral disks using second harmonic generation imaging: comparison with morphometric analysis. J Biomed Opt. 2007;12(6):064019. https://doi.org/10.1117/1.2812631.
Erikson A, Ortegren J, Hompland T, de Lange Davies C, Lindgren M. Quantification of the second-order nonlinear susceptibility of collagen I using a laser scanning microscope. J Biomed Opt. 2007;12(4):044002. https://doi.org/10.1117/1.2772311.
Kirkpatrick ND, Brewer MA, Utzinger U. Endogenous optical biomarkers of ovarian cancer evaluated with multiphoton microscopy. Cancer Epidemiol Biomark Prev. 2007;16(10):2048–57. https://doi.org/10.1158/1055-9965.EPI-07-0009.
Schenke-Layland K, Stock UA, Nsair A, Xie J, Angelis E, Fonseca CG, et al. Cardiomyopathy is associated with structural remodelling of heart valve extracellular matrix. Eur Heart J. 2009;30(18):2254–65. https://doi.org/10.1093/eurheartj/ehp267.
Lacomb R, Nadiarnykh O, Campagnola PJ. Quantitative second harmonic generation imaging of the diseased state osteogenesis imperfecta: experiment and simulation. Biophys J. 2008;94(11):4504–14. https://doi.org/10.1529/biophysj.107.114405.
Hompland T, Erikson A, Lindgren M, Lindmo T, de Lange Davies C. Second-harmonic generation in collagen as a potential cancer diagnostic parameter. J Biomed Opt. 2008;13(5):054050. https://doi.org/10.1117/1.2983664.
•• Conklin MW, Gangnon RE, Sprague BL, Van Gemert L, Hampton JM, Eliceiri KW, et al. Collagen alignment as a predictor of recurrence after ductal carcinoma in situ. Cancer Epidemiol Biomark Prev. 2018;27(2):138–45. https://doi.org/10.1158/1055-9965.EPI-17-0720. Study of collagen alignment as a predictor of DCIS recurrence.
McConnell JC, O’Connell OV, Brennan K, Weiping L, Howe M, Joseph L, et al. Increased peri-ductal collagen micro-organization may contribute to raised mammographic density. Breast Cancer Res. 2016;18(1):5. https://doi.org/10.1186/s13058-015-0664-2.
Butcher DT, Alliston T, Weaver VM. A tense situation: forcing tumour progression. Nat Rev Cancer. 2009;9(2):108–22. https://doi.org/10.1038/nrc2544.
Paszek MJ, Zahir N, Johnson KR, Lakins JN, Rozenberg GI, Gefen A, et al. Tensional homeostasis and the malignant phenotype. Cancer Cell. 2005;8(3):241–54. https://doi.org/10.1016/j.ccr.2005.08.010.
Galbraith CG, Yamada KM, Sheetz MP. The relationship between force and focal complex development. J Cell Biol. 2002;159(4):695–705. https://doi.org/10.1083/jcb.200204153.
Giancotti FG, Ruoslahti E. Integrin signaling. Science. 1999;285(5430):1028–32.
Riveline D, Zamir E, Balaban NQ, Schwarz US, Ishizaki T, Narumiya S, et al. Focal contacts as mechanosensors: externally applied local mechanical force induces growth of focal contacts by an mDia1-dependent and ROCK-independent mechanism. J Cell Biol. 2001;153(6):1175–86.
Tzima E, del Pozo MA, Shattil SJ, Chien S, Schwartz MA. Activation of integrins in endothelial cells by fluid shear stress mediates Rho-dependent cytoskeletal alignment. EMBO J. 2001;20(17):4639–47. https://doi.org/10.1093/emboj/20.17.4639.
Northcott JM, Dean IS, Mouw JK, Weaver VM. Feeling stress: the mechanics of cancer progression and aggression. Front Cell Dev Biol. 2018;6:17. https://doi.org/10.3389/fcell.2018.00017.
Wozniak MA, Modzelewska K, Kwong L, Keely PJ. Focal adhesion regulation of cell behavior. Biochim Biophys Acta. 2004;1692(2–3):103–19. https://doi.org/10.1016/j.bbamcr.2004.04.007.
Shi Q, Boettiger D. A novel mode for integrin-mediated signaling: tethering is required for phosphorylation of FAK Y397. Mol Biol Cell. 2003;14(10):4306–15. https://doi.org/10.1091/mbc.e03-01-0046.
•• Provenzano PP, Inman DR, Eliceiri KW, Keely PJ. Matrix density-induced mechanoregulation of breast cell phenotype, signaling and gene expression through a FAK-ERK linkage. Oncogene. 2009;28(49):4326–43. https://doi.org/10.1038/onc.2009.299. Demonstration that mechanical signaling promotes FAK-signaling.
Yu H, Mouw JK, Weaver VM. Forcing form and function: biomechanical regulation of tumor evolution. Trends Cell Biol. 2011;21(1):47–56. https://doi.org/10.1016/j.tcb.2010.08.015.
Provenzano PP, Keely PJ. Mechanical signaling through the cytoskeleton regulates cell proliferation by coordinated focal adhesion and Rho GTPase signaling. J Cell Sci. 2011;124(Pt 8):1195–205. https://doi.org/10.1242/jcs.067009.
Sun HW, Tong SL, He J, Wang Q, Zou L, Ma SJ, et al. RhoA and RhoC -siRNA inhibit the proliferation and invasiveness activity of human gastric carcinoma by Rho/PI3K/Akt pathway. World J Gastroenterol. 2007;13(25):3517–22.
Dupont S, Morsut L, Aragona M, Enzo E, Giulitti S, Cordenonsi M, et al. Role of YAP/TAZ in mechanotransduction. Nature. 2011;474(7350):179–83. https://doi.org/10.1038/nature10137.
Du J, Zu Y, Li J, Du S, Xu Y, Zhang L, et al. Extracellular matrix stiffness dictates Wnt expression through integrin pathway. Sci Rep. 2016;6:20395. https://doi.org/10.1038/srep20395.
Irianto J, Pfeifer CR, Ivanovska IL, Swift J, Discher DE. Nuclear lamins in cancer. Cell Mol Bioeng. 2016;9(2):258–67. https://doi.org/10.1007/s12195-016-0437-8.
Osmanagic-Myers S, Dechat T, Foisner R. Lamins at the crossroads of mechanosignaling. Genes Dev. 2015;29(3):225–37. https://doi.org/10.1101/gad.255968.114.
Swift J, Ivanovska IL, Buxboim A, Harada T, Dingal PC, Pinter J, et al. Nuclear lamin-A scales with tissue stiffness and enhances matrix-directed differentiation. Science. 2013;341(6149):1240104. https://doi.org/10.1126/science.1240104.
Vartiainen MK, Guettler S, Larijani B, Treisman R. Nuclear actin regulates dynamic subcellular localization and activity of the SRF cofactor MAL. Science. 2007;316(5832):1749–52. https://doi.org/10.1126/science.1141084.
Ho CY, Jaalouk DE, Vartiainen MK, Lammerding J. Lamin A/C and emerin regulate MKL1-SRF activity by modulating actin dynamics. Nature. 2013;497(7450):507–11. https://doi.org/10.1038/nature12105.
Funding
This work was financially supported by the National Institutes of Health/National Cancer Institute (NIH/NCI) grants R01CA155664, R01CA158668, R01CA170851, R01CA192914, and U01CA189283 (all to VLS) and P30CA033572.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Disclaimer
The funders had no role in the manuscript design, data analysis, decision to publish, or preparation of the manuscript.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Katherine Tossas-Milligan and Sundus Shalabi are co-first authors.
This article is part of the Topical Collection on Risk and Prevention
Rights and permissions
About this article
Cite this article
Tossas-Milligan, K., Shalabi, S., Jones, V. et al. Mammographic Density: Intersection of Advocacy, Science, and Clinical Practice. Curr Breast Cancer Rep 11, 100–110 (2019). https://doi.org/10.1007/s12609-019-00316-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12609-019-00316-4