Abstract
Purpose of the review
Numerous strategies and technologies have been historically used, with new ones being rapidly introduced, to maximize the chance of obtaining clear margins at the first lumpectomy. The goal of this review was to summarize the data on each, illustrate their strengths and weaknesses, and equip the surgeon to determine which best fits into their center or practice.
Recent Findings
There is no technology or device currently that always results in negative margins. Many of the studies reviewed (including frozen sections, shave margins, specimen radiography, intraoperative ultrasound, imprint cytology, and new devices) show excellent negative margin rates, but many of the comparison studies have conflicting results and reasons for this are discussed. Newer emerging technologies hold great promise but there is a tendency to overinflate positive results.
Summary
It is important for surgeons to review their own re-excision rates to determine the need for further technology and strategies. Most of the investigative technologies are still years away from widespread acceptance.


Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Morrow M. Surgeon recommendations and receipt of mastectomy for treatment of breast cancer. JAMA. 2009;302(14):1551–6.
McCahill L, Single R, Aiello Bowles E, et al. Variability in Reexcision following breast conservation surgery. JAMA. 2012;307(5):467–75.
•• Moran M, Schnitt S, Giuliano A, Harris JR, Khan SA, Horton J, et al. Society of Surgical Oncology-American Society for Radiation Oncology consensus guideline on margins for breast-conserving surgery with whole-breast irradiation in stages I and II invasive breast cancer. J Clin Oncol. 2014;32(14):1507–15. This landmark paper established no ink on tumor as an acceptable standard.
• Morrow M, Van Zee K, Solin L, et al. Society of Surgical Oncology-American Society for Radiation Oncology-American Society of Clinical Oncology consensus guideline on margins for breast-conserving surgery with whole-breast irradiation in ductal carcinoma in situ. Pract Radiat Oncol. 2016;6(5):287–95. References 3 and 4 established a consensus on management of margins.
Rosenberger L, Mamtani A, Fuzesi S, et al. Early adoption of the SSO-ASTRO consensus guidelines on margins for breast-conserving surgery with whole-breast irradiation in stage I and II invasive breast cancer: initial experience from Memorial Sloan Kettering Cancer Center. Ann Surg Oncol. 2016;23(10):3239–46.
Kurniawan E, Wong M, Windle I, et al. Predictors of surgical margin status in breast-conserving surgery within a breast screening program. Ann Surg Oncol. 2008;15:2542–9.
Smitt M, Horst K. Association of clinical and pathologic variables with lumpectomy surgical margin status after preoperative diagnosis or excisional biopsy of invasive breast cancer. Ann Surg Oncol. 2007;14:1040–4.
Houssami N, Macaskill P, Luke Marinovich M, Morrow M. The association of surgical margins and local recurrence in women with early-stage invasive breast cancer treated with breast-conserving therapy: a meta-analysis. Ann Surg Oncol. 2014;21(3):717–30.
Uematsu T, Yuen S, KasamiM Yuen S, Kasami M, Uchida Y Comparison of magnetic resonance imaging, multidetector row computed tomography, ultrasonography, and mammography for tumor extension of breast cancer. Breast Cancer Res Treat 2008;112:461–474.
Vanderwalde L, Dang CM, Bresee C, Phillips EH. Discordance between pathologic and radiologic tumor size on breast MRI may contribute to increased re-excision rates. Am Surg. 2011;77(10):1361–3.
McGhan L, Wasif N, Gray R, et al. Use of preoperative magnetic resonance imaging for invasive lobular cancer: good, better, but maybe not the best? Ann Surg Oncol. 2010;17(S3):255–62.
Mann R, Hoogeveen Y, Blickman J, Boetes C. MRI compared to conventional diagnostic work-up in the detection and evaluation of invasive lobular carcinoma of the breast: a review of existing literature. Breast Cancer Res Treat. 2008;107(1):1–14.
Vos E, Voogd A, Verhoef C, et al. Benefits of preoperative MRI in breast cancer surgery studied in a large population-based cancer registry. Br J Surg. 2015;102(13):1649–57.
Lai H, Chen C, Lin Y, et al. Does breast magnetic resonance imaging combined with conventional imaging modalities decrease the rates of surgical margin involvement and reoperation? Medicine. 2016;95(22):e3810.
Sung J, Li J, Costa G, et al. Preoperative breast MRI for early-stage breast cancer: effect on surgical and long-term outcomes. Am J Roent. 2014;202(6):1376–82.
Houssami N, Turner R, Morrow M. Preoperative magnetic resonance imaging in breast cancer: meta-analysis of surgical outcomes. Ann Surg. 2013;257:249–55.
Hwang N, Schiller D, Crystal P, et al. Magnetic resonance imaging in the planning of initial lumpectomy for invasive breast carcinoma: its effect on ipsilateral breast tumor recurrence after breast-conservation therapy. Ann Surg Oncol. 2009;16(11):3000–9.
Davis K, Barth R, Gui J, et al. Use of MRI in preoperative planning for women with newly diagnosed DCIS: risk or benefit? Ann Surg Oncol. 2012;19(10):3270–4.
Fancellu A, Soro D, Castiglia P, Marras V, Melis M, Cottu P, et al. Usefulness of magnetic resonance in patients with invasive cancer eligible for breast conservation: a comparative study. Clin Breast Cancer. 2014;14(2):114–21.
Bleicher R, Ciocca R, Egleston B, et al. Association of routine pretreatment magnetic resonance imaging with time to surgery, mastectomy rate, and margin status. J Am Coll Surg. 2009;209(2):180–7.
Turnbull L, Brown S, Harvey I, Olivier C, Drew P, Napp V, et al. Comparative effectiveness of MRI in breast cancer (COMICE) trial: a randomized controlled trial. Lancet. 2010;375(9714):563–71.
Peters N, van Esser S, van den Bosch M, et al. Preoperative MRI and surgical management in patients with nonpalpable breast cancer: the MONET-randomised controlled trial. Eur J Cancer. 2011;47(6):879–86.
De Felice C, Cipolla V, Stagnitti A, et al. The impact of presurgical magnetic resonance in early breast cancer: an observational study. Eur J Gynaecol Oncol. 2012;33(2):193–9.
Grobmyer S, Mortellaro V, Marshall J, et al. Is there a role for routine use of MRI in selection of patients for breast-conserving cancer therapy? J Am Coll Surg. 2008;206(5):1045–50; discussion 1050-2.
Bilimoria K, Cambic A, Hansen N, Bethke KP. Evaluating the impact of preoperative breast magnetic resonance imaging on the surgical management of newly diagnosed breast cancers. Arch Surg. 2007;142(5):441.
• National Comprehensive Cancer Network 2017 NCCN guidelines for breast cancer screening and diagnosis. https://www.nccn.org/professionals/physician_gls/pdf/breast-screening.pdf. Accessed 25 January 2018. This established national guidelines for MRI.
Clough K, Kaufman G, Nos C, et al. Reply to comments on: improving breast cancer surgery: a classification and quadrant per quadrant atlas for oncoplastic surgery. Ann Surg Oncol. 2010;17(5):1375–91.
Fitoussi A, Berry M, Famà F, et al. Oncoplastic breast surgery for cancer: analysis of 540 consecutive cases. Plast Reconstr Surg. 2010;125(2):454–62.
Clough K, Ihrai T, Oden S, et al. Oncoplastic surgery for breast cancer based on tumour location and a quadrant-per-quadrant atlas. Br J Surg. 2012;99(10):1389–95.
Haloua M, Krekel N, Winters H, et al. A systematic review of oncoplastic breast-conserving surgery. Ann Surg. 2013;257(4):609–20.
Jeevan R, Cromwell D, Trivella M, et al. Reoperation rates after breast conserving surgery for breast cancer among women in England: retrospective study of hospital episode statistics. BMJ. 2012;345(122):e4505-e4505.
Silverstein M, Savalia N, Khan S, et al. Extreme oncoplasty: breast conservation for patients who need mastectomy. Breast J. 2015;21(1):52–9.
Campbell E, Romics L. Oncological safety and cosmetic outcomes in oncoplastic breast conservation surgery, a review of the best level of evidence literature. Breast Cancer: Targets Ther. 2017;9:521–30.
Losken A, Dugal C, Styblo T, et al. A meta-analysis comparing breast conservation therapy alone to the oncoplastic technique. Ann Plas Surg. 2014;72(2):145–9.
Clough K, van la Parra R, Thygesen H, et al. Long-term results after oncoplastic surgery for breast cancer: a 10-year follow-up. Ann Surg 2017: Apr 26. [Epub ahead of print], 1.
Yoon J, Green W, Kim S, et al. Oncoplastic breast surgery in the setting of breast-conserving therapy: a systematic review. Adv Radiat Oncol. 2016;1(4):205–15.
Shah C, Vicini F, Shaitelman S, et al. The American Brachytherapy Society consensus statement for accelerated partial-breast irradiation. Brachytherapy. 2017. S1538–4721(17)30462–30462.
Cross M, Lebovic G, Stubbs J, Ross J, Jones S, Beck T. Identifying the surgical cavity following oncoplastic breast surgery. J Clin Oncol. 2014;32(26 suppl):81–1.
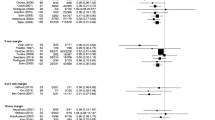
•• St John E, Al-Khudairi R, Ashrafian H, et al. Diagnostic accuracy of intraoperative techniques for margin assessment in breast cancer surgery: a meta-analysis. Ann Surg. 2017;265(2):300–10. Landmark article on how to assess new technology that looks at detecting disease at the margin of breast cancers
• Gray R, Pockaj B, Garvey E, Blair S. Intraoperative margin management in breast-conserving surgery: a systematic review of the literature. Ann Surg Oncol. 2017;25(1):18–27. A recent review of standardly used techniques to evaluate margins on lumpectomy specimens
Chagpar AB, Killelea BK, Tsangaris TN, Butler M, Stavris K, Li F, et al. A randomized controlled trial of cavity shave margins in breast cancer. N Engl J Med. 2015;373(6):503–10.
Janes S, Stankhe M, Singh S, et al. Systematic cavity shaves reduces close margins and re-excision rates in breast conserving surgery. Breast. 2006;15(3):326–30.
Huston TL, Pigalarga M, Osborne MP, et al. The influence of additional surgical margins on the total specimen volume excised and the reoperative rate after breast-conserving surgery. Am J Surg. 2006;192(4):509–12.
Fizzy M, Iyengar R, Gabram S. The effects of additional tumor cavity sampling at the time of breast-conserving surgery on final margin status, volume of resection, and pathologist workload. Ann Surg Oncol. 2010;17(1):228–34.
Héquet D, Bricou A, Koual M, Ziol M, Feron JG, Rouzier R, et al. Systematic cavity shaving: modifications of breast cancer management and long-term local recurrence, a multicentre study. Eur J Surg Oncol (EJSO). 2013;39(8):899–905.
Malik H, George W, Mallon E, et al. Margin assessment by cavity shaving after breast-conserving surgery: analysis and follow-up of 543 patients. Eur J Surg Oncol (EJSO). 1999;25(5):464–9.
Schwartz G, Goldberg B, Rifkin M, D’Orazio SE. Ultrasonography: an alternative to X-ray guided needle localization of non-palpable breast masses. Surgery. 1988;104:870–3.
Harlow S, Krag D, Ames S, et al. Intraoperative ultrasound localization to guide surgical excision of nonpalpable breast carcinoma. J Am Coll Surg. 1999;189(3):241–6.
Kaufman C, Jacobson L, Bachman B, et al. Intraoperative ultrasound facilitates surgery for early breast cancer. Ann Surg Oncol. 2002;9(10):988–93.
Hargreaves A, Mohamed M, Audisio R. Intra-operative guidance: methods for achieving negative margins in breast conserving surgery. J Surg Oncol. 2014;110(1):21–5.
Tummel E, Betzold R, Gallagher K, Klimberg VS. The CUBE technique: continuous ultrasound-guided breast excision. Ann Surg Oncol. 2014;21(10):3354–5.
Tan K, Tan S, Chiang S, et al. Breast specimen ultrasound and mammography in the prediction of tumour free margins. Anns J Surg. 2006;76(12):1064–7.
Olsha O, Shemesh D, Carmon M, Sibirsky O, Abu Dalo R, Rivkin L, et al. Resection margins in ultrasound-guided breast-conserving surgery. Ann Surg Oncol. 2010;18(2):447–52.
Ignatov A, Ignatov T, Costa S, et al. Accuracy of ultrasound-guided breast-conserving surgery in the determination of adequate surgical margins. Breast Cancer Res Treat. 2014;145(01):129–36.
Krekel N, Haloua M, Lopes Cardozo A, et al. Intraoperative ultrasound guidance for palpable breast cancer excision (COBALT trial): a multicentre, randomised controlled trial. Lancet Oncol. 2013;14(1):48–54.
Rahusen F, Bremers A, Fabry H, et al. Ultrasound-guided lumpectomy of nonpalpable breast cancer versus wire-guided resection: a randomized clinical trial. Ann Surg Oncol. 2002;9(10):994–8.
Barentsz M, van Dalen T, Gobardhan P, et al. Intraoperative ultrasound guidance for excision of non-palpable invasive breast cancer: a hospital based series and an overview of the literature. Breast Cancer Res Treat. 2012;135:209–19.
• Landercasper J, Attai D, Atisha D, Beitsch P, Bosserman L, Boughey J, et al. Toolbox to reduce lumpectomy reoperations and improve cosmetic outcome in breast cancer patients: the American Society of Breast Surgeons Consensus Conference. Ann Surg Oncol. 2015;22(10):3174–83. A review of how to maximize negative margins
Sajid M, Parampalli U, Haider Z, Bonomi R. Comparison of radioguided occult lesion localization (ROLL) and wire localization for non-palpable breast cancers: a meta-analysis. J Surg Oncol. 2011;105(8):852–8.
Chadwick D, Shorthouse A. Wire-directed localization biopsy of the breast: an audit of results and analysis of factors influencing therapeutic value in the treatment of breast cancer. Eur J Surg Oncol. 1997;23(2):128–33.
Giacalone P, Bourdon A, Trinh P, et al. Radioguided occult lesion localization plus sentinel node biopsy (SNOLL) versus wire-guided localization plus sentinel node detection: a case control study of 129 unifocal pure invasive non-palpable breast cancers. Eur J Surg Oncol. 2012;23(2):128–33.
Kim S, Cornacch S, Heller B, et al. An evaluation of intraoperative digital specimen mammography versus conventional specimen radiography for the excision of nonpalpable breast lesions. Am J Surg. 2013;205(6):703–10.
McCormick J, Keleher A, Tikhomirov V, et al. Analysis of the use of specimen mammography in breast conservation therapy. Am J Surg. 2004;188(4):433–6.
Ihrai T, Quaranta D, Fouche Y, Machiavello JC, Raoust I, Chapellier C, et al. Intraoperative radiological margin assessment in breast-conserving surgery. Eur J Surg Oncol. 2014;40(4):449–53.
Muttalib M, Tisdall M, Scawn R, Shousha S, Cummins RS, Sinnett HD. Intra-operative specimen analysis using faxitron microradiography for excision of mammographically suspicious, non-palpable breast lesions. Breast. 2004;13(4):307–15.
Bathla L, Harris A, Davey M, Sharma P, Silva E. High resolution intra-operative two-dimensional specimen mammography and its impact on second operation for re-excision of positive margins at final pathology after breast conservation surgery. Am J Surg. 2011;202(4):387–94.
Weber W, Engelberger S, Viehl C, et al. Accuracy of frozen section analysis versus specimen radiography during breast-conserving surgery for nonpalpable lesions. World J Surg. 2008;32(12):2599–606.
Esbona K, Li Z, Wilke L. Intraoperative imprint cytology and frozen section pathology for margin assessment in breast conservation surgery: a systematic review. Ann Surg Oncol. 2012;19:3236–45.
Rusby J, Paramanathan N, Laws S, et al. Immediate latisimuss dorsi mini flap volume replacement for partial mastectomy: use of intra-operative frozen sections to confirm negative margins. Am J Surg. 2008;196(4):512–8.
Caruso F, Ferrara M, Castiglione G, Cannata I, Marziani A, Polino C, et al. Therapeutic mammaplasties: full local control of breast cancer in one surgical stage with frozen sections. Eur J Surg Oncol. 2011;37:871–5.
Jorns J, Daignault S, Sabel M, et al. Frozen sections in patients undergoing breast conserving surgery at a single ambulatory surgical center: 5 year experience. Eur J Surg Oncol. 2017;43(7):1273–81.
Osako T, Nishimura R, Nishiyama Y, Okumura Y, Tashima R, Nakano M, et al. Efficacy of intraoperative entire-circumferential frozen section analysis of lumpectomy margins during breast-conserving surgery for breast cancer. Int J Clin Oncol. 2015;20(6):1093–101.
Boughey JC, Keeney GL, Radensky P, Song CP, Habermann EB. Economic implications of widespread expansion of frozen section margin analysis to guide surgical resection in women with breast cancer undergoing breast-conserving surgery. J Oncol Pract. 2016;12(4):e413–22.
Cendán J, Coco D, Copeland EM 3rd. Accuracy of intraoperative frozen-section analysis of breast cancer lumpectomy-bed margins. J Am Coll Surg. 2005;201(2):194–8.
Olson TP, Harter J, Munoz A, et al. Frozen section analysis for intraoperative margin assessment during breast-conserving surgery results in low rates of re-excision and local recurrence. Ann Surg Oncol. 2007;14:2953–60.
Cabioglu N, Hunt KK, Sahin A, et al. Role for intraoperative margin assessment in patients undergoing breast-conserving surgery. Ann Surg Oncol. 2007;14:1458–71.
Reidl O, Fitzal F, Mader N, et al. Intraoperative frozen section analysis for breast-conserving therapy in 1016 patients with breast cancer. Eur J Surg Oncol. 2009;35:264–70.
D’Halluin F, Tas P, Rouquette S, Bendavid C, Foucher F, Meshba H, et al. Intra-operative touch preparation cytology following lumpectomy for breast cancer: a series of 400 procedures. Breast. 2009;18(4):248–53.
Cox C, Ku N, Reintgen DS, Greenberg HM, Nicosia SV, Wangensteen S. Touch preparation cytology of breast lumpectomy margins with histologic correlation. Arch Surg. 1991;126:490–3.
Cortes-Mateos M, Martin D, Sandoval S, et al. Automated microscopy to evaluate surgical specimens via touch prep in breast cancer. Ann Surg Oncol. 2009;16(3):709–20.
• Wang Y, Reder N, Kang S, et al. Raman-encoded molecular imaging with topically applied SERS nanoparticles for intraoperative guidance of lumpectomy. Canc Res. 2017;77(16):4506–16. Innovative new technology to look at tumor biology at the margin
• Dixon J, Renshaw L, Keys J, et al. Intra-operative assessment of excision margins in breast conserving surgery for breast cancer using ClearEdge imaging device. Eur J Surg Oncol. 2015:41:S54. Advanced technology that could be practically used in the operating room.
St John E, Al-Khudairi R, Balog J, et al. Rapid evaporative ionization mass spectrometry towards real time intraoperative oncological margin status determination in breast conserving surgery. Cancer Res 2016:76(4 suppl):P2-12-20.
Erickson-Bhatt S, Nolan R, Shemonski N, et al. Real-time imaging of the resection bed using a handheld probe to reduce incidence of microscopic positive margins in cancer surgery. Cancer Res. 2015;75(18):3706–12.
Zysk A, Chen K, Gabrielson E, et al. Intraoperative assessment of final margins with a handheld optical imaging probe during breast-conserving surgery may reduce the reoperation rate: results of a multicenter study. Ann Surg Oncol. 2015;22(10):3356–62.
Chang T, Leff D, Shousha S, et al. Imaging breast cancer morphology using probe-based confocal laser endomicroscopy: towards a real-time intraoperative imaging tool for cavity scanning. Breast Cancer Res Treat. 2015;153:299–310.
Whitley M, Cardona D, Lazarides A, et al. A mouse-human phase 1 co-clinical trial of a protease-activated fluorescent probe for imaging cancer. Sci Transl Med. 2016;8(320):320ra4.
Tang R, Coopey S, Buckley J, Aftreth OP, Fernandez LJ, Brachtel EF, et al. A pilot study evaluating shaved cavity margins with micro-computed tomography: a novel method for predicting lumpectomy margin status intraoperative. Breast J. 2013;19:485–9.
Omer R, Soensen K, Neumayer L, et al. High-frequency ultrasound for evaluating margins during breast conservation surgery: results from a 17-patient pilot study. J Acoustic Sock Am. 2015;138:1746.
Moshe P, Allweis T, Karni T, et al. An intraoperative MRI system for margin assessment in breast conserving surgery: initial results from a novel technique. J Surg Onc. 2016;114:22–6.
Grootendorst M, Cariati M, Pinder S, et al. Intraoperative assessment of tumor resection margins in breast-conserving surgery using 18F-FDG cerenkov luminescence imaging: a first-in-human feasibility study. J Nucl Med. 2017;58:891–8.
Coble J, Reid V. Achieving clear margins. Directed shaving using MarginProbe, as compared to a full cavity shave approach. Amer J Surg. 2017;213:627–30.
Blohmer J, Tanko J, Keuper J, et al. MarginProbe reduces the rate of re-excision following breast conserving surgery for breast cancer. Arch Gynecol Obstet. 2016;294:361–7.
• Schnabel F, Boolbol S, Gittleman M, et al. A randomized prospective study of lumpectomy margin assessment with use of MarginProbe in patients with nonpalpable breast malignancies. Ann Surg Oncol 2014;21:1589-95. This showed that the take back rate did not change significantly.
Allweis T, Kaufman Z, Lelcuk S, et al. A prospective, randomized, controlled multi-center study of real-time intraoperative probe for positive margin detection in breast-conserving surgery. Am J Surg. 2008;196:483–9.
Klein J, Kong I, Paszat L, Nofech-Mozes S, Hanna W, Thiruchelvam D, et al. Close or positive resection margins are not associated with an increased risk of chest wall recurrence in women with DCIS treated by mastectomy: a population-based analysis. Spring. 2015;4:335.
Al-Himdani S, Timbrell S, Tan K, et al. Prediction of margin involvement and local recurrence after skin-sparing and simple mastectomy. Eur J Surg Oncol. 2016;42(7):935–41.
Childs S, Chen Y, Duggan M, et al. Impact of margin status on local recurrence after mastectomy for ductal carcinoma in situ. Int J Radiat Oncol Biol Phys. 2013;85(4):948–52.
Acknowledgements
The authors thank Stephanie Parlacoski, BS, for clerical assistance.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no competing interests.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Local-Regional Evaluation and Therapy
Rights and permissions
About this article
Cite this article
Stelle, L., Wellington, J., Liang, W. et al. Local-Regional Evaluation and Therapy: Maximizing Margin-Negative Breast Cancer Resection Rates on the First Try. Curr Breast Cancer Rep 10, 110–121 (2018). https://doi.org/10.1007/s12609-018-0273-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12609-018-0273-z