Abstract
Objectives
In this study, we examined the factors influencing the presence or absence of dental intervention in patients with pneumonia in an acute-care hospital, focusing on oral intake and its status.
Design
Observational study.
Setting
Teikyo University School of Medicine, Mizonokuchi Hospital.
Participants
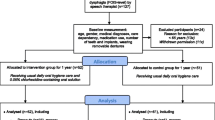
Patients ≥65 years of age who were admitted to the Teikyo University School of Medicine, Mizonokuchi Hospital between January 1, 2018 and December 31, 2019 with pneumonia who were referred to the Department of Rehabilitation with suspected dysphagia were included in the study. Fifty patients who underwent dental intervention were compared with 50 controls who had received no dental interventions prior to the opening of the dental department.
Measurements
Time series matching was retrospectively performed using the Oral Health Assessment Tool (OHAT). From the medical records, age at admission, sex, pneumonia severity classification (age, dehydration, respiratory failure, orientation disturbance, and blood pressure [A-DROP] score), body mass index, Charlson’s Comorbidity Index, OHAT, functional oral intake scale (FOIS) score at admission and discharge, and the length of hospital stay were retrieved; FOIS level ≥4 was defined as established oral intake.
Results
The number of patients in the control group before matching was 179. Twelve patients with missing information and seven patients who died in the hospital were excluded from this study. Multivariable logistic regression analysis showed that dental intervention (odds ratio 3.0, p = 0.014) was associated with the establishment of oral intake at discharge. Multiple logistic regression analysis showed that dental intervention was a significant factor for FOIS at discharge (p = 0.002) and the length of hospital stay (p = 0.039).
Conclusion
Oral management with dental intervention was associated with establishing oral intake and reducing hospital stay in patients with pneumonia, regardless of pneumonia severity or comorbidities.
Similar content being viewed by others
References
Furuya J, Suzuki H, Tamada Y, Onodera S, Nomura T, Hidaka R, Minakuchi S, Kondo H. Food intake and oral health status of inpatients with dysphagia in acute care settings. J Oral Rehabil 2020;47:736–742. doi: https://doi.org/10.1111/joor.12964
Rech RS, Baumgarten A, Colvara BC, Brochier CW, de Goulart B, Hugo FN, Hilgert JB. Association between oropharyngeal dysphagia, oral functionality, and oral sensorimotor alteration. Oral Dis 2018;24:664–672. doi: https://doi.org/10.1111/odi.12809
Yoshimi K, Nakagawa K, Hara K, Yamaguchi K, Nakane A, Kubota K, Furuya J, Tohara H. Relationship between tongue pressure and back muscle strength in healthy elderly individuals. Aging Clin Exp Res 2020;32:2549–2555. doi: https://doi.org/10.1007/s40520-020-01484-5
Komatsu R, Okazaki T, Ebihara S, Kobayashi M, Tsukita Y, Nihei M, Sugiura H, Niu K, Ebihara T, Ichinose M. Aspiration pneumonia induces muscle atrophy in the respiratory, skeletal, and swallowing systems. J Cachexia Sarcopenia Muscle 2018;9:643–653. doi: https://doi.org/10.1002/jcsm.12297
Ishimaru M, Matsui H, Ono S, Hagiwara Y, Morita K, Yasunaga H. Preoperative oral care and effect on postoperative complications after major cancer surgery. Br J Surg 2018;105:1688–1696. doi: https://doi.org/10.1002/bjs.10915
Shiraishi A, Yoshimura Y, Wakabayashi H, Tsuji Y, Yamaga M, Koga H. Hospital dental hygienist intervention improves activities of daily living, home discharge and mortality in post-acute rehabilitation. Geriatr Gerontol Int 2019;19:189–196.
Miyashita N, Matsushima T, Oka M, Japanese Respiratory Society. The JRS guidelines for the management of community-acquired pneumonia in adults: an update and new recommendations. Intern Med 2006;45:419–428. doi: https://doi.org/10.2169/internalmedicine.45.1691
Shindo Y, Sato S, Maruyama E, Ohashi T, Ogawa M, Imaizumi K. Comparison of severity scoring systems A-DROP and CURB-65 for community-acquired pneumonia. Respirology 2008;13:731–735. doi: https://doi.org/10.1111/j.1440-1843.2008.01329.x
Crary MA, Mann GD, Groher ME. Initial psychometric assessment of a functional oral intake scale for dysphagia in stroke patients. Arch Phys Med Rehabil 2005;86:1516–1520. doi: https://doi.org/10.1016/j.apmr.2004.11.049
Chalmers JM, King PL, Spencer AJ, Wright FA, Carter KD. The oral health assessment tool-validity and reliability. Aust Dent J 2005;50:191–199. doi: https://doi.org/10.1111/j.1834-7819.2005.tb00360.x
Austin PC. An introduction to propensity score methods for reducing the effects of confounding in observational studies. Multivariate Behav Res 2011;46:399–424. doi: https://doi.org/10.1080/00273171.2011.568786
Momosaki R, Yasunaga H, Matsui H, Horiguchi H, Fushimi K, Abo M. Effect of dysphagia rehabilitation on oral intake in elderly patients with aspiration pneumonia. Geriatr Gerontol Int 2015;15:694–699. doi: https://doi.org/10.1111/ggi.12333
Ni-Chroinin D, Montalto A, Jahromi S, Ingham N, Beveridge A, Foltyn P. Oral health status is associated with common medical comorbidities in older hospital inpatients. J Am Geriatr Soc 2016;64:1696–1700. doi: https://doi.org/10.1111/jgs.14247
Azzolino D, Passarelli PC, De Angelis P, Piccirillo GB, D’Addona A, Cesari M. Poor oral health as a determinant of malnutrition and sarcopenia. Nutrients 2019;11:2898. doi: https://doi.org/10.3390/nu11122898
Koyama T, Maeda K, Anzai H, Koganei Y, Shamoto H, Wakabayashi H. Early commencement of oral intake and physical function are associated with early hospital discharge with oral intake in hospitalized elderly individuals with pneumonia. J Am Geriatr Soc 2015;63:2183–2185. doi: https://doi.org/10.1111/jgs.13679
Shiraishi A, Yoshimura Y, Wakabayashi H, Tsuji Y, Shimazu S, Jeong S. Impaired oral health status on admission is associated with poor clinical outcomes in post-acute inpatients: A prospective cohort study. Clin Nutr 2019;38:2677–2683.
Wu CP, Xu YJ, Wang TG, Ku SC, Chan DC, Lee JJ, Wei YC, Hsiao TY, Chen CC. Effects of a swallowing and oral care intervention for patients following endotracheal extubation: a pre- and post-intervention study. Crit Care 2019;23:350. doi: https://doi.org/10.1186/s13054-019-2623-2
Akiyama Y, Iwaya T, Endo F, Shioi Y, Kumagai M, Takahara T, Otsuka K, Nitta H, Koeda K, Mizuno M et al. Effectiveness of intervention with a perioperative multidisciplinary support team for radical esophagectomy. Support Care Cancer 2017;25:3733–3739. doi: https://doi.org/10.1007/s00520-017-3801-x
Aoki S, Hosomi N, Hirayama J, Nakamori M, Yoshikawa M, Nezu T, Kubo S, Nagano Y, Nagao A, Yamane N et al. The multidisciplinaiy swallowing team approach decreases pneumonia onset in acute stroke patients. PLoS One 2016;11:e0154608. doi: https://doi.org/10.1371/journal.pone.0154608
Obana M, Furuya J, Matsubara C, Tohara H, Inaji M, Miki K, Numasawa Y, Minakuchi S, Maehara T. Effect of a collaborative transdisciplinary team approach on oral health status in acute stroke patients. J Oral Rehabil 2019;46:1170–1176. doi: https://doi.org/10.1111/joor.12855
Acknowledgments
The authors would like to thank Mikako Nakamura at the Teikyo University School of Medicine, Mizonokuchi Hospital, for coordinating the study.
Funding
Funding: This study was supported by Japanese Dental Science Federation (JDSF-DSP1-2021-116-1).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical Standards: The experiments in this study comply with the current laws of the country in which they were performed.
Conflict of Interest Statement: The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Yoshimi, K., Nakagawa, K., Momosaki, R. et al. Effects of Oral Management on Elderly Patients with Pneumonia. J Nutr Health Aging 25, 979–984 (2021). https://doi.org/10.1007/s12603-021-1660-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12603-021-1660-0