Abstract
Objective
No studies analyzing the role of dementia as a risk factor for mortality in patients affected by COVID-19. We assessed the prevalence, clinical presentation and outcomes of dementia among subjects hospitalized for COVID19 infection.
Design
Retrospective study.
Setting
COVID wards in Acute Hospital in Brescia province, Northern Italy.
Participants
We used data from 627 subjects admitted to Acute Medical wards with COVID 19 pneumonia.
Measurements
Clinical records of each patients admitted to the hospital with a diagnosis of COVID19 infection were retrospectively analyzed. Diagnosis of dementia, modalities of onset of the COVID-19 infection, symptoms of presentation at the hospital and outcomes were recorded.
Results
Dementia was diagnosed in 82 patients (13.1%). The mortality rate was 62.2% (51/82) among patients affected by dementia compared to 26.2% (143/545) in subjects without dementia (p<0.001, Chi-Squared test). In a logistic regression model age, and the diagnosis of dementia resulted independently associated with a higher mortality, and patients diagnosed with dementia presented an OR of 1.84 (95% CI: 1.09–3.13, p<0.05). Among patients diagnosed with dementia the most frequent symptoms of onset were delirium, especially in the hypoactive form, and worsening of the functional status.
Conclusion
The diagnosis of dementia, especially in the most advanced stages, represents an important risk factor for mortality in COVID-19 patients. The clinical presentation of COVID-19 in subjects with dementia is atypical, reducing early recognition of symptoms and hospitalization.
Similar content being viewed by others
Introduction
In Italy, SARS-CoV-2 outbreak was catastrophic with 135,586 confirmed cases and 17,127 deaths at April, 8th (1). In clinical series of patients who died of COVID-19 comorbidities (especially hypertension, cardiac ischemic disease, diabetes and obesity) were identified as significant risk factors for mortality, while dementia was described as a comorbid condition in only 6.8% of COVID-19 patients (2).
Although dementia is known to be an important mortality risk factor among older people, so far there are no studies analyzing the role of dementia as a risk factor for mortality in patients affected by COVID-19 (3, 4).
In the Province of Brescia, an administrative district in eastern Lombardy home to 1.2 million people, between February 22nd and April 8th, 9,900 cases of Covid-19 have been diagnosed and 1,800 deaths have been reported. About 53% (2265 out of 4200) of hospital beds have been dedicated to treat patients affected by Covid-19 pneumonia. Specific units were created to cater to these patients: acute medical units, named COVID Wards, and intensive care units, with the last accounting fort the 8.5% of all the beds dedicated to COVID-19 patients.
Methods and study population
During this period, 627 patients diagnosed with COVID-19 pneumonia were admitted to our hospitals. All patients admitted to COVID Wards were positive to RT-PCR for SARS-Cov-2 conducted on a nasopharyngeal specimen and presented respiratory failure. Each patient underwent a thorough medical evaluation and, if over 65, a geriatric multi-dimensional assessment, comprehensive of evaluation of cognitive and functional status and presence of delirium.
Dementia was diagosed according to clinical history and results of the cognitive assessment. The modalities of onset of the COVID-19 infection, the symptoms of presentation at the hospital emergency department and the outcomes were recorded.
Results
Dementia was diagnosed in 82 patients (13.1%). The mean age of patients diagnosed with dementia was 82.6 (SD 5.3; IQR 80–86), versus 68.9 (SD 12.7; IQR 60–68) in patients not affected by dementia (p<0.001; Student’s t test). Females were 47 (57.3%) among patients with dementia and 288 (52.8%) among patients not diagnosed with dementia, respectively.
The mortality rate was 62.2% (51/82) among patients affected by dementia compared to 26.2% (143/545) in subjects without dementia (p<0.001, Chi-Squared test). (Table 1)
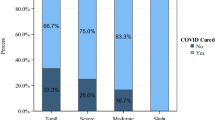
The Clinical Dementia Rating Scale (CDR) (5) was used to determine the severity of dementia: 36 patients (43.4%) were classified in stage 1, 15 (18.3%) in stage 2 and 31 (37.8%) in stage 3. The Mortality rates were, respectively, 41.7%, 66.7%, and 83.9% (p<0.001, one-way ANOVA). (table 2)
To assess if the diagnosis of dementia was associated with a worse outcome regardless of age and sex, we built a logistic regression model. According to this model age, and the diagnosis of dementia resulted independently associated with a higher mortality. For every increased year of age, the Odds Ratio (OR) for mortality was 1.09 (95% CI: 1.07–1.12, p<0.001), and patients diagnosed with dementia presented an OR of 1.84 (95% CI: 1.09–3.13, p<0.05). According to this model sex was not associated with a change in mortality risk. (Table 3)
As shown in table 4, among patients diagnosed with dementia the most frequent symptoms of onset were delirium (67%, especially in the hypoactive form, 50%) and worsening of the functional status. The classic symptoms of COVID-19 infection were less frequent: only 47% of patients had fever, 44% dyspnea and 14% cough.
Conclusions
Caring for patients with dementia during the current pandemic is a complex task, involving the management of patients in different settings. Some patients need to be treated at home, often with caregivers burdened by isolation due to lockdown measures and by limitation of home services. Other patients are cared in nursing homes, which often lack adequate and trained staffs and access to personal protective equipment. Hospital patient’s management has been difficult due to the scarce collaboration offered by the patient and difficulties in communication, immobility, and limited availability of trained staff members (6). There are also ethical concerns regarding hospitalization of patients with dementia due to resource constraints during the current pandemic (7).
To our knowledge, the proportion of subjects with dementia among patients admitted to an acute hospital for COVID-19 has never been evaluated. The prevalence of demented patient found in the present study (13.1%) is lower than the previous estimates of the prevalence of dementia in hospital, which vary from 15% to 42% (7). According to our data, the diagnosis of dementia, especially in the most advanced stages, represents an important risk factor for mortality in COVID-19 patients. The clinical presentation of COVID-19 in subjects with dementia is atypical, reducing early recognition of symptoms and hospitalization. We suggest that the onset of hypoactive delirium and worsening functional status in people with dementia may be considered a sign of possible COVID-19 infection during this epidemic. Early recognition of COVID-19 in demented people can help provide timely treatment and adequate isolation. Hospitals should develop integrated care models, create Special Care Geriatric COVID units and promote guidelines to ensure the better possible treatment for frail older persons.
References
Word Health Organization. Coronavirus disease 2019 (COVID-19) Situation Report - 79. Available at: https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200408-sitrep-79-covid-19.pdf?sfvrsn=4796bl43_4
Onder G, Rezza G, Brusaferro S. Case-Fatality Rate and Characteristics of Patients Dying in Relation to COVID-19 in Italy. JAMA. Published online March 23, 2020. doi:https://doi.org/10.1001/jama.2020.4683
Morandi A, Di Santo SG, Zambón A et al, Italian Study Group on Delirium (ISGoD). Delirium, Dementia, and In-Hospital Mortality: The Results From the Italian Delirium Day 2016, A National Multicenter Study. J Gerontol A Biol Sci Med Sci;2019;74:910–916.
D’Adamo H, Yoshikawa T, Ouslander JG. Coronavirus Disease 2019 in Geriatrics and Long-term Care: The ABCDs of COVID-19. JAGS 2020;doi: https://doi.org/10.1111/jgs.16445
Hughes CP, Berg L, Danziger WL, Coben LA, Martin RL. A new clinical scale for the staging of dementia. The British Journal of Psychiatry; 1982;140, 566–572.
Wang H, Li T, Barbarino P, Gauthier S, Brodaty H, Molinuevo JL, Xie H, Sun Y, Yu E, Tang Y, Weidner W, Yu X. Dementia care during COVID-19. Lancet. 2020;395(10231):1190–1191. doi: https://doi.org/10.1016/S0140-6736(20)30755-8. Epub 2020 Mar 30.
Aprahamian I, Cesari M. Geriatric Syndromes and SARS-COV-2: More than Just Being Old [published online ahead of print,]. J Frailty Aging. 2020;1–3. doi:https://doi.org/10.14283/jfa.2020.17
Jackson TA, Gladman JR, Harwood RH et al. Challenges and opportunities in understanding dementia and delirium in the acute hospital. PLoS Med:e 2017;1002247.
Acknowledgement
Anita Chizzoli, MD; Marzia Cristo, MD; Silvia Comini, MD; Assunta Di Stasio, MD and Antonella Ricci, MD for the support in clinical evaluation of patients.
Funding
Funding: No funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest/Competing interests: The authors declare that they have no conflict of interest.
Ethics approval: This is a review study; the protocol was approved by the institutional committee.
Rights and permissions
About this article
Cite this article
Bianchetti, A., Rozzini, R., Guerini, F. et al. Clinical Presentation of COVID19 in Dementia Patients. J Nutr Health Aging 24, 560–562 (2020). https://doi.org/10.1007/s12603-020-1389-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12603-020-1389-1