Abstract
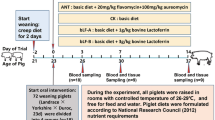
Probiotics could promote animal growth and enhance immune function. This study investigated the effects of Clostridium butyricum (CB) on the growth performance, intestinal immune, and gut microbiota of weaning rex rabbits. A total of 60 healthy female rabbits (5-month-old) were divided equally into four groups and mated on the same day: control group (CTRL, fed with basal feed), low-dose group (LDG, fed with basal feed + 1.0 × 103 CFU/g CB), middle-dose group (MDG, fed with basal feed + 1.0 × 104 CFU/g CB), and high-dose group (HDG, fed with basal feed + 1.0 × 105 CFU/g CB). Then, 30 weaning rex rabbits (35-day-old) were collected from each group for this experiment, and they were offered the same feeds as their mother. The results demonstrated that high-dose CB treatment significantly increased average daily weight gain of weaning rex rabbits. Further studies suggested that CB enhanced small intestinal digestive enzyme activity and improved mucosal morphology and antioxidant status. Supplemented with CB, small intestinal barrier function was maintained with the upregulation of mRNA levels of ZO-1, claudin, and occludin as well as the increase of sIgA production. Moreover, the relative expressions of MyD88, TLR2, and TLR4 were elevated in HDG; simultaneously, pro-inflammatory cytokines including IL-6, INF-γ, and TNF-α were decreased after CB administration. In addition, CB showed beneficial effects in improving weaning rex rabbit intestinal microflora via increasing the abundance of beneficial bacteria. Therefore, our results indicated CB can promote rex rabbit growth, which is likely to the enhancement of immune function and the improvement of intestinal microbiota.







Similar content being viewed by others
References
Zhu Y, Wang C, Li F (2015) Impact of dietary fiber/starch ratio in shaping caecal microbiota in rabbits. Can J Microbiol 61(10):771–784. https://doi.org/10.1139/cjm-2015-0201
Barton MD (2000) Antibiotic use in animal feed and its impact on human health. Nutr Res Rev 13(2):279–299. https://doi.org/10.1079/095442200108729106
Zou F, Zeng D, Wen B, Sun H, Zhou Y, Yang M, Peng Z, Xu S, Wang H, Fu X, Du D, Zeng Y, Zhu H, Pan K, Jing B, Wang P, Ni X (2016) Illumina Miseq platform analysis caecum bacterial communities of rex rabbits fed with different antibiotics. AMB Express 6(1):100. https://doi.org/10.1186/s13568-016-0273-1
He GQ, Kong Q, Ding LX (2004) Response surface methodology for optimizing the fermentation medium of Clostridium butyricum. Lett Appl Microbiol 39(4):363–368. https://doi.org/10.1111/j.1472-765X.2004.01595.x
Nakanishi S, Tanaka M (2010) Sequence analysis of a bacteriocinogenic plasmid of Clostridium butyricum and expression of the bacteriocin gene in Escherichia coli. Anaerobe 16(3):253–257. https://doi.org/10.1016/j.anaerobe.2009.10.002
Liu L, Tian Y, Ni X, Zeng D, Pan K, Wang H (2017) Optimization of carbon and nitrogen sources of Clostridium butyricum CBM01 and its tolerance to gastrointerestinal tract.[in Chinese] Chinese Journal of Animal Nutrition 29(10):3831–3836. https://doi.org/10.3969/j.issn.1006?267x.2017.10.047
Duan Y, Zhang Y, Dong H, Wang Y, Zhang J (2017) Effect of the dietary probiotic Clostridium butyricum on growth, intestine antioxidant capacity and resistance to high temperature stress in kuruma shrimp Marsupenaeus japonicus. J Therm Biol 66:93–100. https://doi.org/10.1016/j.jtherbio.2017.04.004
Imase K, Takahashi M, Tanaka A, Tokunaga K, Sugano H, Tanaka M, Ishida H, Kamiya S, Takahashi S (2008) Efficacy of Clostridium butyricum preparation concomitantly with Helicobacter pylori eradication therapy in relation to changes in the intestinal microbiota. Microbiol Immunol 52(3):156–161. https://doi.org/10.1111/j.1348-0421.2008.00026.x
Kong Q, He GQ, Jia JL, Zhu QL, Ruan H (2011) Oral administration of Clostridium butyricum for modulating gastrointestinal microflora in mice. Curr Microbiol 62(2):512–517. https://doi.org/10.1007/s00284-010-9737-8
Li HH, Li YP, Zhu Q, Qiao JY, Wang WJ (2018) Dietary supplementation with Clostridium butyricum helps to improve the intestinal barrier function of weaned piglets challenged with enterotoxigenic Escherichia coli K88. J Appl Microbiol 125:964–975. https://doi.org/10.1111/jam.13936
Sun J, Wang F, Ling Z, Yu X, Chen W, Li H, Jin J, Pang M, Zhang H, Yu J, Liu J (2016) Clostridium butyricum attenuates cerebral ischemia/reperfusion injury in diabetic mice via modulation of gut microbiota. Brain Res 1642:180–188. https://doi.org/10.1016/j.brainres.2016.03.042
Takahashi M, Taguchi H, Yamaguchi H, Osaki T, Komatsu A, Kamiya S (2004) The effect of probiotic treatment with Clostridium butyricum on enterohemorrhagic Escherichia coli O157:H7 infection in mice. FEMS Immunol Med Microbiol 41(3):219–226. https://doi.org/10.1016/j.femsim.2004.03.010
Woo TD, Oka K, Takahashi M, Hojo F, Osaki T, Hanawa T, Kurata S, Yonezawa H, Kamiya S (2011) Inhibition of the cytotoxic effect of Clostridium difficile in vitro by Clostridium butyricum MIYAIRI 588 strain. J Med Microbiol 60(11):1617–1625. https://doi.org/10.1099/jmm.0.033423-0
Zhang L, Cao GT, Zeng XF, Zhou L, Ferket PR, Xiao YP, Chen AG, Yang CM (2014) Effects of Clostridium butyricum on growth performance, immune function, and cecal microflora in broiler chickens challenged with Escherichia coli K88. Poult Sci 93(1):46–53. https://doi.org/10.3382/ps.2013-03412
Shang H, Jia S, Chen YQ (2016) Clostridium Butyricum CGMCC0313.1 modulates lipid profile, insulin resistance and colon homeostasis in obese mice. PLoS One 11(4):e0154373. https://doi.org/10.1371/journal.pone.0154373
Liao X, Wu R, Ma G, Zhao L, Zheng Z, Zhang R (2015) Effects of Clostridium butyricum on antioxidant properties, meat quality and fatty acid composition of broiler birds. Lipids Health Dis 14(1):36. https://doi.org/10.1186/s12944-015-0035-0
Kashiwagi I, Morita R, Schichita T, Komai K, Saeki K, Matsumoto M, Takeda K, Nomura M, Hayashi A, Kanai T, Yoshimura A (2015) Smad2 and Smad3 inversely regulate TGF-β autoinduction in Clostridium butyricum-activated dendritic cells. Immunity 43(1):65–79. https://doi.org/10.1016/j.immuni.2015.06.010
Gomez de Agüero M, Ganal-Vonarburg SC, Fuhrer T, Rupp S, Uchimura Y, Li H, Steinert A, Heikenwalder M, Hapfelmeier S, Sauer U, McCoy KD, Macpherson AJ (2016) The maternal microbiota drives early postnatal innate immune development. Science 351(6279):1296–1302. https://doi.org/10.1126/science.aad2571
Zijlmans MA, Korpela K, Riksen-Walraven JM, de Vos WM, de Weerth C (2015) Maternal prenatal stress is associated with the infant intestinal microbiota. Psychoneuroendocrinology 53:233–245. https://doi.org/10.1016/j.psyneuen.2015.01.006
Zhao X, Guo Y, Guo S, Tan J (2013) Effects of Clostridium butyricum and Enterococcus faecium on growth performance, lipid metabolism, and cecal microbiota of broiler chickens. Appl Microbiol Biotechnol 97(14):6477–6488. https://doi.org/10.1007/s00253-013-4970-2
Rawski M, Kierończyk B, Długosz J, Świątkiewicz S, Józefiak D (2016) Dietary probiotics affect gastrointestinal microbiota, histological structure and shell mineralization in turtles. PLoS One 11(2):e0147859. https://doi.org/10.1371/journal.pone.0147859
Latorre E, Mendoza C, Layunta E, Alcalde AI, Mesonero JE (2014) TLR2, TLR3, and TLR4 activation specifically alters the oxidative status of intestinal epithelial cells. Cell Stress Chaperones 19(2):289–293. https://doi.org/10.1007/s12192-013-0461-8
Chiva M, Guarner C, Peralta C, Llovet T, Gómez G, Soriano G, Balanzó J (2003) Intestinal mucosal oxidative damage and bacterial translocation in cirrhotic rats. Eur J Gastroenterol Hepatol 15(2):145–150. https://doi.org/10.1097/00042737-200302000-00007
Kasprzak KS (1991) The role of oxidative damage in metal carcinogenicity. Chem Res Toxicol 4(6):604–615. https://doi.org/10.1021/tx00024a002
Shen X, Yi D, Ni X, Zeng D, Jing B, Lei M, Bian Z, Zeng Y, Li T, Xin J (2014) Effects of Lactobacillus plantarum on production performance, immune characteristics, antioxidant status, and intestinal microflora of bursin-immunized broilers. Can J Microbiol 60(4):193–202. https://doi.org/10.1139/cjm-2013-0680
Amaretti A, Nunzio MD, Pompei A, Raimondi S, Rossi M, Bordoni A (2013) Antioxidant properties of potentially probiotic bacteria: in vitro and in vivo activities. Appl Microbiol Biotechnol 97(2):809–817. https://doi.org/10.1007/s00253-012-4241-7
Chauhan R, Vasanthakumari AS, Panwar H, Mallapa RH, Duary RK, Batish VK, Grover S (2014) Amelioration of colitis in mouse model by exploring antioxidative potentials of an indigenous probiotic strain of Lactobacillus fermentum Lf1. Biomed Res Int 2014:206732. https://doi.org/10.1155/2014/206732, 1, 12
Martarelli D, Verdenelli MC, Scuri S, Cocchioni M, Silvi S, Cecchini C, Pompei P (2011) Effect of a probiotic intake on oxidant and antioxidant parameters in plasma of athletes during intense exercise training. Curr Microbiol 62(6):1689–1696. https://doi.org/10.1007/s00284-011-9915-3
Aluwong T, Kawu M, Raji M, Dzenda T, Govwang F, Sinkalu V, Ayo J (2013) Effect of yeast probiotic on growth, antioxidant enzyme activities and malondialdehyde concentration of broiler chickens. Antioxidants 2(4):326–339. https://doi.org/10.3390/antiox2040326
Esteban MA, Cordero H, Martínez-Tomé M, Jiménez-Monreal AM, Bakhrouf A, Mahdhi A (2014) Effect of dietary supplementation of probiotics and palm fruits extracts on the antioxidant enzyme gene expression in the mucosae of gilthead seabream ( Sparus aurata L.). Fish Shellfish Immunol 39(2):532–540. https://doi.org/10.1016/j.fsi.2014.06.012
Merska M, Czech A, Ognik K (2015) The effect of yeast Yarrowia lipolytica on the antioxidant indices and macro- and microelements in blood plasma of turkey hens. Pol J Vet Sci 18(4):709–714. https://doi.org/10.1515/pjvs-2015-0092
Mantis NJ, Rol N, Corthésy B (2011) Secretory IgA’s complex roles in immunity and mucosal homeostasis in the gut. Mucosal Immunol 4(6):603–611. https://doi.org/10.1038/mi.2011.41
Kotani Y, Shinkai S, Okamatsu H, Toba M, Ogawa K, Yoshida H, Fukaya T, Fujiwara Y, Chaves PH, Kakumoto K, Kohda N (2010) Oral intake of Lactobacillus pentosus strain b240 accelerates salivary immunoglobulin A secretion in the elderly: a randomized, placebo-controlled, double-blind trial. Immun Ageing 7(1):11. https://doi.org/10.1186/1742-4933-7-11
Anderson RC, Cookson AL, Mcnabb WC, Park Z, Mccann MJ, Kelly WJ, Roy NC (2010) Lactobacillus plantarum MB452 enhances the function of the intestinal barrier by increasing the expression levels of genes involved in tight junction formation. BMC Microbiol 10(1):316. https://doi.org/10.1186/1471-2180-10-316
Navasa M, Follo A, Filella X, Jiménez W, Francitorra A, Planas R, Rimola A, Arroyo V, Rodés J (1998) Tumor necrosis factor and interleukin-6 in spontaneous bacterial peritonitis in cirrhosis: relationship with the development of renal impairment and mortality. Hepatology 27(5):1227–1232. https://doi.org/10.1002/hep.510270507
Gao Q, Qi L, Wu T, Wang J (2012b) An important role of interleukin-10 in counteracting excessive immune response in HT-29 cells exposed to Clostridium butyricum. BMC Microbiol 12(1):100. https://doi.org/10.1186/1471-2180-12-100
Maloy KJ, Powrie F (2011) Intestinal homeostasis and its breakdown in inflammatory bowel disease. Nature 474(7351):298–306. https://doi.org/10.1038/nature10208
Maynard CL, Harrington LE, Janowski KM, Oliver JR, Zindl CL, Rudensky AY, Weaver CT (2007) Regulatory T cells expressing interleukin 10 develop from Foxp3+ and Foxp3- precursor cells in the absence of interleukin 10. Nat Immunol 8(9):931–941. https://doi.org/10.1038/ni1504
Siegmund B, Sennello JA, Lehr HA, Batra A, Fedke I, Zeitz M, Fantuzzi G (2004) Development of intestinal inflammation in double IL-10- and leptin-deficient mice. J Leukoc Biol 76(4):782–786. https://doi.org/10.1189/jlb.0404239
Shkoda A, Ruiz PA, Daniel H, Kim SC, Rogler G, Sartor RB, Haller D (2007) Interleukin-10 blocked endoplasmic reticulum stress in intestinal epithelial cells: impact on chronic inflammation. Gastroenterology 132(1):190–207. https://doi.org/10.1053/j.gastro.2006.10.030
Hayashi A, Sato T, Kamada N, Mikami Y, Matsuoka K, Hisamatsu T, Hibi T, Roers A, Yagita H, Ohteki T, Yoshimura A, Kanai T (2013) A single strain of Clostridium butyricum induces intestinal IL-10-producing macrophages to suppress acute experimental colitis in mice. Cell Host Microbe 13(6):711–722. https://doi.org/10.1016/j.chom.2013.05.013
Kanai T, Mikami Y, Hayashi A (2015) A breakthrough in probiotics: Clostridium butyricum regulates gut homeostasis and anti-inflammatory response in inflammatory bowel disease. J Gastroenterol 50(9):928–939. https://doi.org/10.1007/s00535-015-1084-x
Grivennikov S, Karin E, Terzic J, Mucida D, Yu GY, Vallabhapurapu S, Scheller J, Rose-John S, Cheroutre H, Eckmann L, Karin M (2009) IL-6 and Stat3 are required for survival of intestinal epithelial cells and development of colitis-associated cancer. Cancer Cell 15(2):103–113. https://doi.org/10.1016/j.ccr.2009.01.001
Cortes A, Sotillo J, Muñozantoli C, Fried B, Esteban JG, Toledo R (2014) Intestinal IFN-γ production is associated with protection from clinical signs, but not with elimination of worms, in Echinostoma caproni infected-mice. Parasitol Res 113(6):2037–2045. https://doi.org/10.1007/s00436-014-3851-7
He C, Shi Y, Wu R, Sun M, Fang L, Wu W, Liu C, Tang M, Li Z, Wang P, Cong Y, Liu Z (2015) miR-301a promotes intestinal mucosal inflammation through induction of IL-17A and TNF-α in IBD. Gut 65(12):1938–1950. https://doi.org/10.1136/gutjnl-2015-309389
Iwasaki A, Medzhitov R (2004) Toll-like receptor control of the adaptive immune responses. Nat Immunol 5(10):987–995. https://doi.org/10.1038/ni1112
Okamoto M, Hirai H, Taniguchi K, Shimura K, Inaba T, Shimazaki C, Taniwaki M, Imanishi J (2009) Toll-like receptors (TLRs) are expressed by myeloid leukaemia cell lines, but fail to trigger differentiation in response to the respective TLR ligands. Br J Haematol 147(4):585–587. https://doi.org/10.1111/j.1365-2141.2009.07858.x
Gao Q, Qi L, Wu T, Wang J (2012a) Clostridium butyricum activates TLR2-mediated MyD88-independent signaling pathway in HT-29 cells. Mol Cell Biochem 361(1–2):31–37. https://doi.org/10.1007/s11010-011-1084-y
Quanxin G, Lili Q, Tianxing W, Tingting X, Jinbo W (2013) Immunomodulatory effects of Clostridium butyricum on human enterocyte-like HT-29 cells. Anim Cells Syst 17(2):121–126. https://doi.org/10.1080/19768354.2013.789075
Takeda K, Akira S (2005) Toll-like receptors in innate immunity. Int Immunol 17(1):1–14. https://doi.org/10.1093/intimm/dxh186
Magrone T, Jirillo E (2013) The interplay between the gut immune system and microbiota in health and disease: nutraceutical intervention for restoring intestinal homeostasis. Curr Pharm Des 19(7):1329–1342. https://doi.org/10.2174/138161213804805793
Thomas F, Hehemann JH, Rebuffet E, Czjzek M, Michel G (2011) Environmental and gut bacteroidetes: the food connection. Front Microbiol 2(93):93. https://doi.org/10.3389/fmicb.2011.00093
Brousseau JP, Talbot G, Beaudoin F, Lauzon K, Roy D, Lessard M (2015) Effects of probiotics Pediococcus acidilactici strain MA18/5M and Saccharomyces cerevisiae subsp. boulardii strain SB-CNCM I-1079 on fecal and intestinal microbiota of nursing and weanling piglets. J Anim Sci 93(11):5313–5326. https://doi.org/10.2527/jas.2015-9190
Zhang SL, Wang SN, Miao CY (2017) Influence of microbiota on intestinal immune system in ulcerative colitis and its intervention. Front Immunol 8:1674. https://doi.org/10.3389/fimmu.2017.01674
Atarashi K, Tanoue T, Shima T, Imaoka A, Kuwahara T, Momose Y, Cheng G, Yamasaki S, Saito T, Ohba Y, Taniguchi T, Takeda K, Hori S, Ivanov II, Umesaki Y, Itoh K, Honda K (2011) Induction of colonic regulatory T cells by indigenous Clostridium species. Science 331(6015):337–341. https://doi.org/10.1126/science.1198469
Atarashi K, Tanoue T, Oshima K, Suda W, Nagano Y, Nishikawa H, Fukuda S, Saito T, Narushima S, Hase K, Kim S, Fritz JV, Wilmes P, Ueha S, Matsushima K, Ohno H, Olle B, Sakaguchi S, Taniguchi T, Morita H, Hattori M, Honda K (2013) Treg induction by a rationally selected mixture of Clostridia strains from the human microbiota. Nature 500(7461):232–236. https://doi.org/10.1038/nature12331
Garrett WS, Gordon JI, Glimcher LH (2010) Homeostasis and inflammation in the intestine. Cell 140(6):859–870. https://doi.org/10.1016/j.cell.2010.01.023
Hooper LV, Dan RL, Macpherson AJ (2012) Interactions between the microbiota and the immune system. Science 336(6086):1268–1273. https://doi.org/10.1126/science.1223490
Wang H, Gong J, Wang W, Long Y, Fu X, Fu Y, Qian W, Hou X (2014) Are there any different effects of Bifidobacterium, Lactobacillus and Streptococcus on intestinal sensation, barrier function and intestinal immunity in PI-IBS mouse model? PLoS One 9(3):e90153. https://doi.org/10.1371/journal.pone.0090153
Wang Y, Xie J, Li Y, Dong S, Liu H, Chen J, Wang Y, Zhao S, Zhang Y, Zhang H (2016) Probiotic Lactobacillus casei Zhang reduces pro-inflammatory cytokine production and hepatic inflammation in a rat model of acute liver failure. Eur J Nutr 55(2):821–831. https://doi.org/10.1007/s00394-015-0904-3
Klein A, Friedrich U, Vogelsang H, Jahreis G (2008) Lactobacillus acidophilus 74-2 and Bifidobacterium animalis subsp lactis DGCC 420 modulate unspecific cellular immune response in healthy adults. Eur J Clin Nutr 62(5):584–593. https://doi.org/10.1038/sj.ejcn.1602761
Munita JM, Arias CA, Murray BE (2012) Enterococcal endocarditis: can we win the war? Curr Infect Dis Rep 14(4):339–349. https://doi.org/10.1007/s11908-012-0270-8
Funding
This study was funded by the Natural Science project of Chengdu Technology Bureau, the Research on Key Technology Integration and Industrialization Demonstration of Modern Industrial Chain in Rabbit (15ZC0725), the 13th Five-year Livestock and poultry breeding Project “High Quality Characteristics of Rabbit Breeding Cross System and Breeding Material Innovation” (2016NYZ0046), and the Rabbit Industrial Technology of China Agriculture Research System (CARS-44-A-4).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical Approval
All applicable international, national, and/or institutional guidelines for the care and use of animals were followed. This article does not contain any studies with human participants performed by any of the authors.
Rights and permissions
About this article
Cite this article
Liu, L., Zeng, D., Yang, M. et al. Probiotic Clostridium butyricum Improves the Growth Performance, Immune Function, and Gut Microbiota of Weaning Rex Rabbits. Probiotics & Antimicro. Prot. 11, 1278–1292 (2019). https://doi.org/10.1007/s12602-018-9476-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12602-018-9476-x