Abstract
Viruses are the causative agents of an estimated 60% of human infections worldwide. The most common viral illnesses are produced by enteric and respiratory viruses. Transmission of these viruses from an infected person or animal to a new host can occur via several routes. Existing studies strongly suggest that contaminated fomites or surfaces play an important role in the spreading of viral diseases. The potential of viral spreading via contaminated surfaces depends particularly on the ability of the virus to maintain infectivity whilst it is in the environment. This is affected by a combination of biological, physical and chemical factors. This review summarises current knowledge about the influence of environmental factors on the survival and spread of viruses via contaminated surfaces.
Similar content being viewed by others
Introduction
Viruses are causative agents of an estimated 60% of human infections worldwide (Barker et al. 2001). For centuries it was assumed that these viral diseases were spread primarily through direct patient contact or by the airborne route, and surrounding environment played little or no role in disease transmissions. Due to the opinion that nosocomial infections were not related to microbial contamination of surfaces, the Centre for Disease Control (CDC) and the American Hospital Association focussed only on patient diagnosis up to 1987. Over the years studies have changed perspectives on viral transmission and have integrated a more complex multifactorial model of disease spreading including the contaminated environment (Boone and Gerba 2007).
Viral transmission from an infected person or an animal to a new host can occur by direct or indirect routes. During indirect transmission, contaminated surfaces can play an important role. This kind of transmission is dependent on several factors, which include the quantity of viral particles excreted by an infected organism, their stability in the environment, the potential to spread within a closed environment, as well as interaction of the virus and the host organism. Large numbers of viral particles can be shed via various body fluids including blood, faeces, vomit, saliva, urine, and respiratory secretions from infected individuals or carriers. The more viruses are shed, the greater their chance is to survive and reach a new host organism (Rzezutka and Cook 2004).
A critical factor of viral transmission is its ability to survive in the environment. Previous studies have shown that viral particles can persist for extended periods on surfaces such as medical devices, fomites or human skin (Abad et al. 2001; Sattar et al. 1986, 1987; Todd et al. 2009). Even if some viruses survive relatively poorly in the environment, the low infective dose suggests that these viruses are able to persist in sufficient numbers to act as a source of infection for several days, week or in some cases months (Barker et al. 2001; Boone and Gerba 2007).
Surfaces can be contaminated directly by their contact with body secretions and fluids or indirectly through virus contaminated aerosol or other contaminated fomites. Once a surface is contaminated, the transfer of infectious viral particles may easily occur between inanimate or animated objects, or vice versa, e.g. hands and work surfaces with the potential of subsequent transfer to food or direct hand-to-mouth transfer (Goldmann 2000; Marks et al. 2000; Rzezutka and Cook 2004). Rapid spread of viral infections through contaminated surfaces is common particularly in crowded indoor establishments such as schools, day-care facilities, nursing homes, business offices, hospitals or transport systems (Barker et al. 2001). The influences of environmental factors on the stability and spread of bacterial infections are well documented, especially in hospitals. The comparable knowledge concerning the role of surfaces or fomites in viral transmission is still lacking and further investigation is needed (Boone and Gerba 2007; von Rheinbaben et al. 2000).
The objective of this review is to summarise current knowledge about influences of environmental factors on survival and spread of viruses via contaminated surfaces.
Viruses Spread Via Contaminated Fomites
Nearly one thousand different types of viruses are known to infect humans, whilst the most common viral illnesses are produced by enteric and respiratory viruses (Barker et al. 2001). In developed countries, viruses are responsible approximately for 30–40% of infectious gastroenteritis cases. Estimates indicate that adults have two to five colds per year and infants or preschool children four to eight colds per year. Existing studies prove that contaminated fomites play an important role in the spreading of these diseases (Barker et al. 2004; Winther et al. 2006; Wu et al. 2005).
Viral Gastroenteritis and Hepatitis
Viruses that infect a host organism via the gastrointestinal tract are excreted in faeces and may be also present in vomit (Seymour and Appleton 2001). Normally they are shed in high numbers and exhibit great particle stability outside the organism and on passage through the stomach. There are two types of viruses infecting gastrointestinal tract:
-
1.
Capable of primarily multiplying in the intestine. These agents cause gastroenteritis, and include members of genus: Rotavirus, Norovirus, Astrovirus and Adenovirus. Viral gastroenteritis is usually relatively mild disease, which has a short incubation period (1–4 days) depending on the virus species. Specific symptoms are diarrhoea and vomiting. Most infected people do not consult a medical practitioner. Therefore, the majority of cases is not reported and subsequently investigated.
-
2.
Capable of multiplying elsewhere in the body. These viruses include enteroviruses (e.g. poliovirus or Coxsackievirus), hepatitis A virus (HAV) and hepatitis E virus (HEV). Infection by enteroviruses is often subclinical but they may induce signs and symptoms of disease in not related with intestinal tissue. The infections caused by hepatitis viruses affect liver tissue (Carter 2005).
Recent epidemiological studies have shown that norovirus is one of the most frequent cause of acute non-bacterial gastroenteritis. Additionally, it is responsible for almost all foodborne outbreaks, where viruses are identified (Goodgame 2006; Koopmans and Duizer 2004). A study by Barker et al. (2004) demonstrated that noroviruses could be transferred from contaminated surfaces to clean hands. It was also found that norovirus-contaminated hands could cross-contaminate a series of seven types of clean surfaces. Wu et al. (2005) tested ten environmental samples taken during the norovirus outbreak at a long-term-care facility. Positive swabs were obtained from toilet seats used by case-residents, bed rails from case-residents’ bed, a dining room tabletop and an elevator button.
Worldwide, rotavirus is probably the most important pathogen causing diarrhoeal disease in infants. Rotaviruses are shed in large numbers from infected person with faeces often containing 108–1011 virions per gram (Bajolet and Chippaux-Hyppolite 1998; Leung et al. 2005). It has been demonstrated that infective viral particles can survive on human hands and be transferred to animate and non-porous surfaces (Ansari et al. 1988; Sattar et al. 1986). Ward et al. (1991) examined the transmission of rotavirus from a contaminated surface to the mouth and from surface to hands and mouth. All the volunteers who licked rotavirus-contaminated plates became infected. Whereas, only about half of individuals touching the virus contaminated plates with their fingers and then their mouth became infected.
Infections caused by HAV are endemic throughout the world. Transfer of infectious viral particles from contaminated to clean surfaces was also reported. The persistence of HAV on surfaces and the ability of the virus to be interchanged from animate and inanimate environments confirm that surfaces present important epidemiological factors in the indirect transmission of HAV (Croci et al. 2002; Bidawid et al. 2000; Mbithi et al. 1992). Mbithi et al. (1992) presented that considerable amounts of HAV remained infectious on finger pads after 4 h, even though 68% of viruses lost their infectivity during the first hour.
Astroviruses or adenoviruses exhibited shorter survival time than rotaviruses and HAV. Despite this, they were able to survive on inert surfaces long enough to suggest that contaminated surfaces may have a relevant role in the secondary transmission of these viruses (Abad et al. 2001). Information about the survival of HEV in environment is still lacking.
Respiratory Infections
Respiratory viral infections are a major health burden (Winther et al. 2006). Although these diseases are often regarded as trivial, hospital admission and mortality rates in infant or elderly are considerable. For instance, respiratory viruses cause more than 400,000 hospitalizations per year in children less than 18 years of age in the United States (Henrickson et al. 2004). Viral agents that primarily infect the upper or lower respiratory tract include influenza and parainfluenza viruses, adenoviruses, respiratory syncytial virus (RSV), coronaviruses, human metapneumovirus, rhinoviruses and enteroviruses (Kesson 2007).
It is generally accepted that respiratory viruses are spread from person to person by aerosol transmission due to sneezing or coughing (Goldmann 2000). Additionally, there is evidence to suggest that a significant proportion of flu viruses and other respiratory viruses are spread via contaminated hands and fomites (Hall et al. 1980; Tiwari et al. 2006; Winther et al. 2007).
RSV was recovered from counters for up to 6 h, from rubber gloves for up to 1.5 h, from clothing gowns and paper tissue for 30–45 min, and from skin for up to 20 min. Additional experiments demonstrated that infectious RSV could be transferred to hands by touching these contaminated surfaces and could be further recovered from these hands for up to 25 min (Hall et al. 1980). A study done by Winther et al. (2007) was designed to assess rhinovirus contamination of surfaces and rhinovirus transfer from these surfaces to fingertips during normal daily activities of adults. Common virus-positive sites were door handles, pens, light switches, TV remote controls, faucets and telephones. Rhinovirus was transferred from surfaces to fingertips in 60% trials 1 h after contamination and in 33% after 18 h after contamination.
Influenza viruses, and parainfluenza viruses are also able to survive on hands long enough to permit self-inoculation. It has been demonstrated that these infectious viral particles could be transferred from hands and fingers to surfaces and back again (Brady et al. 1990; Gwaltney and Hendley 1982; Hendley et al. 1973; Winther et al. 2007).
Factors Affecting Virus Survival on Surfaces
The potential of viral spreading via contaminated surfaces depends particularly on the ability of the viruses to maintain infectivity whilst they are in the environment (Boone and Gerba 2007). Their survival in the environment is affected by a combination of biological, physical and chemical factors (Fig. 1). To date, complete information regarding the influence of the environment on all viruses and their stability in external conditions does not exist. Most studies have used only few target viruses or their surrogates. Since experimental condition and methods vary, it is difficult to draw conclusions from these studies (Carter 2005).
Once the surface is contaminated, it can be source of contamination for other animate or inanimate objects, e.g. contaminated door handles and hands were found to be an efficient vector of viruses. At least 14 persons could be contaminated or infected by touching a polluted door handle. Successive transmission of virus from one person to another could be followed up to the sixth contact person (von Rheinbaben et al. 2000). It was also found that contaminated fingers could subsequently transfer a virus from up to seven clean surfaces (Barker et al. 2004).
Virus Characterisation and Classification
The most important aspects affecting virus survival are biological factors like the presence of the envelope and virus type. These basic characteristics influence and help to predict virus survival in the environment and behaviour in a host organism.
Persistence of a virus in the environment is primarily affected by the presence of a viral envelope. The non-enveloped viruses have higher resistance to drying or desiccation methods and therefore are spread more easily than enveloped viruses (which are less stable in the environment). The non-enveloped enteric viruses like HAV, rotavirus or astrovirus are able to remain infective on surfaces for at least 2 months. In contrast, enveloped respiratory viruses usually remain infectious for several hours to several days (Duizer et al. 2004). Reovirus, non-enveloped virus, when dried in an organic matrix can survive for a period of 30 days, whereas the enveloped Sindibis virus dies rapidly (Howie et al. 2008).
Variation in virus survival occurs within a viral family or even genus. Feline calicivirus (FCV) and norovirus belong to the same family. Their physicochemical properties and genome organisation are similar. Therefore, FCV is used as a surrogate model, e.g. to determine the efficacy of disinfectants against norovirus on fresh produce or surfaces (Gulati et al. 2001). Duizer et al. (2004) reported that norovirus is profoundly more resistant to low and high pH than FCV and canine calicivirus, which are members of the same family. Hewitt and Greening (2004) mentioned that in comparison to norovirus, FCV is more sensitive to environmental factors in general. Examples of survival variation within the genus are coronaviruses OC43 and 229E. After drying, coronavirus 229E infectivity was detectable after 3 h on various surfaces (aluminium, sterile latex surgical gloves and sterile sponges), whilst coronavirus OC43 survived 1 h or less (Sizun et al. 2000).
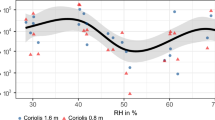
Relative Humidity
Effect of relative humidity (RH) varies within virus type. It is believed that the survival of enveloped viruses on inanimate surfaces is better when RH levels are below 50%. On the other hand, RH levels higher than 80% are considered to be more beneficial to the survival of non-enveloped viruses. In general, viruses with higher lipid content tend to be more persistent at a lower RH, whilst viruses with lesser or no lipid content are more stable at a higher RH (Assar and Block 2000; Moce-Llivina et al. 2006). However, there are exceptions.
Studies have shown that HAV is able to survive better at low levels of RH, which is in contrast to the behaviour of other enteroviruses (Mbithi et al. 1991; Stine et al. 2005). When its persistence in high and medium RH (85.7–90.3% and 45.1–48.4%) was compared, HAV survived longer on lettuce in dry conditions. Based on the calculated inactivation rates, a 99.9% reduction in HAV could take 822 days in pre-harvest conditions of contaminated vegetables (Stine et al. 2005). In contrast, Abad et al. (1994) found that survival of HAV was enhanced at high RH.
Data regarding rotavirus survival was determined to be contradictory. Moe and Shirley (1982) showed that a field strain of human rotavirus could survive longer when RH was kept either low or high than when RH has medium range. Sattar et al. (1986) reported that human rotavirus survived for a shorter period of time at high RH. Abad et al. (1994) also observed that human rotavirus and poliovirus exhibited greater persistence at high RH on non-porous material. The survival of adenovirus was not affected by RH. At 5°C RH had a little effect on survival time of norovirus, but its survival was longest at 20°C and low RH.
Sattar et al. (1987) investigated rhinovirus on surfaces. Humidity was used as a variable factor. The study found that rhinovirus exhibits optimum survival at 50% RH.
Temperature
However the degree of virus survival on surfaces is affected by temperature, it depends also on the virus type and RH. Viral particles are able to persist from days to months over a range of temperatures in the environment, and being preserved by refrigeration or freezing (Cliver 2009).
Temperature is one of the most important of determining norovirus survival in the environment. Recent studies indicate that noroviruses can survive for a prolonged period of time at a low temperature and can be transmitted to a susceptible population via different environmental media including surfaces (Mattison et al. 2007). Doultree et al. (1999) found that FCV dried onto glass and stored at 4°C displays a 4.75 log reduction over 56 days. FCV survival was lower at room temperature, but still prolonged. The number of infectious FCV declined to undetectable levels by 21–28 days. FCV was not detected at 37°C after 1 day. Comparative analyses indicated that FCV survival was greater at 4°C than at room temperature. Therefore, outbreaks caused by noroviruses are much more prevalent in the winter than in the summertime (Doultree et al. 1999; Mattison et al. 2007).
Rotavirus particles are able to survive storage in ambient tropical temperatures for more than 2 months (Fischer et al. 2002). Moe and Shirley (1982) reported that rotavirus infectivity decreases more rapidly under all RH at 37°C than at 4 or 20°C. According to a study done by Sattar et al. (1986), rotaviruses can persist longer at a lower temperature (4°C) and RH (25–50%), with approximately 10% infectious virus remaining after 10 days, in comparison to less than 1% after 2 days at 22°C and 85% RH. Abad et al. (2001) investigated the survival of an astrovirus at 4 and 20°C with a high RH (90 ± 5%). At 4°C, the virus was able to persist for 60 days desiccated on non-porous material and for 90 days on porous material. Faster decay was observed at 20°C. Short-term survival of astrovirus was compared to that observed for other enteric viruses significant for health, such as rotavirus, adenovirus, poliovirus and HAV. Overall, astrovirus persisted better than poliovirus and adenovirus, although they exhibited a shorter survival than the rotavirus and HAV.
Amongst other factors, the effect of freezing on enteric viruses in berries and herbs was tested by Butot et al. (2008). This study revealed that freezing does not significantly reduce the viability of norovirus, HAV and rotavirus. Only infectivity of FCV on strawberries can be decreased. Freezing for 3 months had a limited effect on HAV and rotavirus in all tested food products. A higher decay rate was observed in frozen raspberries and strawberries contaminated with FCV due to the acidic pH (Butot et al. 2008). No reduction of MNV-1 PFUs was observed on frozen onions or spinach during storage for 6 months (Baert et al. 2008). Kurdziel et al. (2001) reported a reduction of <2 log10 units of poliovirus on frozen strawberries after 15 days of storage. So far, no data about survival of other viruses during freezing are available.
Sunlight and UV
Ultraviolet radiation is the crucial virucidal agent, which primary targets viral nucleic acid but also modifies capsid proteins. Virus resistance to UV exposure also appears to vary according to virus type. Viruses with single-stranded nucleic acid (ssDNA and ssRNA) are more susceptible to UV inactivation than viruses with double-stranded nucleic acid: dsDNA and dsRNA (Gerba et al. 2002; Hijnen et al. 2006; Tseng and Li 2007).
According to Hijnen et al. (2006), adenoviruses are classified as the most resistant virus type to UV. The obtained k-values, which characterise UV-sensitivity of the microorganism, are similar for FCV, rotavirus, poliovirus and Coxsackievirus. HAV is more sensitive then the above-mentioned viruses. The correlation between low and high solar virucidal radiation and high and low influenza prevalence suggest that inactivation of viruses in the environment by solar UV radiation has a stronger effect than expected and can play a role in seasonal occurrence, e.g. influenza pandemics (Sagripanti and Lytle 2007).
Duizer et al. (2004) exposed surrogate caliciviruses (enteric canine calicivirus and respiratory FCV) to UV-B radiation as a factor affecting environmental survival. Results were comparable to enteroviruses (Gerba et al. 2002), less effective than for vegetative bacteria, but more effective than for phage MS2 (Husman et al. 2004), adenoviruses (Gerba et al. 2002; Nwachuku et al. 2005), and Baccilus subtilis spores (Chang et al. 1985). Parallel analysis of four RNA virus models (poliovirus 1, phage MS2, phage GA and phage Qβ) showed that the least resistant virus to UV radiation was poliovirus 1. Qβ phage had intermediate sensitivity, whilst MS2 and GA phages were the most resistant. The rate of RNA degradation increased linearly with increasing fragment size, except viruses with a similar size of genome (poliovirus 1 and MS2). Based on these results, viral resistance to UV depends especially on fragment size of viral nucleic acid. Nevertheless, it also shows that the viral capsid structure has an important protective role against UV radiation (Simonet and Gantzer 2006).
Type of Surface
Several studies have compared the survival of different types of viruses on porous and non-porous surfaces. The majority of viruses remain viable for a longer period of time on non-porous materials, although there are exceptions (Abad et al. 1994; Boone and Gerba 2007; Lamhoujeb et al. 2009; Tiwari et al. 2006); e.g. higher persistence of poliovirus and adenovirus was observed on porous materials (paper and cotton cloth) compared to non-porous materials: aluminium, china, glazed tile, latex, and polystyrene (Abad et al. 1994). The enteric viruses reveal exhibited inactivation rates (at least 2 logs lower) than respiratory viruses, with the exception of adenovirus and influenza virus (Boone and Gerba 2007). Tiwari et al. (2006) studied survival of avian metapneumovirus and avian influenza virus on 12 different porous and non-porous materials. Both viruses persisted longer (up to 6 days) on non-porous surfaces than on porous ones.
Survival times for enteric viruses have been determined on a range of different fruit and vegetable commodities (Seymour and Appleton 2001). Mattison et al. (2007) suggested that smooth surfaces, such a lettuce leaf, might provide less protection to the virus than coarse surfaces like ham has. Results of other studies indicated that on plant surfaces, viruses are exposed to potentially toxic compounds, such as phenols, ethanol, and acetaldehyde, which could accelerate the inactivation process (Lamhoujeb et al. 2009).
Some specific chemical surfaces (e.g. heavy metals) are virucidal. Influenza virus particles (2 × 106) were inoculated onto cooper and stainless steel surfaces in a study by Noyce et al. (2007). After incubation for 24 h on stainless steel, 500,000 virus particles were still infectious in comparison with cooper, where only 500 viral particles were active after incubation for 6 h. Other recent studies also suggest the antimicrobial properties of cooper-based surfaces (Barker et al. 2004; Faundez et al. 2004; Iriarte et al. 2007; Noyce et al. 2006, 2007). It has been reported that aluminium also has virucidal activity. Adenovirus, poliovirus and the B40-8 phage persist for a shorter time on aluminium than on other non-porous material (Abad et al. 1994; Thurman and Gerba 1988).
Adsorption State and Organic Matter
The extent and state of virus adsorption on surfaces has an important influence on virus survival. Studies have shown that the survival of viruses is increased with increased adsorption to the surfaces and that immobilized (adsorbed) viral particles most often keep their infectious potential after desorption. Interactions that take place between viruses and surfaces are determined by their characteristics and involve electrostatic, hydrophobic interactions, and/or ionic strength (Hurst et al. 1980; Lacroix-Gueu et al. 2005). Vega et al. (2008) compared the relative contributions of these interactions with the nonspecific attachment of echovirus 11, FCV, MS2, and φX174 to butterhead lettuce. The results imply that electrostatic forces play a major role in controlling virus adsorption to lettuce.
Many viruses can be stabilized and protected by dissolved, colloidal and solid organic matter; including faecal and humic material. Organic matter has a low isoelectric point, and thus carries a negative surface charge at most naturally occurring pH levels (Boone and Gerba 2007). Kiseleva (1971) reported that strains of poliomyelitis virus, echovirus and coxsackievirus remained infectious from two to more than 12 days on the surface of substances used in various household objects. The greater survival was observed, if the inoculum also contained coliform bacteria, proteins, fats and dust particles, but no precise results or experimental details were given (Kiseleva 1971 as quoted by Rzezutka and Cook 2004). Lee et al. (2008) found that murine norovirus is more stable in a stool suspension than on different types of surfaces. After 30 days of incubation at 18°C, there was a 2.7-log10 reduction in the stool suspension, compared to the maximum reduction of 5.3-log10 on a gauze or diaper surface. A study by Abad et al. (1994) showed that on non-porous surfaces, poliovirus and adenovirus persist better in the presence of faeces. However, on porous fomites the presence of faecal material has a negative influence on the survival of these viruses. HAV and human rotavirus persistence is not affected by the presence of faeces.
pH and Presence of Salts
In general, pH has a minimal effect on virus survival in an indoor environment. Hurst et al. (1980) measured the effects of several environmental conditions on virus persistence in soil. They found that the temperature and virus adsorption to soil is more important for virus survival than the effect of pH. Enteric viruses are able to survive severe conditions in the gastrointestinal tract, such as low pH in stomach or high bile concentration. They are generally most stable near pH 7, but prefer low pH’s (3–5) rather than alkaline pH’s (9–12). It was shown that noroviruses are able to persist at pH 2.7 and room temperature more than 3 h (Duizer et al. 2004). As the surface charge of viral particles varies depending on the pH, disruption of electrostatic interactions between viral particles and environmental surfaces commonly consists of changing the pH, and thus affect viral persistence in the environment (Gerba 1984).
The viral adsorption to the surfaces can be influenced by ionic strengths; therefore, salts are commonly used to favour the attachment of viruses to different types of surfaces. Theoretically, adsorption of viral particles is better in high ionic strength. Enteric viruses are destabilized and inactivated by water lacking salt ions, e.g. Mg2+. On the contrary, increased concentrations of salts (e.g. NaCl) are antiviral for many viruses.
Interaction of Pathogenic Viruses with Other Microorganisms During their Presence on Surfaces
Data about the influence of other microorganisms on virus survival are contradictory. Virus survival may increase or decrease with the number of microbes present on the surface. Bacteria or microscopic fungi are able to attack and inactivate infectious viral particles. Some bacteria can produce low molecular weight substances that apparently inactivate viruses. Others appear to use viral capsid proteins as substrates (Deng and Cliver 1995a, b; Cliver 2009; Herrmann et al. 1974). By contrast increasing amount of microbes can protect viruses from desiccation and disinfection. Interactions of pathogenic viruses with bacterial biofilms have been reported (Lacroix-Gueu et al. 2005; Skraber et al. 2005). As biofilms can form on a wide spectra of surfaces (Davey and O’toole 2000), their influence on virus survival is also discussed in this review.
Negative Influence of Other Microorganisms on Virus Survival
One proposed mechanism of viral loss in the environment is inactivation by the direct or indirect action of microorganisms. Environmental isolates of bacteria with antiviral ability have been found on several occasions. These microbes are able to produce metabolites, which adversely affect viral particles, or can use the viral capsid as a nutrient source (Deng and Cliver 1995a, b; Ward 1982). The inactivation of viruses by bacterial cultures is temperature dependent. The lower the temperature of the mixed waste, the longer the virus is able to persist. Moreover temperature could strongly influence microbial activity, and thus influence viral persistence (Deng and Cliver 1992).
Ward (1982) investigated the influence of mixed-liquor suspended solids (MLSS) of inactivated sludge on a poliovirus 1 survival. The first experiment was conducted in order to determine the effect of MLSS on the recovery of poliovirus after a different period of time. The second experiment was designed to find out the role of different MLSS components in virus loss. Results of these studies indicate that MLSS contain a component(s) which can inactivate poliovirus 1. These components were pelleted during centrifugation, destroyed by autoclaving, and removed by filtration. Consecutively, residual activity of an MLSS supernatant fraction was also studied to confirm the absence of antiviral activity in non-living heat-sensitive material in the MLSS. Subsequent increasing activity of this supernatant, coupled with the previous results, strongly indicates the antiviral activity of some microbial species. Deng and Cliver (1992) demonstrated the antiviral effect of several bacterial cultures from swine manure slurry and mixed septic tank effluent. These cultures were identified as Micrococcus luteus, Staphylococcus epidermidis, Bacillus sp. and Streptococcus sanguis group. A comparison of poliovirus 1 inactivation in raw mixed waste, autoclaved mixed waste, and bacterium-free filtrate of raw mixed waste demonstrated that virus inactivation is related, at least in part, to microbial activity in similar environmental conditions. Inhibition of poliovirus 1 inactivation by protease inhibitors suggested that antiviral activity of mixed waste was partially due to proteolytic enzymes produced by bacteria in wastes.
Bacteria may also produce substances that inactivate viruses by processes other than enzymatic ones, e.g. Pseudomonas aeruginosa can produce substances with molecular weights below 500 Da which appear to inactivate viral particles. Substances with such low molecular weights cannot act enzymatically and they are referred to as virolytic substances (Cliver and Hermann 1972; Deng and Cliver 1992). Deng and Cliver (1995a) studied the role of the microbial activity of animal wastes in inactivation of HAV. Ten out of 31 bacterial isolates were able to efficiently inactivate HAV. The inactivation capacity of four of the nine culture filtrates was significantly reduced by incubation with selected protease inhibitors before the virus was added. These inhibitors did not affect the activities of the other five culture filtrates. Fractions prepared by ultrafiltration (nominal molecular weights <1,000 Da) from two of these cultures inactivated HAV suggested that their mode of action was not enzymatic.
Viruses Within Biofilms
From a public health point of view, biofilms have been already regarded as a common cause of bacterial infections. It has also been hypothesised that produced exopolymeric substances (EPS) may protect biofilms from viruses, especially phage penetration (Sutherland et al. 2004). Recent studies have revealed that, even in the absence of specific enzymatic reactions, viral particles are able to penetrate inside the EPS structure of mucoid biofilms. After penetration inside the polymeric matrix, the viruses may take advantage from the specific ‘biofilm lifestyle’, and benefit from protection against environmental stress, such as desiccation or other actions of antimicrobial agents. Moreover during biofilms erosion or sloughing, protected immobilised viral particles may be released in the environment, and then contact their target host commencing the viral infectious cycle (Briandet et al. 2008; Helmi et al. 2008; Lacroix-Gueu et al. 2005; Lehtola et al. 2007; Quignon et al. 1997). Viral attachment rates to biofilms vary greatly and may depend on many factors such as the biofilm or viral characteristics (size, shape, isoelectric point), and concentration of viral particles (Helmi et al. 2008).
Helmi et al. (2008) reported that poliovirus 1 adsorption was higher in wastewater biofilm than in drinking water biofilm. Infectious viral particles were detected in the drinking water biofilm for up to 6 days after inoculation, whilst the viral genome was still detectable at day 34. Hock and Botzenhart (2002, 2003) injected phages MS2, φX174 and poliovirus 1 at comparable concentrations into a laboratory reactor containing approximately 100 ml of drinking water. After the contact time of 1 h, concentrations of 0.04, 0.13 and 0.27% were recovered from the biofilm. MS2 showed less adsorption to the biofilm than φX174 and poliovirus 1 (Hock and Botzenhart 2002; Hock and Botzenhart 2003 as quoted by Skraber et al. 2005). These results can be explained by the fact that MS2 is more negatively charged than other tested viruses. In contrast, Storey and Ashbolt (2003a, b) estimated that the attachment rates of MS2 and φX174 were similar: 1% of the initial input. The efficiency of viral recovery was predetermined for MS2, but not for φX174 or poliovirus in the mentioned studies. Due to this fact, differences or similarities between apparent attachments can be explained by variation between efficiencies of viral recovery.
Results published by Quignon et al. (1997) showed that water biofilm can protect viruses form inactivation. This hypothesis is supported by the study of Storey and Ashbolt (2001). Phages MS2 and B40-8 were recovered from biofilm in the presence of the average concentration of 0.2 mg free chlorine/l during a 30-day period. In comparison, Duran et al. (2003) reported that phages MS2 and B40-8 showed 3.2 and 1.7 log10-units reduction after only ten min in groundwater containing 0.5 mg free chlorine/l. Storey and Ashbolt (2003b) compared the inactivation of two phages (B40-8 and MS2) within biofilms. Results indicated that the subpopulation of approximately 0.01% of phages had the potential to persist over 100 days for B40-8 and almost 10 times longer for MS2 in the presence of free chlorine. The level of viral protection may depend on parameters such as the composition, thickness, or structure of biofilms.
Various studies have suggested that biofilms may trap and accumulate virus-sized particles and produce a potential reservoir of human or bacterial pathogens. In natural environments, biofilms are mixed microbial cultures normally consisting of predominantly prokaryotes with some eukaryotes (Sutherland et al. 2004). Although virus attachments to biofilms have been observed experimentally and contamination of natural biofilms with pathogenic viruses can be very low, biofilms should be considered as a protective reservoir for pathogenic viruses, and could be responsible for numerous persistent viral infections (Lacroix-Gueu et al. 2005).
Specific Antiviral Chemicals
Due to the importance in preventing the spread of viruses in healthcare settings and food establishments, the effect of chemical disinfectants on contaminated surfaces has been extensively studied. Some studies demonstrated that suspension tests performed with the same disinfectants showed different virus inactivation rates, thus failing to provide a reliable indication of the extent of virus disinfection on surfaces. The activity of disinfectants is strongly related to RH and temperature (Casella and Schmidt-Lorenz 1989; Theilen et al. 1987).
Viruses without envelope are more resistant to desiccation. Biocides that have activity against both enveloped and non-enveloped viruses include chlorine- and iodine-releasing agents, peracids and ozone. Their effectiveness depends on the nature of the virus, the surface carrier, the presence of interfering substances such as organic soil or hard water salts, and contact time. However, some cleaning products or disinfectants are ineffective against viruses, and can result in viral spread or cross-contamination of surfaces (Boone and Gerba 2007).
Chemical disinfection on food contact surfaces and rising food items with sanitizers is generally relied on prevention and control food-borne outbreaks. Numerous authors have reported on the efficacy of disinfectants for the inactivation of cultivable viruses using standard suspension tests, but data for gastroenteritis viruses and HAV are lacking (Seymour and Appleton 2001). This is partially due to the lack of methods for propagation of these viruses in vitro (Gulati et al. 2001).
Detection of Viruses on Surfaces
Sufficient detection of infectious viral particles in the environment is affected by several obstacles such as: virus size, the large variability amongst and within viral genera, the low concentration, the presence of substances which can interfere with analysis procedures, the limits of detection of proposed techniques, and absence of reliable controls. Therefore, appropriate sampling and sensitive detection methods are necessary to help better understanding of viral transmission routes.
It is obvious that physical properties of the surface could further reduce recovery of viral particles form surfaces. Viruses can be trapped within the matrix, especially if the surface is porous (Scherer et al. 2009). Therefore, sampling and detection methods must be sensitive enough to detect low levels of viral particles. Cell culture methods are sensitive and can determine infectivity of isolated viral particles, but these methods are time consuming. Moreover, there is a problem of interference amongst viruses, which are able to grow on the same cell line (e.g. reovirus and enterovirus) or can allow chronic infections without a visible cytopathic effect (e.g. HAV or reovirus). Even if this cytopathic effect is evident, the identification of isolated agents requires additional techniques for confirmation of virus strain or type. Finally, cultivation methods cannot be used for non-cell culture viruses (e.g. HEV). For enumeration of infectious viruses it is necessary to use cell culture in a quantitative format, e.g. plaque assay. The number of infectious viruses remaining in the sample is compared with the number which was introduced, and a statistical procedure can be performed to calculate any degree of decline.
Molecular methods are an alternative which can be used for virus detection. PCR and NASBA techniques represent high sensitive and specific methods. They can be used for all types of viruses, require a short time for execution, can determine different agents in the same sample, and allow identification of non-cultivable virus. Nevertheless, analyses may be hindered by inhibitory substances present in the environment, so there is a risk of occurrence of false negative results. Due to this fact it is necessary to implement internal amplification controls. Moreover viruses detected by these techniques are not necessary infectious. Molecular methods can reveal nucleic acid originating from partially denatured viral particles. Thus, viral capsid is still capable of protecting nucleic acid, but the viral particle is not infectious. Therefore, the combination of molecular techniques and cell culture methods should be used for the detection of viruses (Cliver 2009; Cook 2003).
Conclusion
In conclusion, there is strong evidence to suggest that transmission of viruses via contaminated surfaces is a significant factor contributing to the spread of disease. Virological monitoring of surfaces can be very useful in risk analysis to identify ways of viruses spreading, to monitor environmental pollution, and thus assess the risk of infection. Moreover detection of viral contamination of the environment allows molecular epidemiologic and phylogenetic data for virus surveillance and circulation.
References
Abad, F. X., Pinto, R. M., & Bosch, A. (1994). Survival of enteric viruses on environmental fomites. Applied and Environmental Microbiology, 60, 3704–3710.
Abad, F. X., Villena, C., Guix, S., Caballero, S., Pinto, R. M., & Bosch, A. (2001). Potential role of fomites in the vehicular transmission of human astroviruses. Applied and Environmental Microbiology, 67, 3904–3907.
Ansari, S. A., Sattar, S. A., Springthorpe, V. S., Wells, G. A., & Tostowaryk, W. (1988). Rotavirus survival on human hands and transfer of infectious virus to animate and nonporous inanimate surfaces. Journal of Clinical Microbiology, 26, 1513–1518.
Assar, S. K., & Block, S. S. (2000). Survival of microorganisms in the environment. In S. S. Block (Ed.), Disinfection, sterilization, and preservation. Philadelphia: Lippinkott-Williams.
Baert, L., Uyttendaele, M., Vermeersch, M., Van Coillie, E., & Debeverei, J. (2008). Survival and transfer of murine norovirus 1, a surrogate for human noroviruses, during the production process of deep-frozen onions and spinach. Journal of Food Protection, 71, 1590–1597.
Bajolet, O., & Chippaux-Hyppolite, C. (1998). Rotaviruses and other diarrheal viruses. Bulletin de la Societe de Pathologie Exotique, 91, 432–437.
Barker, J., Stevens, D., & Bloomfield, S. F. (2001). Spread and prevention of some common viral infections in community facilities and domestic homes. Journal of Applied Microbiology, 91, 7–21.
Barker, J., Vipond, I. B., & Bloomfield, S. F. (2004). Effects of cleaning and disinfection in reducing the spread of norovirus contamination via environmental surfaces. Journal of Hospital Infection, 58, 42–49.
Bidawid, S., Farber, J. M., & Sattar, S. A. (2000). Contamination of foods by food handlers: Experiments on hepatitis A virus transfer to food and its interruption. Applied and Environmental Microbiology, 66, 2759–2763.
Boone, S. A., & Gerba, C. P. (2007). Significance of foraites in the spread of respiratory and enteric viral disease. Applied and Environmental Microbiology, 73, 1687–1696.
Brady, M. T., Evans, J., & Cuartas, J. (1990). Survival and disinfection of parainfluenza viruses on environmental surfaces. American Journal of Infection Control, 18, 18–23.
Briandet, R., Lacroix-Gueu, P., Renault, M., Lecart, S., Meylheuc, T., Bidnenko, E., et al. (2008). Fluorescence correlation spectroscopy to study diffusion and reaction of bacteriophages inside biofilms. Applied and Environmental Microbiology, 74, 2135–2143.
Butot, S., Putallaz, T., & Sanchez, G. (2008). Effects of sanitation, freezing and frozen storage on enteric viruses in berries and herbs. International Journal of Food Microbiology, 126, 30–35.
Carter, M. J. (2005). Enterically infecting viruses: pathogenicity, transmission and significance for food and waterborne infection. Journal of Applied Microbiology, 98, 1354–1380.
Casella, M. L., & Schmidt-Lorenz, W. (1989). Disinfection with gaseous formaldehyde. Third Part: bactericidal and sporicidal effectiveness of gaseous formaldehyde and level of residues in dependence on concentration, temperature and relative humidity. International Journal of Hygiene and Environmental Medicine, 188(6), 533–549.
Chang, J. C. H., Ossoff, S. F., Lobe, D. C., Dorfman, M. H., Dumais, C. M., Qualls, R. G., et al. (1985). UV inactivation of pathogenic and indicator microorganisms. Applied and Environmental Microbiology, 49, 1361–1365.
Cliver, D. O. (2009). Control of viral contamination of food and environment. Food and Environmental Virology, 1, 3–9.
Cliver, D. O., & Hermann, J. E. (1972). Proteolytic and microbial inactivation of enteroviruses. Water Research, 6, 338–353.
Cook, N. (2003). The use of NASBA for the detection of microbial pathogens in food and environmental samples. Journal of Microbiological Methods, 53, 165–174.
Croci, L., De Medici, D., Scalfaro, C., Fiore, A., & Toti, L. (2002). The survival of hepatitis A virus in fresh produce. International Journal of Food Microbiology, 73, 29–34.
Davey, M. E., & O’toole, G. A. (2000). Microbial biofilms: from ecology to molecular genetics. Microbiology and Molecular Biology Reviews, 64, 847–867.
Deng, M. Y., & Cliver, D. O. (1992). Inactivation of poliovirus type-1 in mixed human and swine wastes and by bacteria from swine manure. Applied and Environmental Microbiology, 58, 2016–2021.
Deng, M. Y., & Cliver, D. O. (1995a). Antiviral effects of bacteria isolated from manure. Microbial Ecology, 30, 43–54.
Deng, M. Y., & Cliver, D. O. (1995b). Persistence of inoculated hepatitis-A virus in mixed human and animal wastes. Applied and Environmental Microbiology, 61, 87–91.
Doultree, J. C., Druce, J. D., Birch, C. J., Bowden, D. S., & Marshall, J. A. (1999). Inactivation of feline calicivirus, a Norwalk virus surrogate. Journal of Hospital Infection, 41, 51–57.
Duizer, E., Bijkerk, P., Rockx, B., de Groot, A., Twisk, F., & Koopmans, M. (2004). Inactivation of caliciviruses. Applied and Environmental Microbiology, 70, 4538–4543.
Duran, A. E., Muniesa, M., Moce-Llivina, L., Campos, C., Jofre, J., & Lucena, F. (2003). Usefulness of different groups of bacteriophages as model micro-organisms for evaluating chlorination. Journal of Applied Microbiology, 95, 29–37.
Faundez, G., Troncoso, M., Navarrete, P., & Figueroa, G. (2004). Antimicrobial activity of copper surfaces against suspensions of Salmonella enterica and Campylobacter jejuni. BMC Microbiology, 4, 19.
Fischer, T. K., Steinsland, H., & Valentiner-Branth, P. (2002). Rotavirus particles can survive storage in ambient tropical temperatures for more than 2 months. Journal of Clinical Microbiology, 40, 4763–4764.
Gerba, C. P. (1984). Applied and theoretical aspects of virus adsorption to surfaces. Advances in Applied Microbiology, 30, 133–168.
Gerba, C. P., Gramos, D. M., & Nwachuku, N. (2002). Comparative inactivation of enteroviruses and adenovirus 2 by UV light. Applied and Environmental Microbiology, 68, 5167–5169.
Goldmann, D. A. (2000). Transmission of viral respiratory infections in the home. Pediatric Infectious Disease Journal, 19, S97–S102.
Goodgame, R. (2006). Norovirus gastroenteritis. Current Gastroenterology Reports, 8, 401–408.
Gulati, B. R., Allwood, P. B., Hedberg, C. W., & Goyal, S. M. (2001). Efficacy of commonly used disinfectants for the inactivation of calicivirus on strawberry, lettuce, and a food-contact surface. Journal of Food Protection, 64, 1430–1434.
Gwaltney, J. M., & Hendley, J. O. (1982). Transmission of experimental rhinovirus infection by contaminated surfaces. American Journal of Epidemiology, 116, 828–833.
Hall, C. B., Douglas, R. G., & Geiman, J. M. (1980). Possible transmission by fomites of respiratory syncytial virus. Journal of Infectious Diseases, 141, 98–102.
Helmi, K., Skraber, S., Gantzer, C., Willame, R., Hoffmann, L., & Cauchie, H. M. (2008). Interactions of Cryptosporidium parvum, Giardia lamblia, vaccinal poliovirus type 1, and bacteriophages phi X174 and MS2 with a drinking water biofilm and a wastewater biofilm. Applied and Environmental Microbiology, 74, 2079–2088.
Hendley, J. O., Wenzel, R. P., & Gwaltney, J. M. (1973). Transmission of rhinovirus colds by self-inoculation. New England Journal of Medicine, 288, 1361–1364.
Henrickson, K. J., Hoover, S., Kehl, K. S., & Hua, W. M. (2004). National disease burden of respiratory viruses detected in children by polymerase chain reaction. Pediatric Infectious Disease Journal, 23, S11–S18.
Herrmann, J. E., Kostenbader, K. D., Jr, & Cliver, D. O. (1974). Persistence of enteroviruses in lake water. Applied Microbiology, 28, 895–896.
Hewitt, J., & Greening, G. E. (2004). Survival and persistence of norovirus, hepatitis A virus, and feline calicivirus in marinated mussels. Journal of Food Protection, 67, 1743–1750.
Hijnen, W. A. M., Beerendonk, E. F., & Medema, G. J. (2006). Inactivation credit of UV radiation for viruses, bacteria and protozoan (oo)cysts in water: A review. Water Research, 40, 3–22.
Hock, C., & Botzenhart, K. (2002). Detection of enteric viruses in biofilms of the drinking water system. Melbourne: 3rd IWA World Water Congress.
Hock, C., & Botzenhart, K. (2003). Auftreten von Obligat und Fakultative Pathogenen Organismen in Trinkwasser-Biofilmen: Viren. In H.-C. Fleming (Ed.) Erfassung des Wachstums und des Kontaminationspotenzials von Biofilmen in der Verteilung von Trinkwasser (pp. 160–185). Mülheim an der Ruhr: Berichte aus dem IWW Rheinisch-Westfälisches Institut für Wasserforschung gemeinnützige GmbH, band 36.
Howie, R., Alfa, M. J., & Coombs, K. (2008). Survival of enveloped and non-enveloped viruses on surfaces compared with other micro-organisms and impact of suboptimal disinfectant exposure. Journal of Hospital Infection, 69, 368–376.
Hurst, C. J., Gerba, C. P., & Cech, I. (1980). Effects of environmental variables and soil characteristics on virus survival in soil. Applied and Environmental Microbiology, 40, 1067–1079.
Husman, A. M. D., Bijkerk, P., Lodder, W., van den Berg, H., Pribil, W., Cabaj, A., et al. (2004). Calicivirus inactivation by nonionizing (253.7-nanometer-wavelength [UV]) and ionizing (Gamma) radiation. Applied and Environmental Microbiology, 70, 5089–5093.
Iriarte, F. B., Balogh, B., Momol, M. T., Smith, L. M., Wilson, M., & Jones, J. B. (2007). Factors affecting survival of bacteriophage on tomato leaf surfaces. Applied and Environmental Microbiology, 73, 1704–1711.
Kesson, A. M. (2007). Respiratory virus infections. Paediatric Respiratory Reviews, 8, 240–248.
Kiseleva, L. F. (1971). Survival of poliomyelitis, ECHO and coxsackie viruses in some food products. Voprosy Pitaniia, 30, 58–61.
Koopmans, M., & Duizer, E. (2004). Foodborne viruses: an emerging problem. International Journal of Food Microbiology, 90, 23–41.
Kurdziel, A. S., Wilkinson, N., Langton, S., & Cook, N. (2001). Survival of poliovirus on soft fruit and salad vegetables. Journal of Food Protection, 64, 706–709.
Lacroix-Gueu, P., Briandet, R., Leveque-Fort, S., Bellon-Fontaine, M. N., & Fontaine-Aupart, M. P. (2005). In situ measurements of viral particles diffusion inside mucoid biofilms. Comptes Rendus Biologies, 328, 1065–1072.
Lamhoujeb, S., Fliss, I., Ngazoa, S. E., & Jean, J. (2009). Molecular study of the persistence of infectious human norovirus on food-contact surfaces. Food and Environmental Virology, 1, 51–56.
Lee, J., Zoh, K., & Ko, G. (2008). Inactivation and UV disinfection of murine norovirus with TiO2 under various environmental conditions. Applied and Environmental Microbiology, 74, 2111–2117.
Lehtola, M. J., Torvinen, E., Kusnetsov, J., Pitkanen, T., Maunula, L., von Bonsdorff, C. H., et al. (2007). Survival of Mycobacterium avium, Legionella pneumophila, Escherichia coli, and caliciviruses in drinking water-associated biofilms grown under high-shear turbulent flow. Applied and Environmental Microbiology, 73, 2854–2859.
Leung, A. K. C., Kellner, J. D., & Davies, H. D. (2005). Rotavirus gastroenteritis. Advances in Therapy, 22, 476–487.
Marks, P. J., Vipond, I. B., Carlisle, D., Deakin, D., Fey, R. E., & Caul, E. O. (2000). Evidence for airborne transmission of Norwalk-like virus (NLV) in a hotel restaurant. Epidemiology and Infection, 124, 481–487.
Mattison, K., Karthikeyan, K., Abebe, M., Malik, N., Sattar, S. A., Farber, J. M., et al. (2007). Survival of calicivirus in foods and on surfaces: Experiments with feline calicivirus as a surrogate for norovirus. Journal of Food Protection, 70, 500–503.
Mbithi, J. N., Springthorpe, V. S., Boulet, J. R., & Sattar, S. A. (1992). Survival of hepatitis-A virus on human hands and its transfer on contact with animate and inanimate surfaces. Journal of Clinical Microbiology, 30, 757–763.
Mbithi, J. N., Springthorpe, V. S., & Sattar, S. A. (1991). Effect of relative-humidity and air-temperature on survival of hepatitis-A virus on environmental surfaces. Applied and Environmental Microbiology, 57, 1394–1399.
Moce-Llivina, L., Papageorgiou, G. T., & Jofre, J. (2006). A membrane-based quantitative carrier test to assess the virucidal activity of disinfectants and persistence of viruses on porous fomites. Journal of Virological Methods, 135, 49–55.
Moe, K., & Shirley, J. A. (1982). The effects of relative-humidity and temperature on the survival of human rotavirus in feces. Archives of Virology, 72, 179–186.
Noyce, J. O., Michels, H., & Keevil, C. W. (2006). Potential use of copper surfaces to reduce survival of epidemic meticillin-resistant Staphylococcus aureus in the healthcare environment. Journal of Hospital Infection, 63, 289–297.
Noyce, J. O., Michels, H., & Keevil, C. W. (2007). Inactivation of influenza A virus on copper versus stainless steel surfaces. Applied and Environmental Microbiology, 73, 2748–2750.
Nwachuku, N., Gerba, C. P., Oswald, A., & Mashadi, F. D. (2005). Comparative inactivation of adenovirus serotypes by UV light disinfection. Applied and Environmental Microbiology, 71, 5633–5636.
Quignon, F., Sardin, M., Kiene, L., & Schwartzbrod, L. (1997). Poliovirus-1 inactivation and interaction with biofilm: A pilot-scale study. Applied and Environmental Microbiology, 63, 978–982.
Rzezutka, A., & Cook, N. (2004). Survival of human enteric viruses in the environment and food. FEMS Microbiology Reviews, 28, 441–453.
Sagripanti, J. L., & Lytle, C. D. (2007). Inactivation of influenza virus by solar radiation. Photochemistry and Photobiology, 83, 1278–1282.
Sattar, S. A., Karim, Y. G., Springthorpe, V. S., & Johnson-Lussenburg, C. M. (1987). Survival of human rhinovirus type-14 dried onto nonporous inanimate surfaces—effect of relative-humidity and suspending medium. Canadian Journal of Microbiology, 33, 802–806.
Sattar, S. A., Lloydevans, N., Springthorpe, V. S., & Nair, R. C. (1986). Institutional outbreaks of rotavirus diarrhoea—potential role of fomites and environmental surfaces as vehicles for virus transmission. Journal of Hygiene, 96, 277–289.
Scherer, K., Mäde, D., Ellerbroek, L., Schulenburg, J., Johne, R., & Klein, G. (2009). Application of a swab sampling method for the detection of noroviruses and rotaviruses on artificially contaminated food and environmental surfaces. Food and Environmental Virology, 1, 42–49.
Seymour, I. J., & Appleton, H. (2001). Foodborne viruses and fresh produce. Journal of Applied Microbiology, 91, 759–773.
Simonet, J., & Gantzer, C. (2006). Inactivation of poliovirus 1 and F-specific RNA phages and degradation of their genomes by UV irradiation at 254 nanometres. Applied and Environmental Microbiology, 72, 7671–7677.
Sizun, J., Yu, M. W. N., & Talbot, P. J. (2000). Survival of human coronaviruses 229E and OC43 in suspension and after drying on surfaces: a possible source of hospital-acquired infections. Journal of Hospital Infection, 46, 55–60.
Skraber, S., Schijven, J., Gantzer, C., & de Roda Husman, A. M. (2005). Pathogenic viruses in drinking-water biofilms: a public health risk? Biofilms, 2, 1–13.
Stine, S. W., Song, I., Choi, C. Y., & Gerba, C. P. (2005). Effect of relative humidity on preharvest survival of bacterial and viral pathogens on the surface of cantaloupe, lettuce, and bell peppers. Journal of Food Protection, 68, 1352–1358.
Storey, M. V., & Ashbolt, N. J. (2001). Persistence of two model enteric viruses (B40-8 and MS-2 bacteriophages) in water distribution pipe biofilms. Water Science and Technology, 43, 133–138.
Storey, M. V., & Ashbolt, N. J. (2003a). A risk model for enteric virus accumulation and release from recycled water distribution pipe biofilms. 3rd World Water Congress: Efficient Water Supply and Water Reuse, 3, 93–100.
Storey, M. V., & Ashbolt, N. J. (2003b). Enteric virions and microbial biofilms—a secondary source of public health concern? Water Science and Technology, 48, 97–104.
Sutherland, I. W., Hughes, K. A., Skillman, L. C., & Tait, K. (2004). The interaction of phage and biofilms. FEMS Microbiology Letters, 232, 1–6.
Theilen, U., Wilsberg, F. J., Bohm, R., & Strauch, D. (1987). Aerosol disinfection of bacterial spores. Zentralblatt für Bakteriologie, Mikrobiologie und Hygiene. 1. Abt. Originale B, Hygiene, 184(3–4), 229–252.
Thurman, R. B., & Gerba, C. P. (1988). Characterization of the effect of aluminium metal on poliovirus. Journal of Industrial Microbiology, 3, 33–38.
Tiwari, A., Patnayak, D. P., Chander, Y., Parsad, M., & Goyal, S. M. (2006). Survival of two avian respiratory viruses on porous and nonporous surfaces. Avian Diseases, 50, 284–287.
Todd, E. C., Greig, J. D., Bartleson, C. A., & Michaels, B. S. (2009). Outbreaks where food workers have been implicated in the spread of foodborne disease. Part 6. Transmission and survival of pathogens in the food processing and preparation environment. Journal of Food Protection, 72, 202–219.
Tseng, C. C., & Li, C. S. (2007). Inactivation of viruses on surfaces by ultraviolet germicidal irradiation. Journal of Occupational and Environmental Hygiene, 4, 400–405.
Vega, E., Garland, J., & Pillai, S. D. (2008). Electrostatic forces control nonspecific virus attachment to lettuce. Journal of Food Protection, 71, 522–529.
von Rheinbaben, F., Schunemann, S., Gross, T., & Wolff, M. H. (2000). Transmission of viruses via contact in a household setting: experiments using bacteriophage phi X174 as a model virus. Journal of Hospital Infection, 46, 61–66.
Ward, R. L. (1982). Evidence that microorganisms cause inactivation of viruses in activated-sludge. Applied and Environmental Microbiology, 43, 1221–1224.
Ward, R. L., Bernstein, D. I., Knowlton, D. R., Sherwood, J. R., Young, E. C., Cusack, T. M., et al. (1991). Prevention of surface-to-human transmission of rotaviruses by treatment with disinfectant spray. Journal of Clinical Microbiology, 29, 1991–1996.
Winther, B., Hayden, F. G., & Hendley, J. O. (2006). Picornavirus infections in children diagnosed by RT-PCR during longitudinal surveillance with weekly sampling: Association with symptomatic illness and effect of season. Journal of Medical Virology, 78, 644–650.
Winther, B., McCue, K., Ashe, K., Rubino, J. R., & Hendley, J. O. (2007). Environmental contamination with rhinovirus and transfer to fingers of healthy individuals by daily life activity. Journal of Medical Virology, 79, 1606–1610.
Wu, H. M., Fornek, M., Schwab, K. J., Chapin, A. R., Gibson, K., Schwab, E., et al. (2005). A norovirus outbreak at a long-term-care facility: The role of environmental surface contamination. Infection Control and Hospital Epidemiology, 26, 802–810.
Acknowledgments
This study was supported by Grants No. MZE0002716202 (Ministry of Agriculture of the Czech Republic), OC08045 (support of the Cost Action 929) and AdmireVet (Ministry of Education, Youth and Sports of the Czech Republic), Cost Action 929 ENVIRONET of Brussels, EC and the Italian National Institute of Occupational Safety and Prevention. The authors wish to thank Maria Vass (Scientific Editing Services, m_vass@hotmail.com) for grammatical corrections of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Vasickova, P., Pavlik, I., Verani, M. et al. Issues Concerning Survival of Viruses on Surfaces. Food Environ Virol 2, 24–34 (2010). https://doi.org/10.1007/s12560-010-9025-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12560-010-9025-6