Abstract
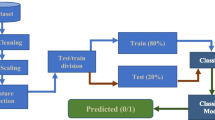
In clinical practice, plasma glucose concentrations in fasting and postprandial are measured to assess glucose metabolism and to diagnose diabetes. Plasma glucose and insulin concentrations in fasting and postprandial have been used to better characterize normal, prediabetic and diabetic conditions. In this paper, we seek to automatically recognize nine classes of metabolic conditions (three normal, three prediabetics, and three diabetics) by considering the age the patient and its fasting plasma glucose (FPG) and insulin (FPI) concentrations. Multinomial logistic regression (MLR), artificial neural network (ANN), support vector machine (SVM), decision tree (DT) and random forests (RF) were set for different attribute combinations (age, FPG and FPI). Accuracy, and macro-average and weighted-average measures of precision, recall and F1-score were employed to assess the performance of the classifiers. Accuracy and weighted-average of precision, recall and F1-score above 79% were obtained using an ANN and an RF with age, FPG and FPI as attributes. In terms of the weighted-average of F1, an ANN with FPG and FPI as attributes was the best classifier (weighted-average F1 = 81.50%). Age, FPG and FPI provided information to recognize the nine metabolic classes. Moreover, age helped to distinguish between two diabetic classes with overlapping glucose and insulin levels. Given the morbidity and mortality rate of metabolic diseases (Latin America counts for 26 million diabetic people and 10 million undiagnosed), the significance of this work lies in the conception of an automatic classifier for diagnosis support or preliminary screening in places with limited or non-existent health service delivery systems.


Similar content being viewed by others
Data Availability
Availability of data and material
The dataset used in this study is freely available at https://ieee-dataport.org/documents/fasting-and-postprandial-glucose-and-insulin-dataset
Code Availability
The code used in this study is freely available at https://codeocean.com/capsule/4180912/tree/v1
References
Alberti KG, Zimmet PZ. Definition, diagnosis and classification of diabetes mellitus and its complications. Part 1: diagnosis and classification of diabetes mellitus. Provisional report of a WHO consultation. Diabet Med. 1998;15(7):539-53.
Misra S, Hattersley AT. Monogenic causes of diabetes, chapter 18. Wiley Online Library; 2017. p. 241–261.
Marx J. Unraveling the causes of diabetes. Science. 2002;296(5568):686–9.
Rodríguez A, Delgado-Cohen H, Reviriego J, Serrano-Ríos M. Risk factors associated with metabolic syndrome in type 2 diabetes mellitus patients according to world health organization, third report national cholesterol education program, and international diabetes federation definitions. Diabetes, Metabolic Syndrome and Obesity: Targets and Therapy. 2011;4:1.
Willi C, Bodenmann P, Ghali WA, Faris PD, Cornuz J. Active smoking and the risk of type 2 diabetes: a systematic review and meta-analysis. Jama. 2007;298(22):2654-64.
Grootenhuis PA, Snoek FJ, Heine RJ, Bouter LM. Development of a type 2 diabetes symptom checklist: a measure of symptom severity. Diabet Med. 1994;11(3):253–61.
International Diabetes Federation. IDF diabetes atlas, 2017. Eighth edition.
Nieto-Martínez R, González-Rivas JP, Lima-Martínez M, Stepenka V, Rísquez A, Mechanick JI. Diabetes care in Venezuela. Ann Glob Health. 2015;81(6):776-91.
American Diabetes Association. 2. classification and diagnosis of diabetes: Standards of medical care in diabetes—2019. Diabetes Care, 42(Supplement 1):S13–S28, 2019.
Altuve M, Severeyn E. Joint analysis of fasting and postprandial plasma glucose and insulin concentrations in venezuelan women. Diabetes Metab Syndr Clin Res Rev. 2019;13(3):2242–8.
Melmed S, Polonsky KS, Larsen PR, Kronenberg HM. Williams Textbook of Endocrinology (Thirteenth Edition). Elsevier, 2015.
Burtis CA, Ashwood ER, Bruns DE. Tietz Textbook of Clinical Chemistry and Molecular Diagnostics (5th Edition). Saunders, 2011.
Karegowda AG, Manjunath AS, Jayaram MA. Application of genetic algorithm optimized neural network connection weights for medical diagnosis of pima Indians diabetes. International Journal on Soft Computing (IJSC). 2011;2(2):15-23.
Temurtas H, Yumusak N, Temurtas F. A comparative study on diabetes disease diagnosis using neural networks. Expert Systems with Applications. 2009;36(4):8610–5.
Soltani Z, Jafarian A. A new artificial neural networks approach for diagnosing diabetes disease type II. Int J Adv Comput Sci Appl. 2016;7(6):89–94.
Kannadasan K, Edla DR, Kuppili V. Type 2 diabetes data classification using stacked autoencoders in deep neural networks. Clinical Epidemiology and Global Health. 2019;7(4):530–535.
Hasan MK, Alam MA, Das D, Hossain E, Hasan M. Diabetes prediction using ensembling of different machine learning classifiers. IEEE Access. 2020;8:76516–76531.
Kaur H, Kumari V. Predictive modelling and analytics for diabetes using a machine learning approach. Applied Computing and Informatics, 2020.
Naz H, Ahuja S. Deep learning approach for diabetes prediction using PIMA Indian dataset. J Diabetes Metab Disord. 2020;19(1):391–403.
Esmaily H, Tayefi M, Doosti H, Ghayour-Mobarhan M, Nezami H, Amirabadizadeh A. A comparison between decision tree and random forest in determining the risk factors associated with type 2 diabetes. Journal of Research in Health Sciences. 2018;18(2):412.
Maniruzzaman M, Rahman MJ, Ahammed B, Abedin MM. Classification and prediction of diabetes disease using machine learning paradigm. Health Information Science and Systems. 2020;8(1):7.
Zou Q, Qu K, Luo Y, Yin D, Ju Y, Tang H. Predicting diabetes mellitus with machine learning techniques. Front Genet. 2018;9:515.
Sarwar A, Ali M, Manhas J, Sharma V. Diagnosis of diabetes type-II using hybrid machine learning based ensemble model. Int J Inf Technol. 2020;12(2):419–28.
Shuja M, Mittal S, Zaman M. Effective prediction of type II diabetes mellitus using data mining classifiers and smote. In Advances in Computing and Intelligent Systems. Springer, 2020. pp. 195–211.
Severeyn E, Wong S, Velásquez J, Perpiñán G, Herrera H, Altuve M, Díaz J. Diagnosis of type 2 diabetes and pre-diabetes using machine learning. In Latin American Conference on Biomedical Engineering. Springer, 2019. pp. 792–802.
Altuve M, Severeyn E. Cluster analysis based on fasting and postprandial plasma glucose and insulin concentrations. bioRxiv 2019. pp. 1–11.
Altuve M, Severeyn E. Fasting and postprandial glucose and insulin dataset, 2019.
Goodfellow I, Bengio Y, Courville A. Deep learning. MIT press, 2016.
Simon H. Neural networks and learning machines. Prentice Hall, 2009.
Rokach L, Maimon OZ. Data mining with decision trees: theory and applications. World Scientific, volume 69. 2008.
Liu DC, Nocedal J. On the limited memory BFGS method for large scale optimization. Math Program. 1989;45(1):503–528.
Kingman DP, Ba J. Adam: A method for stochastic optimization. In Proceedings of the 3rd International Conference on Learning Representations (ICLR), 2015.
Raileanu LA, Stoffel K. Theoretical comparison between the gini index and information gain criteria. Ann Math Artif Intell. 2004;41(1):77–93.
Van Asch V. Macro-and micro-averaged evaluation measures. Technical report, 2013.
Pedregosa F, Varoquaux G, Gramfort A, Michel V, Thirion B, Grisel O, Blondel M, Prettenhofer P, Weiss R, Dubourg V, et al. Scikit-learn: Machine learning in python. J Mach Learn Res. 2011;12:2825–30.
Petersen KF, Befroy D, Dufour S, Dziura J, Ariyan C, Rothman DL, DiPietro L, Cline GW, Shulman GI. Mitochondrial dysfunction in the elderly: possible role in insulin resistance. Science. 2003;300(5622):1140–1142.
Ling C, Groop L. Epigenetics: a molecular link between environmental factors and type 2 diabetes. Diabetes. 2009;58(12):2718–25.
Ching T, Himmelstein DS, Beaulieu-Jones BK, Kalinin AA, Do BT, Way GP, Ferrero E, Agapow PM, Zietz M, Hoffman MM, Xie W, Rosen GL, Lengerich BJ, Israeli J, Lanchantin J, Woloszynek S, Carpenter AE, Shrikumar A, Xu J, Cofer EM, Lavender CA, Turaga SC, Alexandari AM, Lu Z, Harris DJ, DeCaprio D, Qi Y, Kundaje A, Peng Y, Wiley LK, Segler MHS, Boca SM, Swamidass J, Huang A, Gitter A, Greene CS. Opportunities and obstacles for deep learning in biology and medicine. J R Soc Interface. 2018;15(141):20170387.
Shin HC, Roth HR, Gao M, Lu L, Xu Z, Nogues I, Yao J, Mollura D, Summers RM. Deep convolutional neural networks for computer-aided detection: Cnn architectures, dataset characteristics and transfer learning. IEEE Trans Med Imaging. 2016;35(5):1285–1298.
Beaulieu-Jones BK, Greene CS. Semi-supervised learning of the electronic health record for phenotype stratification. J Biomed Inform. 2016;64:168–78.
Himmelstein MS, Sanchez DT. Masculinity impediments: Internalized masculinity contributes to healthcare avoidance in men and women. J Health Psychol. 2016;21(7):1283–1292.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Conflicts of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Altuve, M., Alvarez, A.J. & Severeyn, E. Multiclass classification of metabolic conditions using fasting plasma levels of glucose and insulin. Health Technol. 11, 953–962 (2021). https://doi.org/10.1007/s12553-021-00550-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12553-021-00550-w