Abstract
Background
Technological advancements and ease of Internet access have increased the number of digital behavior change interventions (DBCIs). This systematic review and meta-analysis aimed to assess the effectiveness of DBCIs in reducing sedentary behavior (SB) and promoting physical activity (PA) in adults with diabetes.
Methods
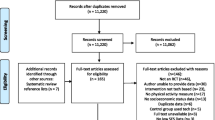
A comprehensive search of seven databases—PubMed, Embase, PsycINFO, Cochrane Library, CINAHL, Web of Science, and Sedentary Behavior Research Database—was performed. Two reviewers independently carried out the study selection, data extraction, risk of bias assessment, and quality of evidence evaluation. Meta-analyses were performed where feasible; otherwise, narrative summaries were performed.
Results
A total of 13 randomized controlled trials with 980 participants met the inclusion criteria. Overall, DBCIs could significantly increase steps and the number of breaks in sedentary time. The subgroup analyses exhibited significant effects in DBCIs with over 10 behavior change techniques (BCTs) in improving steps, the time spent in light physical activity (LPA), and moderate-to-vigorous physical activity (MVPA). The subgroup analyses showed a significant step increment in DBCIs of moderate and long durations, with over 4 BCT clusters, or in conjunction with a face-to-face component. The subgroup analyses also indicated significant effects in studies with ≥ 2 DBCI components in improving steps, the time spent in LPA and MVPA, and reducing sedentary time.
Conclusion
There is some evidence that DBCI may increase PA and reduce SB in adults with type 2 diabetes. However, more high-quality studies are required. Future studies are needed to examine the potential of DBCIs in adults with type 1 diabetes.



Similar content being viewed by others
Data Availability
All the data used in this study are available within the article.
References
Kanaley JA, Colberg SR, Corcoran MH, et al. Exercise/physical activity in individuals with type 2 diabetes: a consensus statement from the American College of Sports Medicine. Med Sci Sports Exerc. 2022;54(2):353–68.
Bull FC, Al-Ansari SS, Biddle S, et al. World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br J Sports Med. 2020;54(24):1451–62.
Colberg SR, Sigal RJ, Yardley JE, et al. Physical activity/exercise and diabetes: a position statement of the American Diabetes Association. Diabetes Care. 2016;39(11):2065–79.
Garcia JM, Cox D, Rice DJ. Association of physiological and psychological health outcomes with physical activity and sedentary behavior in adults with type 2 diabetes. BMJ Open Diabetes Res Care. 2017;5(1): e306.
Guo C, Zhou Q, Zhang D, et al. Association of total sedentary behaviour and television viewing with risk of overweight/obesity, type 2 diabetes and hypertension: a dose–response meta-analysis. Diabetes Obes Metab. 2020;22(1):79–90.
Fritschi C, Park H, Richardson A, et al. Association between daily time spent in sedentary behavior and duration of hyperglycemia in type 2 diabetes. Biol Res Nurs. 2016;18(2):160–6.
Rossen J, Von Rosen P, Johansson UB, et al. Associations of physical activity and sedentary behavior with cardiometabolic biomarkers in prediabetes and type 2 diabetes: a compositional data analysis. Phys Sportsmed. 2020;48(2):222–8.
Zhu X, Zhao L, Chen J, et al. The effect of physical activity on glycemic variability in patients with diabetes: a systematic review and meta-analysis of randomized controlled trials. Front Endocrinol (Lausanne). 2021;12: 767152.
Brugnara L, Murillo S, Novials A, et al. Low physical activity and its association with diabetes and other cardiovascular risk factors: a nationwide, population-based study. PLoS ONE. 2016;11(8): e160959.
Domínguez-Domínguez A, Martínez-Guardado I, Domínguez-Muñoz FJ, et al. Association between the level of physical activity and health-related quality of life in type 1 diabetes mellitus. A Preliminary Study J Clin Med. 2021;10(24):5829.
Ozaslan B, Patek SD, Breton MD. Impact of daily physical activity as measured by commonly available wearables on mealtime glucose control in type 1 diabetes. Diabetes Technol Ther. 2020;22(10):742–8.
Biswas A, Oh PI, Faulkner GE, et al. Sedentary time and its association with risk for disease incidence, mortality, and hospitalization in adults: a systematic review and meta-analysis. Ann Intern Med. 2015;162(2):123–32.
Thorsen IK, Kayser L, Teglgaard LH, et al. “I tried forcing myself to do it, but then it becomes a boring chore”: understanding (dis)engagement in physical activity among individuals with type 2 diabetes using a practice theory approach. Qual Health Res. 2022;32(3):520–30.
Balducci S, D’Errico V, Haxhi J, et al. Level and correlates of physical activity and sedentary behavior in patients with type 2 diabetes: a cross-sectional analysis of the Italian diabetes and exercise study_2. PLoS ONE. 2017;12(3): e173337.
Çelik Z, Törüner FB, Güçlü MB. Evaluation of quality of life and physical activity in patients with type 1 diabetes mellitus during the COVID-19 pandemic. Arch Endocrinol Metab. 2022;2359–3997000000531.
Riddell MC, Gallen IW, Smart CE, et al. Exercise management in type 1 diabetes: a consensus statement. Lancet Diabetes Endocrinol. 2017;5(5):377–90.
Centers for Disease Control and Prevention., CDC | National Diabetes Statistics Report. https://www.cdc.gov/diabetes/data/statistics/statistics-report.html. Accessed August 18, 2022.
Bohn B, Herbst A, Pfeifer M, et al. Impact of physical activity on glycemic control and prevalence of cardiovascular risk factors in adults with type 1 diabetes: a cross-sectional multicenter study of 18,028 patients. Diabetes Care. 2015;38(8):1536–43.
Balducci S, D’Errico V, Haxhi J, et al. Effect of a behavioral intervention strategy on sustained change in physical activity and sedentary behavior in patients with type 2 diabetes: the IDES_2 randomized clinical trial. JAMA. 2019;321(9):880–90.
Paing AC, Mcmillan KA, Kirk AF, et al. The associations of sedentary time and breaks in sedentary time with 24-hour glycaemic control in type 2 diabetes. Prev Med Rep. 2018;12:94–100.
Konerding U, Szel C. Promoting physical activity in persons with type 2 diabetes mellitus: a systematic review of systematic reviews. Patient Educ Couns. 2021;104(7):1600–7.
Korkiakangas EE, Alahuhta MA, Laitinen JH. Barriers to regular exercise among adults at high risk or diagnosed with type 2 diabetes: a systematic review. Health Promot Int. 2009;24(4):416–27.
Yardley L, Choudhury T, Patrick K, et al. Current issues and future directions for research into digital behavior change interventions. Am J Prev Med. 2016;51(5):814–5.
Rhee SY, Kim C, Shin DW, Steinhubl SR. Present and future of digital health in diabetes and metabolic disease. Diabetes Metab J. 2020;44(6):819–27.
Michie S, Richardson M, Johnston M, et al. The behavior change technique taxonomy (v1) of 93 hierarchically clustered techniques: building an international consensus for the reporting of behavior change interventions. Ann Behav Med. 2013;46(1):81–95.
Datz N, Kordonouri O, Danne T. Wenn Menschen mit Typ-1-Diabetes erwachsen werden When people with type 1 diabetes become adults - diabetes technology and transition - do we need new models? Dtsch Med Wochenschr. 2021;146(18):1200–5.
Keller R, Hartmann S, Teepe GW, et al. Digital behavior change interventions for the prevention and management of type 2 diabetes: systematic market analysis. J Med Internet Res. 2022;24(1): e33348.
Anthony CA, Femino JE, Miller AC, Polgreen LA, Rojas EO, Francis SL, Segre AM, Polgreen PM. Diabetic foot surveillance using mobile phones and automated software messaging, a randomized observational trial. Iowa Orthop J. 2020;40(1):35–42.
Fritschi C, Kim MJ, Srimoragot M, Jun J, Sanchez LE, Sharp LK. “Something tells me i can’t do that no more”: experiences with real-time glucose and activity monitoring among underserved Black women with type 2 diabetes. Sci Diabetes Self Manag Care. 2022;48(2):78–86.
Molavynejad S, Miladinia M, Jahangiri M. A randomized trial of comparing video telecare education vs. in-person education on dietary regimen compliance in patients with type 2 diabetes mellitus: a support for clinical telehealth providers. BMC Endocr Disord. 2022;22(1):116.
Stockwell S, Schofield P, Fisher A, et al. Digital behavior change interventions to promote physical activity and/or reduce sedentary behavior in older adults: a systematic review and meta-analysis. Exp Gerontol. 2019;120:68–87.
McLeroy KR, Bibeau D, Steckler A, Glanz K. An ecological perspective on health promotion programs. Health Educ Q. 1988;15(4):351–77.
Liebreich T, Plotnikoff RC, Courneya KS, et al. Diabetes NetPLAY: a physical activity website and linked email counselling randomized intervention for individuals with type 2 diabetes. Int J Behav Nutr Phys Act. 2009;6(1):18.
De Greef KP, Deforche BI, Ruige JB, et al. The effects of a pedometer-based behavioral modification program with telephone support on physical activity and sedentary behavior in type 2 diabetes patients. Patient Educ Couns. 2011;84(2):275–9.
Jennings CA, Vandelanotte C, Caperchione CM, et al. Effectiveness of a web-based physical activity intervention for adults with type 2 diabetes—a randomised controlled trial. Prev Med. 2014;60:33–40.
Agboola S, Jethwani K, Lopez L, et al. Text to move: a randomized controlled trial of a text-messaging program to improve physical activity behaviors in patients with type 2 diabetes mellitus. J Med Internet Res. 2016;18(11): e307.
Connelly J, Kirk A, Masthoff J, et al. A website to promote physical activity in people with type 2 diabetes living in remote or rural locations: feasibility pilot randomized controlled trial. JMIR Diabetes. 2017;2(2): e26.
Ramirez M, Wu S. Phone messaging to prompt physical activity and social support among low-income latino patients with type 2 diabetes: a randomized pilot study. JMIR diabetes. 2017;2(1): e8.
Akinci B, Yeldan I, Satman I, et al. The effects of Internet-based exercise compared with supervised group exercise in people with type 2 diabetes: a randomized controlled study. Clin Rehabil. 2018;32(6):799–810.
Arovah NI, Kushartanti BMW, Washington TL, et al. Walking with diabetes (WW-DIAB) programme a walking programme for Indonesian type 2 diabetes mellitus patients: a pilot randomised controlled trial. SAGE Open Med. 2018;6:1936895009.
Kooiman TJM, de Groot M, Hoogenberg K, et al. Self-tracking of physical activity in people with type 2 diabetes. Comput Inform Nurs. 2018;36(7):340–9.
Höchsmann C, Müller O, Ambühl M, et al. Novel smartphone game improves physical activity behavior in type 2 diabetes. Am J Prev Med. 2019;57(1):41–50.
Poppe L, De Bourdeaudhuij I, Verloigne M, et al. Efficacy of a self-regulation–based electronic and mobile health intervention targeting an active lifestyle in adults having type 2 diabetes and in adults aged 50 years or older: two randomized controlled trials. J Med Internet Res. 2019;21(8): e13363.
Bailey DP, Mugridge LH, Dong F, et al. Randomised Controlled feasibility study of the MyHealthAvatar-Diabetes smartphone app for reducing prolonged sitting time in type 2 diabetes mellitus. Int J Environ Res Pub Health. 2020;17(12):4414.
Pelletier C, Gagnon M, Alméras N, et al. Using an activity tracker to increase motivation for physical activity in patients with type 2 diabetes in primary care: a randomized pilot trial. mHealth. 2021;7:59.
Sriram RD, Reddy SSK. Artificial intelligence and digital tools: future of diabetes care. Clin Geriatr Med. 2020;36(3):513–25.
Moher DLAT. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Annals Intern Med. 2009;4(151):264–9.
Aromataris E, Riitano D. Constructing a search strategy and searching for evidence. A guide to the literature search for a systematic review. Am J Nurs. 2014;114(5):49–56.
Tremblay MS, Aubert S, Barnes JD, et al. Sedentary Behavior Research Network (SBRN) - terminology consensus project process and outcome. Int J Behav Nutr Phys Act. 2017;14(1):75.
Caspersen CJ, Powell KE, Christenson GM. Physical activity, exercise, and physical fitness: definitions and distinctions for health-related research. Pub Health Rep. 1985;100(2):126–31.
Hoffmann TC, Glasziou PP, Boutron I, et al. Better reporting of interventions: template for intervention description and replication (TIDieR) checklist and guide. BMJ. 2014;348: g1687.
Higgins Jph T J C J. Cochrane handbook for systematic reviews of interventions version 6.0 (updated July 2019)[EB/OL]. www.training.cochrane.org/handbook.
Guyatt GH, Oxman AD, Vist GE, et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ. 2008;336(7650):924–6.
Sterne JA, Sutton AJ, Ioannidis JP, et al. Recommendations for examining and interpreting funnel plot asymmetry in meta-analyses of randomised controlled trials. BMJ. 2011;343: d4002.
Roberts AL, Fisher A, Smith L, et al. Digital health behaviour change interventions targeting physical activity and diet in cancer survivors: a systematic review and meta-analysis. J Cancer Surviv. 2017;11(6):704–19.
Martín-Martín J, Roldán-Jiménez C, De-Torres I, et al. Behavior change techniques and the effects associated with digital behavior change interventions in sedentary behavior in the clinical population: a systematic review. Front Digit Health. 2021;3: 620383.
El-Gayar O, Ofori M, Nawar N. On the efficacy of behavior change techniques in mHealth for self-management of diabetes: a meta-analysis. J Biomed Inform. 2021;119: 103839.
McEwan D, Beauchamp MR, Kouvousis C, et al. Examining the active ingredients of physical activity interventions underpinned by theory versus no stated theory: a meta-analysis. Health Psychol Rev. 2019;13(1):1–17.
Martin A, Fitzsimons C, Jepson R, et al. Interventions with potential to reduce sedentary time in adults: systematic review and meta-analysis. Br J Sports Med. 2015;49(16):1056–63.
Prince SA, Saunders TJ, Gresty K, et al. A comparison of the effectiveness of physical activity and sedentary behaviour interventions in reducing sedentary time in adults: a systematic review and meta-analysis of controlled trials. Obes Rev. 2014;15(11):905–19.
Chastin S, Gardiner PA, Harvey JA, et al. Interventions for reducing sedentary behaviour in community-dwelling older adults. Cochrane Database Syst Rev. 2021;6(6):D12784.
Gomersall S, Maher C, English C, et al. Time regained: when people stop a physical activity program, how does their time use change? A randomised controlled trial. PLoS ONE. 2015;10(5): e126665.
Melanson EL. The effect of exercise on non-exercise physical activity and sedentary behavior in adults. Obes Rev. 2017;18(Suppl 1):40–9.
Copeland JL, Ashe MC, Biddle SJ, et al. Sedentary time in older adults: a critical review of measurement, associations with health, and interventions. Br J Sports Med. 2017;51(21):1539.
Ferguson T, Olds T, Curtis R, et al. Effectiveness of wearable activity trackers to increase physical activity and improve health: a systematic review of systematic reviews and meta-analyses. Lancet Digit Health. 2022;4(8):e615–26.
Michie S, Johnston M, Francis JJ, et al. From theory to intervention: mapping theoretically derived behavioural determinants to behaviour change techniques. John Wiley & Sons Ltd. 2008;4:660–80.
Springer MV, Sales AE, Islam N, et al. A step toward understanding the mechanism of action of audit and feedback: a qualitative study of implementation strategies. Implement Sci. 2021;16(1):35.
Ostman C, Jewiss D, King N, Smart NA. Clinical outcomes to exercise training in type 1 diabetes: a systematic review and meta-analysis. Diabetes Res Clin Pract. 2018;139:380–91.
Frier BM. Hypoglycaemia in diabetes mellitus: epidemiology and clinical implications. Nat Rev Endocrinol. 2014;10(12):711–22.
Seok H, Huh JH, Kim HM, et al. 1,5-anhydroglucitol as a useful marker for assessing short-term glycemic excursions in type 1 diabetes. Diabetes Metab J. 2015;39(2):164–70.
Funding
This study was funded by Beijing University of Traditional Chinese Medicine 2022 University-Industry Collaborative Education Program of the Ministry of Education (No. BUCM-2022-JWC-CXY-15).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical Approval
This study was approved by the Ethics Committee of Beijing University of Chinese Medicine (2022BZYLL0505).
Consent to Participate
Not applicable.
Welfare of Animals
Not applicable.
Competing Interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zhang, X., Qiao, X., Peng, K. et al. Digital Behavior Change Interventions to Reduce Sedentary Behavior and Promote Physical Activity in Adults with Diabetes: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Int.J. Behav. Med. (2023). https://doi.org/10.1007/s12529-023-10188-9
Accepted:
Published:
DOI: https://doi.org/10.1007/s12529-023-10188-9