Abstract
Background
Little is known about the association between marital status and long-term outcomes of patients hospitalized with heart failure (HF). We aimed to examine the association between marital status and early as well as long-term outcomes of patients hospitalized with HF.
Method
We analyzed data of 4089 patients hospitalized with HF and were enrolled in the multicenter national survey in Israel between March and April 2003 and were followed until December 2014. Patients were classified into married (N = 2462, 60%) and unmarried (N = 1627, 40%).
Results
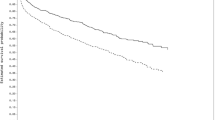
Married patients were more likely to be males, younger, and more likely to have past myocardial infarction and previous revascularization. Also, they tended to have higher rates of diabetes mellitus (DM) and dyslipidemia, as well as smokers. Survival analysis showed that unmarried patients had higher mortality rates at 1 and 10 years (33% vs. 25%, at 1 year, 89% vs. 80% at 10 years, all p < 0.001). Consistently, multivariable analysis showed that unmarried patients had independently 44% and 35% higher risk of mortality at 1- and 10-year follow-up respectively (1-year HR = 1.44; 95%CI 1.14–1.81; p = 0.002, 10-year HR = 1.35; 95%CI 1.19–1.53; p ≤ 0.001). Other consistent predictors of mortality at both 1- and 10-year follow-up include age, renal failure, and advanced HF.
Conclusions
Being unmarried is independently associated with worse short- and long-term outcomes, particularly among women. Thus, attempts to intensify secondary preventive measures should focus mainly on unmarried patients and mainly women.



Similar content being viewed by others
References
Komanduri S, Jadhao Y, Guduru SS, et al. Prevalence and risk factors of heart failure in the USA: NHANES 2013–2014 epidemiological follow-up study. J Community Hosp Intern Med Perspect. 2017;7:15–20.
Shah KS, Xu H, Matsouaka RA, et al. Heart failure with preserved, borderline, and reduced ejection fraction: 5-year outcomes. J Am Coll Cardiol. 2017;70:2476–86.
Virani SS, Alonso A, Benjamin EJ, et al. Heart Disease and Stroke Statistics-2020 update: a report From the American Heart Association. Circulation. 2020;141:e139–596.
Mozaffarian D, Benjamin EJ, Go AS, et al. Heart disease and stroke statistics–2015 update: a report from the American Heart Association. Circulation. 2015;131:e29-322.
McMurray JJ, Packer M, Desai AS, et al. Angiotensin-neprilysin inhibition versus enalapril in heart failure. N Engl J Med. 2014;371:993–1004.
Taylor CJ, Ordonez-Mena JM, Roalfe AK, et al. Trends in survival after a diagnosis of heart failure in the United Kingdom 2000–2017: population based cohort study. BMJ. 2019;364: l223.
Metra M, Teerlink JR. Heart failure. Lancet. 2017;390:1981–95.
Gustafsson F, Rogers JG. Left ventricular assist device therapy in advanced heart failure: patient selection and outcomes. Eur J Heart Fail. 2017;19:595–602.
Braunwald E. Heart failure. JACC. Heart Fail. 2013;1:1–20.
Maggioni AP, Dahlstrom U, Filippatos G, et al. EURObservational Research Programme: regional differences and 1-year follow-up results of the Heart Failure Pilot Survey (ESC-HF Pilot). Eur J Heart Fail. 2013;15:808–17.
Dhindsa DS, Khambhati J, Schultz WM, et al. Marital status and outcomes in patients with cardiovascular disease. Trends Cardiovasc Med. 2020;30:215–20.
Schultz WM, Hayek SS, Samman Tahhan A et al. Marital status and outcomes in patients with cardiovascular disease. J Am Heart Assoc 2017;6.
Wong CW, Kwok CS, Narain A, et al. Marital status and risk of cardiovascular diseases: a systematic review and meta-analysis. Heart. 2018;104:1937–48.
Marcus G, Litovchik I, Pereg D, et al. Impact of marital status on the outcome of acute coronary syndrome: results from the Acute Coronary Syndrome Israeli Survey. J Am Heart Assoc. 2019;8: e011664.
Hayes RM, Carter PR, Gollop ND, et al. The impact of marital status on mortality and length of stay in patients admitted with acute coronary syndrome. Int J Cardiol. 2016;212:142–4.
Luttik ML, Jaarsma T, Veeger N, van Veldhuisen DJ. Marital status, quality of life, and clinical outcome in patients with heart failure. Heart Lung. 2006;35:3–8.
Rohrbaugh MJ, Shoham V, Coyne JC. Effect of marital quality on eight-year survival of patients with heart failure. Am J Cardiol. 2006;98:1069–72.
Chung ML, Lennie TA, Riegel B, et al. Marital status as an independent predictor of event-free survival of patients with heart failure. Am J Crit Care. 2009;18:562–70.
Wu JR, Lennie TA, Chung ML, et al. Medication adherence mediates the relationship between marital status and cardiac event-free survival in patients with heart failure. Heart Lung. 2012;41:107–14.
Matsushita M, Shirakabe A, Hata N, et al. Social determinants are crucial factors in the long-term prognosis of severely decompensated acute heart failure in patients over 75 years of age. J Cardiol. 2018;72:140–8.
Hunt SA, College A, of C, American Heart Association Task Force on Practice G. ACC, AHA,. guideline update for the diagnosis and management of chronic heart failure in the adult: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Update the 2001 Guidelines for the Evaluation and Management of Heart Failure). J Am Coll Cardiol. 2005;2005(46):e1-82.
Garty M, Shotan A, Gottlieb S, et al. The management, early and one year outcome in hospitalized patients with heart failure: a national Heart Failure Survey in Israel–HFSIS 2003. Isr Med Assoc J. 2007;9:227–33.
Barsheshet A, Shotan A, Cohen E, et al. Predictors of long-term (4-year) mortality in elderly and young patients with acute heart failure. Eur J Heart Fail. 2010;12:833–40.
Younis A, Mulla W, Goldkorn R, et al. Differences in mortality of new-onset (de-novo) acute heart failure versus acute decompensated chronic heart failure. Am J Cardiol. 2019;124:554–9.
Mulla W, Goldenberg I, Klempfner R et al. Sex differences in clinical characteristics and 1- and 10-year mortality among patients hospitalized with acute heart failure. Am J Med Sci 2020.
Mulla W, Klempfner R, Natanzon S et al. Female gender is associated with a worse prognosis amongst patients hospitalised for de-novo acute heart failure. Int J Clin Pract 2020: e13902.
Rich MW, Gray DB, Beckham V, et al. Effect of a multidisciplinary intervention on medication compliance in elderly patients with congestive heart failure. Am J Med. 1996;101:270–6.
DiMatteo MR. Social support and patient adherence to medical treatment: a meta-analysis. Health Psychol. 2004;23:207–18.
Molloy GJ, Hamer M, Randall G, Chida Y. Marital status and cardiac rehabilitation attendance: a meta-analysis. Eur J Cardiovasc Prev Rehabil. 2008;15:557–61.
Kulkarni SP, Alexander KP, Lytle B, et al. Long-term adherence with cardiovascular drug regimens. Am Heart J. 2006;151:185–91.
Shen BJ, Xu Y, Eisenberg S. Psychosocial and physiological predictors of mortality in patients of heart failure: independent effects of marital status and C-reactive protein. Int J Behav Med. 2017;24:83–91.
Burnett H, Earley A, Voors AA et al. Thirty years of evidence on the efficacy of drug treatments for chronic heart failure with reduced ejection fraction: a network meta-analysis. Circ Heart Fail 2017;10.
Ergatoudes C, Schaufelberger M, Andersson B et al. Non-cardiac comorbidities and mortality in patients with heart failure with reduced vs. preserved ejection fraction: a study using the Swedish Heart Failure Registry. Clin Res Cardiol 2019;108:1025–33.
Kewcharoen J, Thangjui S, Kanitsoraphan C, et al. The effects of marital status on outcome of heart failure population: a systematic review and meta-analysis. Acta Cardiol. 2021;76:11–9.
Lu MLR, Davila CD, Shah M, et al. Marital status and living condition as predictors of mortality and readmissions among African Americans with heart failure. Int J Cardiol. 2016;222:313–8.
Matthews KA, Gump BB. Chronic work stress and marital dissolution increase risk of posttrial mortality in men from the Multiple Risk Factor Intervention Trial. Arch Intern Med. 2002;162:309–15.
Orth-Gomer K, Wamala SP, Horsten M, et al. Marital stress worsens prognosis in women with coronary heart disease: The Stockholm Female Coronary Risk Study. JAMA. 2000;284:3008–14.
Beam CR, Dinescu D, Emery R, Turkheimer E. A twin study on perceived stress, depressive symptoms, and marriage. J Health Soc Behav. 2017;58:37–53.
Freudenberger R, Cahn SC, Skotzko C. Influence of age, gender, and race on depression in heart failure patients. J Am Coll Cardiol 2004;44: 2254–5; author reply 5–6.
Gottlieb SS, Khatta M, Friedmann E, et al. The influence of age, gender, and race on the prevalence of depression in heart failure patients. J Am Coll Cardiol. 2004;43:1542–9.
Kristofferzon ML, Lofmark R, Carlsson M. Myocardial infarction: gender differences in coping and social support. J Adv Nurs. 2003;44:360–74.
Al-Khatib SM, Hellkamp AS, Hernandez AF, et al. Trends in use of implantable cardioverter-defibrillator therapy among patients hospitalized for heart failure: have the previously observed sex and racial disparities changed over time? Circulation. 2012;125:1094–101.
Pavlovic A, Polovina M, Ristic A, et al. Long-term mortality is increased in patients with undetected prediabetes and type-2 diabetes hospitalized for worsening heart failure and reduced ejection fraction. Eur J Prev Cardiol. 2019;26:72–82.
Damman K, Valente MA, Voors AA, et al. Renal impairment, worsening renal function, and outcome in patients with heart failure: an updated meta-analysis. Eur Heart J. 2014;35:455–69.
Murberg TA, Bru E, Aarsland T, Svebak S. Social support, social disability and their role as predictors of depression among patients with congestive heart failure. Scand J Soc Med. 1998;26:87–95.
Coyne JC, Rohrbaugh MJ, Shoham V, et al. Prognostic importance of marital quality for survival of congestive heart failure. Am J Cardiol. 2001;88:526–9.
Acknowledgements
The study was possible by the combined efforts of the HFSIS Study Group and the Israeli Association for Cardiovascular Trials.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/ or national research committee and with 1964 Helsinki declaration and its later amendments or comparable ethical standards. For this type of study formal consent is not required.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Research Involving Human and Animal Participants
This article does not contain any studies with animals performed by any of the authors.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Maizels, L., Mulla, W., Grupper, A. et al. The Association between Marital Status and Outcomes of Patients Hospitalized with Heart Failure. Int.J. Behav. Med. 30, 532–542 (2023). https://doi.org/10.1007/s12529-022-10117-2
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12529-022-10117-2