Abstract
Background
Psychological disorders can substantially worsen physical symptoms associated with breast cancer diagnosis and treatment, reducing survivors’ quality of life and increasing recurrence risk. Distress disorders may be particularly detrimental given their physical correlates. Across two studies, we examined the relationship between a distress disorder history and physical symptoms pre- and post-adjuvant treatment — two important periods of the cancer trajectory.
Methods
Breast cancer patients awaiting adjuvant treatment (n = 147; mean age = 52.54) in study 1 and survivors 1–10 years post-treatment (n = 183; mean age = 56.11) in study 2 completed a diagnostic interview assessing lifetime presence of psychological disorders. They also rated their pain, fatigue, physical functioning, and self-rated health. Covariates included body mass index, age, cancer stage, menopause status, and physical comorbidities.
Results
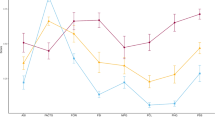
Results from both studies indicated that a distress disorder history was associated with higher pain, fatigue, and sleep difficulties as well as lower self-rated health compared to those without such a history.
Conclusions
These findings suggest that breast cancer survivors with a distress disorder may be particularly at risk for more physical symptoms, poorer sleep, and worse self-rated health both prior to and following adjuvant treatment.
Similar content being viewed by others
References
Watson D. Rethinking the mood and anxiety disorders: a quantitative hierarchical model for DSM-V. J Abnorm Psychol. 2005;114(4):522–36.
Tyrer P, Baldwin D. Generalised anxiety disorder. The Lancet. 2006;368(9553):2156–66.
Hare DL, et al. Depression and cardiovascular disease: a clinical review. Eur Heart J. 2014;35(21):1365–72.
Cohen BE, Edmondson D, Kronish IM. State of the art review: depression, stress, anxiety, and cardiovascular disease. Am J Hypertens. 2015;28(11):1295–302.
Niedzwiedz CL, et al. Depression and anxiety among people living with and beyond cancer: a growing clinical and research priority. BMC Cancer. 2019;19(1):1–8.
Mehnert A, et al. One in two cancer patients is significantly distressed: prevalence and indicators of distress. Psychooncology. 2018;27(1):75–82.
Syrowatka A, et al. Predictors of distress in female breast cancer survivors: a systematic review. Breast Cancer Res Treat. 2017;165(2):229–45.
Carreira H, et al. Associations between breast cancer survivorship and adverse mental health outcomes: a systematic review. JNCI: J Nat Cancer Ins. 2018;110(12):1311–1327.
Pilevarzadeh M, et al. Global prevalence of depression among breast cancer patients: a systematic review and meta-analysis. Breast Cancer Res Treat. 2019;176(3):519–33.
Fatiregun OA, et al. Anxiety disorders in breast cancer: prevalence, types, and determinants. 2016;34(5):32–447.
Administration S.A.a.M.H.S. Key substance use and mental health indicators in the United States: results from the 2019 National Survey on Drug Use and Health. 2020.
O’Connor M, et al. How traumatic is breast cancer? Post-traumatic stress symptoms (PTSS) and risk factors for severe PTSS at 3 and 15 months after surgery in a nationwide cohort of Danish women treated for primary breast cancer. Br J Cancer. 2011;104(3):419.
Bleiker EM, et al. Psychological distress two years after diagnosis of breast cancer: frequency and prediction. Patient Educ Couns. 2000;40(3):209–17.
Hewitt M, Rowland JH, Yancik R. Cancer survivors in the United States: age, health, and disability. Journal of Gerontology: Medical Sciences. 2003;58:82–91.
Sheridan D, et al. Long-term follow-up of pain and emotional characteristics of women after surgery for breast cancer. J Pain Symptom Manage. 2012;44(4):608–14.
Laird BJ, et al. Pain, depression, and fatigue as a symptom cluster in advanced cancer. J Pain Symptom Manage. 2011;42(1):1–11.
Savard J, et al. Prevalence, clinical characteristics, and risk factors for insomnia in the context of breast cancer. Sleep. 2001;24(5):583–90.
Bower JE, et al. Fatigue in long-term breast carcinoma survivors: a longitudinal investigation. Cancer. 2006;106(4):751–8.
Hagen KB, et al. Fatigue, anxiety and depression overrule the role of oncological treatment in predicting self-reported health complaints in women with breast cancer compared to healthy controls. The Breast. 2016;28:100–6.
Bower JE, et al. Fatigue in breast cancer survivors: occurrence, correlates, and impact on quality of life. J Clin Oncol. 2000;18(4):743–743.
Vahdaninia M, Omidvari S, Montazeri A. What do predict anxiety and depression in breast cancer patients? A follow-up study. Soc Psychiatry Psychiatr Epidemiol. 2010;45(3):355–61.
Curt GA, et al. Impact of cancer-related fatigue on the lives of patients: new findings from the Fatigue Coalition. Oncologist. 2000;5(5):353–60.
Burcusa SL, Iacono WG. Risk for recurrence in depression. Clin Psychol Rev. 2007;27(8):959–85.
Wichers M, et al. Scars in depression: is a conceptual shift necessary to solve the puzzle? Psychol Med. 2010;40(3):359–65.
Gunthert KC, et al. Depression and next-day spillover of negative mood and depressive cognitions following interpersonal stress. Cogn Ther Res. 2007;31(4):521–32.
Husky MM, et al. Past depression and gender interact to influence emotional reactivity to daily life stress. Cogn Ther Res. 2009;33(3):264–71.
Jim HS, et al. History of major depressive disorder prospectively predicts worse quality of life in women with breast cancer. Ann Behav Med. 2012;43(3):402–8.
Jensen LS, et al. The impact of prior psychiatric medical treatment on return to work after a diagnosis of breast cancer: a registry based study. Scandinavian journal of public health. 2019;47(5):519–27.
First MB, et al. Structured clinical interview for DSM-V axis I disorders, research version, patient edition. 2015: Arlington, VA.
Hays RD, Morales LS. The RAND-36 measure of health-related quality of life. Ann Med. 2001;33(5):350–7.
Stanton AL, Bernaards CA, Ganz PA. The BCPT symptom scales: a measure of physical symptoms for women diagnosed with or at risk for breast cancer. J Natl Cancer Inst. 2005;97(6):448–56.
Fu MR, et al. Comorbidities and quality of life among breast cancer survivors: a prospective study. Journal of personalized medicine. 2015;5(3):229–42.
Partridge AH, Burstein HJ, Winer EP. Side effects of chemotherapy and combined chemohormonal therapy in women with early-stage breast cancer. JNCI Monographs. 2001;2001(30):135–42.
Charlson ME, et al. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–83.
McFarland DC, et al. Physical symptom burden and its association with distress, anxiety, and depression in breast cancer. Psychosomatics. 2018;59(5):464–71.
Kurtz ME, et al. Physical functioning and depression among older persons with cancer. Cancer Pract. 2001;9(1):11–8.
Faller H, et al. Symptoms of depression and anxiety as predictors of physical functioning in breast cancer patients. A prospective study using path analysis. Acta Oncologica, 2017;56(12):1677–1681.
Renna ME, et al. Worry and rumination in breast cancer patients: perseveration worsens self-rated health. J Behav Med. 2021;44(2):253–9.
Renna ME, et al. Within-person changes in cancer-related distress predict breast cancer survivors’ inflammation across treatment. Psychoneuroendocrinology. 2020;121: 104866.
Clancy F, et al. Perseverative cognition and health behaviors: a systematic review and meta-analysis. Front Hum Neurosci. 2016;10:534.
Strine TW, et al. The association of depression and anxiety with obesity and unhealthy behaviors among community-dwelling US adults. Gen Hosp Psychiatry. 2008;30(2):127–37.
Doyle C, et al. Nutrition and physical activity during and after cancer treatment: an American Cancer Society guide for informed choices. CA: A Cancer Journal for Clinicians. 2006;56(6):323–353.
Tatrow K, Montgomery GH. Cognitive behavioral therapy techniques for distress and pain in breast cancer patients: a meta-analysis. J Behav Med. 2006;29(1):17–27.
Cramer H, et al. Mindfulness-based stress reduction for breast cancer—a systematic review and meta-analysis. Curr Oncol. 2012;19(5): e343.
Kiecolt-Glaser JK, et al. Yoga’s impact on inflammation, mood, and fatigue in breast cancer survivors: a randomized controlled trial. J Clin Oncol. 2014;32(10):1040.
Rankin NM, et al. Everybody wants it done but nobody wants to do it: an exploration of the barrier and enablers of critical components towards creating a clinical pathway for anxiety and depression in cancer. BMC Health Serv Res. 2015;15(1):1–8.
CoC. Optimal Resources for Cancer Care (2020 Standards). 2019 [cited 2020 04/24/2020]; Available from: https://www.facs.org/-/media/files/quality-programs/cancer/coc/optimal_resources_for_cancer_care_2020_standards.ashx.
Andersen BL, et al. Screening, assessment, and care of anxiety and depressive symptoms in adults with cancer: an American Society of Clinical Oncology guideline adaptation. J Clin Oncol. 2014;32(15):1605–19.
Funding
Work on this project was supported by NIH grants R01CA186720, R01CA186251, T32 CA229114, and TL1TR002735.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics Approval
All procedures performed in these studies were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments.
Consent to Participate
Informed consent was obtained from all individual participants included in the study.
Competing Interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Renna, M.E., Shrout, M.R., Madison, A.A. et al. Distress Disorder Histories Relate to Greater Physical Symptoms Among Breast Cancer Patients and Survivors: Findings Across the Cancer Trajectory. Int.J. Behav. Med. 30, 463–472 (2023). https://doi.org/10.1007/s12529-022-10115-4
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12529-022-10115-4