Abstract
Background
Many women internalize negative attitudes regarding body shape and size because of the societal standards for women’s ideal body shapes and sizes. Internalized weight stigma is related to poorer physical and psychological health. A growing body of research has documented the links between other forms of internalized stigma (e.g., HIV-stigma) and poor sleep quality; however, little research examines the links between internalized weight stigma and sleep or the mechanisms that explain this relationship. Internalized weight stigma may be associated with poor sleep through increases in psychological distress. This study hypothesized that the links between internalized weight stigma and sleep would be mediated by higher levels of depression and anxiety.
Methods
About 257 women were recruited via social media, word of mouth, and an undergraduate participant pool. Participants completed an online survey assessing various aspects of weight stigma and health through self-report questionnaires. Most women were non-Hispanic White (86.8%) and had a mean age of 31.40.
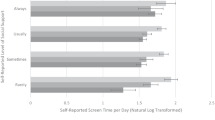
Results
The indirect effects of internalized weight stigma on poorer global sleep quality and daily disturbances through depression and anxiety were significant. In contrast, depressive symptoms but not anxiety explained the links between internalized weight stigma and perceived sleep quality and neither depressive symptoms nor anxiety explained the link between internalized weight stigma and sleep efficiency.
Conclusions
Internalized weight stigma is linked to poorer sleep quality, and these links may be explained by psychological well-being. Understanding the mechanisms by which internalized weight stigma is associated with sleep quality can inform the psychological interventions employed.

Similar content being viewed by others
Notes
This model with global sleep quality was also tested without covariates and results were consistent with the model tested with covariates.
References
Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011–2012. Jama. 2014;311(8):806–14. https://doi.org/10.1001/jama.2014.732.
Bozsik F, Whisenhunt BL, Hudson DL, Bennett B, Lundgren JD. Thin is in? Think again: the rising importance of muscularity in the thin ideal female body. Sex Roles. 2018;79:609–15. https://doi.org/10.1007/s11199-017-0886-0.
Pearl RL, Puhl RM. Measuring internalized weight attitudes across body weight categories: validation of the modified weight bias internalization scale. Body Image. 2014;11(1):89–92. https://doi.org/10.1016/j.bodyim.2013.09.005.
Nutt D, Wilson S, Paterson L. Sleep disorders as core symptoms of depression. Dialogues Clin Neurosci. 2008;10(3):329.
Spira AP, Stone K, Beaudreau SA, Ancoli-Israel S, Yaffe K. Anxiety symptoms and objectively measured sleep quality in older women. Am J Geriatr Psychiatry. 2009;17(2):136–43. https://doi.org/10.1097/JGP.0b013e3181871345.
Knutson KL, Spiegel K, Penev P, Van Cauter E. The metabolic consequences of sleep deprivation. Sleep Med Rev. 2007;11(3):163–78. https://doi.org/10.1016/j.smrv.2007.01.002.
Cappuccio FP, Taggart FM, Kandala NB, Currie A, Peile E, Stranges S, Miller MA. Meta-analysis of short sleep duration and obesity in children and adults. Sleep. 2008;31(5):619–26. https://doi.org/10.1093/sleep/31.5.619.
Madrid-Valero JJ, Martínez-Selva JM, Couto BRD, Sánchez-Romera JF, Ordoñana JR. Age and gender effects on the prevalence of poor sleep quality in the adult population. Gac Sanit. 2017;31:18–22. https://doi.org/10.1016/j.gaceta.2016.05.013.
Luyster FS, Strollo PJ, Zee PC, Walsh JK. Sleep: a health imperative. Sleep. 2012;35(6):727–34. https://doi.org/10.5665/sleep.1846.
Spiegel K, Tasali E, Penev P, Van Cauter E. Brief communication: sleep curtailment in healthy young men is associated with decreased leptin levels, elevated ghrelin levels, and increased hunger and appetite. Ann Intern Med. 2004;141(11):846–50. https://doi.org/10.7326/0003-4819-141-11-200412070-00008.
Chennaoui M, Arnal PJ, Sauvet F, Léger D. Sleep and exercise: a reciprocal issue? Sleep Med Rev. 2015;20:59–72. https://doi.org/10.1016/j.smrv.2014.06.008.
Chrousos G, Vgontzas AN, Kritikou I. HPA axis and sleep. In Endotext[Internet]. MDText. com, Inc. 2016.
Hall MH, Casement MD, Troxel WM, Matthews KA, Bromberger JT, Kravitz HM, Krafty RT, Buysse DJ. Chronic stress is prospectively associated with sleep in midlife women: the SWAN sleep study. Sleep. 2015;38(10):1645–54. https://doi.org/10.5665/sleep.5066.
Hilbert A, Braehler E, Haeuser W, Zenger M. Weight bias internalization, core self-evaluation, and health in overweight and obese persons. Obesity. 2014;22(1):79–88. https://doi.org/10.1002/oby.20561.
Pearl RL, Puhl RM. Weight bias internalization and health: a systematic review. Obes Rev. 2018;19(8):1141–63. https://doi.org/10.1111/obr.12701.
Ratcliffe D, Ellison N. Obesity and internalized weight stigma: a formulation model for an emerging psychological problem. Behav Cogn Psychother. 2015;43(2):239. https://doi.org/10.1017/S1352465813000763.
Kim S, Thibodeau R, Jorgensen RS. Shame, guilt, and depressive symptoms: a meta-analytic review. Psychol Bull. 2011;137(1):68. https://doi.org/10.1037/a0021466.
Sowislo JF, Orth U. Does low self-esteem predict depression and anxiety? A meta-analysis of longitudinal studies. Psychol Bull. 2013;139(1):213. https://doi.org/10.1037/a0028931.
Boswell RG, White MA. Gender differences in weight bias internalization and eating pathology in overweight individuals. Advances in Eating Disorders. 2015;3(3):259–68. https://doi.org/10.1080/21662630.2015.1047881.
Douglas V, Varnado-Sullivan P. Weight stigmatization, internalization, and eating disorder symptoms: the role of emotion dysregulation. Stigma and Health. 2016;1(3):166. https://doi.org/10.1037/sah0000029.
Durso LE, Latner JD. Understanding self-directed stigma: development of the weight bias internalization scale. Obesity. 2008;16(S2):S80–6. https://doi.org/10.1038/oby.2008.448.
Durso LE, Latner JD, Hayashi K. Perceived discrimination is associated with binge eating in a community sample of non-overweight, overweight, and obese adults. Obes Facts. 2012;5(6):869–80. https://doi.org/10.1159/000345931.
Himmelstein MS, Puhl RM, Quinn DM. Intersectionality: an understudied framework for addressing weight stigma. Am J Prev Med. 2017;53(4):421–31. https://doi.org/10.1016/j.amepre.2017.04.003.
Puhl RM, Quinn DM, Weisz BM, Suh YJ. The role of stigma in weight loss maintenance among US adults. Ann Behav Med. 2017;51(5):754–63. https://doi.org/10.1007/s12160-017-9898-9.
O’Brien KS, Latner JD, Puhl RM, Vartanian LR, Giles C, Griva K, Carter A. The relationship between weight stigma and eating behavior is explained by weight bias internalization and psychological distress. Appetite. 2016;102:70–6. https://doi.org/10.1016/j.appet.2016.02.032.
Sevinçer GM, Konuk N, İpekçioğlu D, Crosby RD, Cao L, Coskun H, Mitchell JE. Association between depression and eating behaviors among bariatric surgery candidates in a Turkish sample. Eating and Weight Disorders-Studies on Anorexia Bulimia and Obesity. 2017;22(1):117–23. https://doi.org/10.1007/s40519-016-0296-2.
Pearl RL, Puhl RM, Dovidio JF. Differential effects of weight bias experiences and internalization on exercise among women with overweight and obesity. J Health Psychol. 2015;20(12):1626–32. https://doi.org/10.1177/1359105313520338.
Vartanian LR, Pinkus RT, Smyth JM. Experiences of weight stigma in everyday life: implications for health motivation. Stigma and Health. 2018;3(2):85. https://doi.org/10.1037/sah0000077.
Fekete EM, Williams SL, Skinta MD. Internalised HIV-stigma, loneliness, depressive symptoms and sleep quality in people living with HIV. Psychol Health. 2018;33(3):398–415. https://doi.org/10.1080/08870446.2017.1357816.
Slopen N, Lewis TT, Williams DR. Discrimination and sleep: a systematic review. Sleep Med. 2016;18:88–95. https://doi.org/10.1016/j.sleep.2015.01.012.
Grandner MA, Hale L, Jackson N, Patel NP, Gooneratne NS, Troxel WM. Perceived racial discrimination as an independent predictor of sleep disturbance and daytime fatigue. Behav Sleep Med. 2012;10(4):235–49. https://doi.org/10.1080/15402002.2012.654548.
Park JB, Nakata A, Swanson NG, Chun H. Organizational factors associated with work-related sleep problems in a nationally representative sample of Korean workers. Int Arch Occup Environ Health. 2013;86(2):211–22. https://doi.org/10.1007/s00420-012-0759-3.
Mallampalli MP, Carter CL. Exploring sex and gender differences in sleep health: a Society for Women’s Health Research Report. Journal of Women’s Health. 2014;23(7):553–62. https://doi.org/10.1089/jwh.2014.4816.
Zoccola PM, Dickerson SS, Lam S. Rumination predicts longer sleep onset latency after an acute psychosocial stressor. Psychosom Med. 2009;71(7):771–5. https://doi.org/10.1097/PSY.0b013e3181ae58e8.
McLaughlin KA, Nolen-Hoeksema S. Rumination as a transdiagnostic factor in depression and anxiety. Behav Res Ther. 2011;49(3):186–93. https://doi.org/10.1016/j.brat.2010.12.006.
Johnson DP, Whisman MA. Gender differences in rumination: a meta-analysis. Personality Individ Differ. 2013;55(4):367–74. https://doi.org/10.1016/j.paid.2013.03.019.
Jansson-Fröjmark M, Lindblom K. A bidirectional relationship between anxiety and depression, and insomnia? A prospective study in the general population. J Psychosom Res. 2008;64(4):443–9. https://doi.org/10.1016/j.jpsychores.2007.10.016.
Buysse DJ, Reynolds CF III, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28(2):193–213. https://doi.org/10.1016/0165-1781(89)90047-4.
Cole JC, Motivala SJ, Buysse DJ, Oxman MN, Levin MJ, Irwin MR. Validation of a 3-factor scoring model for the Pittsburgh sleep quality index in older adults. Sleep. 2006;29(1):112–6. https://doi.org/10.1093/sleep/29.1.112.
Eaton WW, Smith C, Ybarra M, Muntaner C, Tien A. Center for EpidemiologicStudies Depression Scale: review and revision (CESD and CESD-R). 2004.
Grös DF, Antony MM, Simms LJ, McCabe RE. Psychometric properties of the state-trait inventory for cognitive and somatic anxiety (STICSA): comparison to the state-trait anxiety inventory (STAI). Psychol Assess. 2007;19(4):369. https://doi.org/10.1037/1040-3590.19.4.369.
Van D, Nicholas T, Daniel FG, Mitch E, and Martin MA. “Establishing a trait anxiety threshold that signals likelihood of anxiety disorders.” Anxiety, Stress & Coping 26, no. 1 2013; 70–86.
Hayes AF. Introduction to mediation, moderation, and conditional process analysis: a regression-based approach. Guilford Publications. 2017.
Hayes AF. The PROCESS macro for SPSS and SAS. 2015.
Brosschot JF, Gerin W, Thayer JF. The perseverative cognition hypothesis: a review of worry, prolonged stress-related physiological activation, and health. J Psychosom Res. 2006;60:113–24. https://doi.org/10.1016/j.jpsychores.2005.06.074.
Clark LA, Watson D. Tripartite model of anxiety and depression: psychometric evidence and taxonomic implications. J Abnorm Psychol. 1991;100(3):316.
Pillai V, Cheng P, Kalmbach DA, Roehrs T, Roth T, Drake CL. Prevalence and predictors of prescription sleep aid use among individuals with DSM-5 insomnia: the role of hyperarousal. Sleep. 2016;39(4):825–32. https://doi.org/10.5665/sleep.5636.
Kalmbach DA, Cuamatzi-Castelan AS, Tonnu CV, Tran KM, Anderson JR, Roth T, Drake CL. Hyperarousal and sleep reactivity in insomnia: current insights. Nature and Science of Sleep. 2018;10:193. https://doi.org/10.2147/NSS.S138823.
Woosley JA, Lichstein KL, Taylor DJ, Riedel BW, Bush AJ. Predictors of perceived sleep quality among men and women with insomnia. Behav Sleep Med. 2012;10(3):191–201. https://doi.org/10.1080/15402002.2012.666218.
Augner C. Associations of subjective sleep quality with depression score, anxiety, physical symptoms and sleep onset latency in young students. Cent Eur J Public Health. 2011;19(2):115–7. https://doi.org/10.21101/cejph.a3647.
Richter T, Fishbain B, Markus A, Richter-Levin G, Okon-Singer H. Using machine learning-based analysis for behavioral differentiation between anxiety and depression. Sci Rep. 2020;10(1):1–12. https://doi.org/10.1038/s41598-020-72289-9.
Beck AT. (Ed.). Cognitive therapy of depression. Guilford press. 1979.
Backhaus J, Junghanns K, Broocks A, Riemann D, Hohagen F. Test–retest reliability and validity of the Pittsburgh Sleep Quality Index in primary insomnia. J Psychosom Res. 2002;53(3):737–40. https://doi.org/10.1016/S0022-3999(02)00330-6.
Puhl RM, Telke S, Larson N, Eisenberg ME, Neumark-Stzainer D. Experiences of weight stigma and links with self-compassion among a population-based sample of young adults from diverse ethnic/racial and socio-economic backgrounds. J Psychosom Res. 2020;134: 110134. https://doi.org/10.1016/j.jpsychores.2020.110134.
Trauer JM, Qian MY, Doyle JS, Rajaratnam SM, Cunnington D. Cognitive behavioral therapy for chronic insomnia: a systematic review and meta-analysis. Ann Intern Med. 2015;163(3):191–204. https://doi.org/10.7326/M14-2841.
Funding
The project was self-funded using faculty development funds from EF.
Author information
Authors and Affiliations
Contributions
Both MC and EF were involved in data analysis and writing portions of the manuscript. EF was responsible for the study design and data collection.
Corresponding author
Ethics declarations
Ethics Approval
The study was approved as exempt from IRB review by the Human Subject Research Protection Program at the University of Indianapolis.
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Research Involving Human and Animal Participants
This article does not contain any studies with animals performed by any of the authors.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Craven, M.P., Fekete, E.M. Internalized Weight Stigma, Psychological Well-Being, and Sleep in Women. Int.J. Behav. Med. 29, 199–208 (2022). https://doi.org/10.1007/s12529-021-10008-y
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12529-021-10008-y