Abstract
Background
Prior to treatment, breast cancer patients are less physically fit compared to peers; during cancer treatment, their fitness typically declines. Depressive symptoms are associated with reduced activity up to 5 years post-treatment, but research has not identified mechanisms linking depression and lower activity. The current study assessed relationships among breast cancer patients’ depression and perceived exertion during exercise as well as heart rate, an objective indicator of exertion.
Methods
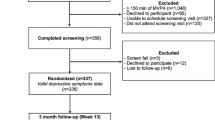
Participants were 106 breast cancer patients, stages I–IIIA, who completed surgery but had not started adjuvant treatment. Heart rate and self-rated exertion, measured using the Borg Scale of Perceived Exertion, were assessed every 2 min during a graded exercise test. Depression was assessed using the CES-D and a structured clinical interview.
Results
Compared to women below the CES-D clinical cutoff, women with significant depressive symptoms reported steeper increases in exertion during the exercise test (p = .010) but had similar heart rates (p = .224) compared to women below the cutoff. Major depression history was unrelated to perceived exertion (ps > .224) and heart rate (ps > .200) during exercise.
Conclusions
Women with currently elevated depressive symptoms experienced exercise as more difficult compared to women below the CES-D cutoff, but these self-perceptions did not reflect actual heart rate differences. Depression may make exercise feel more demanding, which could ultimately decrease patients’ likelihood of engaging in regular exercise. Results support the use of depression screening tools following breast cancer surgery to identify and intervene on individuals at risk for decreased physical activity during survivorship.

Similar content being viewed by others
References
Rock CL, Doyle C, Demark-Wahnefried W, Meyerhardt J, Courneya KS, Schwartz AL, et al. Nutrition and physical activity guidelines for cancer survivors. CA Cancer J Clin. 2012;62:242–74.
Ibrahim EM, Al-Homaidh A. Physical activity and survival after breast cancer diagnosis: meta-analysis of published studies. Med Oncol. 2011;28:753–65.
Phillips SM, Awick EA, Conroy DE, Pellegrini CA, Mailey EL, McAuley E. Objectively measured physical activity and sedentary behavior and quality of life indicators in survivors of breast cancer: activity sedentary time quality of life. Cancer. 2015;121:4044–52.
van Vulpen JK, Peeters PHM, Velthuis MJ, van der Wall E, May AM. Effects of physical exercise during adjuvant breast cancer treatment on physical and psychosocial dimensions of cancer-related fatigue: a meta-analysis. Maturitas. 2016;85:104–11.
Irwin ML, McTiernan A, Bernstein L, Gilliland FD, Baumgartner R, Baumgartner K, et al. Physical activity levels among breast cancer survivors. Med Sci Sports Exerc. 2004;36:1484–91.
Jones LW, Courneya KS, Mackey JR, Muss HB, Pituskin EN, Scott JM, et al. Cardiopulmonary function and age-related decline across the breast cancer survivorship continuum. J Clin Oncol. 2012;30:2530–7.
Jones LW, Habel LA, Weltzien E, Castillo A, Gupta D, Kroenke CH, et al. Exercise and risk of cardiovascular events in women with nonmetastatic breast cancer. J Clin Oncol. 2016;34:2743–9.
Christensen S, Zachariae R, Jensen AB, Vaeth M, Moller S, Ravnsbaek J, et al. Prevalence and risk of depressive symptoms 3-4 months post-surgery in a nationwide cohort study of Danish women treated for early stage breast-cancer. Breast Cancer Res Treat. 2009;113:339–55.
Golden-Kreutz DM, Andersen BL. Depressive symptoms after breast cancer surgery: relationships with global, cancer-related, and life event stress. Psycho-Oncology. 2004;13:211–20.
Emery CF, Yang H-C, Frierson GM, Peterson LJ, Suh S. Determinants of physical activity among women treated for breast cancer in a 5-year longitudinal follow-up investigation. Psycho-Oncology. 2009;18:377–86.
Hong S, Bardwell WA, Natarajan L, Flatt SW, Rock CL, Newman VA, et al. Correlates of physical activity level in breast cancer survivors participating in the Women’s Healthy Eating and Living (WHEL) Study. Breast Cancer Res Treat. 2007;101:225–32.
Beck AT. Depression: clinical, experimental, and theoretical aspects. New York: Harper & Row; 1967.
Beck AT. The evolution of the cognitive model of depression and its neurobiological correlates. Am J Psychiatry. 2008;165:969–77.
Wiech K, Tracey I. The influence of negative emotions on pain: behavioral effects and neural mechanisms. NeuroImage. 2007;47:987–94.
Adler G, Gattaz WF. Pain perception threshold in major depression. Biol Psychiatry. 1993;34:687–9.
Dickens C, McGowan L, Dale S. Impact of depression on experimental pain perception: a systematic review of the literature with meta-analysis. Psychosom Med. 2003;65:369–75.
Euteneuer F, Schwarz MJ, Hennings A, Riemer S, Stapf T, Selberdinger V, et al. Depression, cytokines and experimental pain: evidence for sex-related association patterns. J Affect Disord. 2011;131:143–9.
Hermesdorf M, Berger K, Baune BT, Wellmann J, Ruscheweyh R, Wersching H. Pain sensitivity in patients with major depression: differential effect of pain sensitivity measures, somatic cofactors, and disease characteristics. J Pain. 2016;17:606–16.
Harshaw C. Interoceptive dysfunction: toward an integrated framework for understanding somatic and affective disturbance in depression. Psychol Bull. 2015;141:311–63.
Kibler JL, Ma M. Depressive symptoms and cardiovascular reactivity to laboratory behavioral stress. Int J Behav Med. 2004;11:81–7.
Carroll D, Phillips AC, Hunt K, Der G. Symptoms of depression and cardiovascular reactions to acute psychological stress: evidence from a population study. Biol Psychol. 2007;75:68–74.
Phillips AC, Hunt K, Der G, Carroll D. Blunted cardiac reactions to acute psychological stress predict symptoms of depression five years later: evidence from a large community study. Psychophysiology. 2011;48:142–8.
York KM, Hassan M, Li Q, Li H, Fillingim RB, Sheps DS. Coronary artery disease and depression: patients with more depressive symptoms have lower cardiovascular reactivity during laboratory-induced mental stress. Psychosom Med. 2007;69:521–8.
Lavoie KL, Fleet RP, Lespérance F, Arsenault A, Laurin C, Frasure-Smith N, et al. Are exercise stress tests appropriate for assessing myocardial ischemia in patients with major depressive disorder? Am Heart J. 2004;148:621–7.
Pelletier R, Lavoie KL, Gordon J, Arsenault A, Campbell TS, Bacon SL. The role of mood disorders in exercise-induced cardiovascular reactivity. Psychosom Med. 2009;71:301–7.
Eriksen L, Grønbaek M, Helge JW, Tolstrup JS. Cardiorespiratory fitness in 16,025 adults aged 18-91 years and associations with physical activity and sitting time. Scand J Med Sci Sports. 2015.
Balady GJ, Arena R, Sietsema K, Myers J, Coke L, Fletcher GF, et al. Clinician’s guide to cardiopulmonary exercise testing in adults: a scientific statement from the American Heart Association. Circulation. 2010;122:191–225.
Borg G. Pyschophysical bases of perceived exertion. Med Sci Sports Exerc. 1982;14:377–81.
Borg G. Borg’s perceived exertion and pain scales. Champaign: Human Kinetics; 1998.
Chen MJ, Fan XT, Moe ST. Criterion-related validity of the Borg ratings of perceived exertion scale in healthy individuals: a meta-analysis. J Sports Sci. 2002;20:873–99.
Radloff LS. The CES-D scale. Appl Psychol Meas. 1977;1:385–401.
Hann D, Winter K, Jacobsen P. Measurement of depressive symptoms in cancer patients: evaluation of the Center for Epidemiological Studies Depression Scale (CES-D). J Psychosom Res. 1999;46:437–43.
Lewinsohn PM, Seeley JR, Roberts RE, Allen NB. Center for Epidemiologic Studies Depression Scale (CES-D) as a screening instrument for depression among community-residing older adults. Psychol Aging. 1997;12:277–87.
First MB, Spitzer RL, Gibbon M, Williams JBW. Structured clinical interview for DSM-IV-TR axis I disorders, research version, non-patient edition. (SCID-I/NP). New York: Biometrics Research, New York State Psychiatric Institute; 2002.
Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–83.
Charlson M, Szatrowski TP, Peterson J, Gold J. Validation of a combined comorbidity index. J Clin Epidemiol. 1994;47:1245–51.
Klabunde CN, Legler JM, Warren JL, Baldwin LM, Schrag D. A refined comorbidity measurement algorithm for claims-based studies of breast, prostate, colorectal, and lung cancer patients. Ann Epidemiol. 2007;17:584–90.
Godin G, Shephard RJ. A simple method to assess exercise behavior in the community. Can J Appl Sport Sci. 1985;10:141–6.
Amireault S, Godin G, Lacombe J, Sabiston CM. Validation of the Godin-Shephard Leisure-Time Physical Activity Questionnaire classification coding system using accelerometer assessment among breast cancer survivors. J Cancer Surviv. 2015;9:532–40.
Everaert J, Koster EHW, Derakshan N. The combined cognitive bias hypothesis in depression. Clin Psychol Rev. 2012;32:413–24.
Joormann J, D’Avanzato C. Emotion regulation in depression: examining the role of cognitive processes. Cogn Emot. 2010;24:913–39.
Terhaar J, Viola FC, Bär K-J, Debener S. Heartbeat evoked potentials mirror altered body perception in depressed patients. Clin Neurophysiol. 2012;123:1950–7.
Furman DJ, Waugh CE, Bhattacharjee K, Thompson RJ, Gotlib IH. Interoceptive awareness, positive affect, and decision making in major depressive disorder. J Affect Disord. 2013;151:780–5.
Wiebking C, de Greck M, Duncan NW, Tempelmann C, Bajbouj M, Northoff G. Interoception in insula subregions as a possible state marker for depression—an exploratory fMRI study investigating healthy, depressed and remitted participants. Front Behav Neurosci. 2015;9.
Blanchfield A, Hardy J, Marcora S. Non-conscious visual cues related to affect and action alter perception of effort and endurance performance. Front Hum Neurosci. 2014;8.
Viana BF, Pires FO, Inoue A, Micklewright D, Santos TM. Correlates of mood and RPE during multi-lap off-road cycling. Appl Psychophysiol Biofeedback. 2016;41:1–7.
Stults-Kolehmainen MA, Lu T, Ciccolo JT, Bartholomew JB, Brotnow L, Sinha R. Higher chronic psychological stress is associated with blunted affective responses to strenuous resistance exercise: RPE, pleasure, pain. Psychol Sport Exerc. 2016;22:27–36.
Hemmis L, de Vries H, Vandelanotte C, Short CE, Duncan MJ, Burton NW, et al. Depressive symptoms associated with psychological correlates of physical activity and perceived helpfulness of intervention features. Ment Health and Phys Act. 2015;9:16–23.
Maeda U, Shen B-J, Schwarz ER, Farrell KA, Mallon S. Self-efficacy mediates the associations of social support and depression with treatment adherence in heart failure patients. Int J Behav Med. 2013;20:88–96.
Risch AK, Buba A, Birk U, Morina N, Steffens MC, Stangier U. Implicit self-esteem in recurrently depressed patients. J Behav Ther Exp Psychiatry. 2010;41:199–206.
Neupert SD, Lachman ME, Whitbourne SB. Exercise self-efficacy and control beliefs predict exercise behavior after an exercise intervention for older adults. J Aging Phys Act. 2009;17:1–16.
Godin G, Valois P, Lepage L. The pattern of influence of perceived behavioral control upon exercising behavior: an application of Ajzen’s theory of planned behavior. J Behav Med. 1993;16:81–102.
Pomp S, Fleig L, Schwarzer R, Lippke S. Depressive symptoms interfere with post-rehabilitation exercise: outcome expectancies and experience as mediators. Psychol Health Med. 2012;17:698–708.
Greenwald AG, Banaji MR. Implicit social cognition: attitudes, self-esteem, and stereotypes. Psychol Rev. 1995;102:4–27.
Lonigan CJ, Vasey MW. Negative affectivity, effortful control, and attention to threat-relevant stimuli. J Abnorm Child Psychol. 2009;37:387–99.
Strauman TJ. Self-regulation and depression. Self Identity. 2002;1:151–7.
Carver CS, Johnson SL, Joormann J. Serotonergic function, two-mode models of self-regulation, and vulnerability to depression: what depression has in common with impulsive aggression. Psychol Bull. 2008;134:912–43.
Padin AC, Emery CF, Vasey M, Kiecolt-Glaser JK. Self-regulation and implicit attitudes toward physical activity influence exercise behavior. J Sport Exerc Psychol. 2017;39:237–48.
Holland JC, Andersen B, Breitbart WS, Buchmann LO, Compas B, Deshields TL, et al. Distress management: clinical practice guidelines in oncology. J Natl Compr Cancer Netw. 2013;11:190–209.
Chase J-AD, Conn VS. Meta-analysis of fitness outcomes from motivational physical activity interventions. Nurs Res. 2013;62:294–304.
Josefsson T, Lindwall M, Archer T. Physical exercise intervention in depressive disorders: meta-analysis and systematic review. Scand J Med Sci Sports. 2014;24:259–72.
Schoeny ME, Fogg L, Buchholz SW, Miller A, Wilbur J. Barriers to physical activity as moderators of intervention effects. Prev Med Rep. 2017;5:57–64.
Anderson RT, Kimmick GG, McCoy TP, Hopkins J, Levine E, Miller G, et al. A randomized trial of exercise on well-being and function following breast cancer surgery: the RESTORE trial. J Cancer Surviv. 2012;6:172–81.
McNeely ML, Campbell K, Ospina M, Rowe BH, Dabbs K, Klassen TP, et al. Exercise interventions for upper-limb dysfunction due to breast cancer treatment. Cochrane Database Syst Rev. 2010:CD005211.
Furmaniak AC, Menig M, Markes MH. Exercise for women receiving adjuvant therapy for breast cancer. Cochrane Database Syst Rev. 2016;9:CD005001.
Funding
This work was supported in part by the National Institutes of Health grant nos. R01 CA186720, UL1TR001070, K05 CA172296, T32 DE014320, and a Pelotonia Postdoctoral Fellowship from Ohio State University’s Comprehensive Cancer Center. The first author also receives support from the National Institutes of Health grant no. R01 CA186720-02S2, and the third author receives support from the National Institutes of Health grant no. R01 CA186720-02S1.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Conflict of Interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Padin, A.C., Wilson, S.J., Bailey, B.E. et al. Physical Activity After Breast Cancer Surgery: Does Depression Make Exercise Feel More Effortful than It Actually Is?. Int.J. Behav. Med. 26, 237–246 (2019). https://doi.org/10.1007/s12529-019-09778-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12529-019-09778-3