Abstract
Purpose
Although poor oral hygiene practices can have serious health consequences, a large number of adults brush or floss their teeth less than the recommended time or not at all. This study examined the mediating effect of two key self-regulatory processes, self-efficacy and planning, as the mechanisms that translate dental flossing intentions into behavior.
Method
Participants (N = 629) comprised young adults attending a major university in Queensland, Australia. A longitudinal design guided by sound theory was adopted to investigate the sequential mediation chain for the effect of dental flossing intentions (time 1) on behavior (time 3) via self-efficacy and planning (time 2).
Results
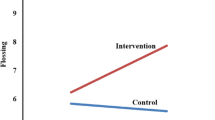
A latent variable structural equation model with standardized parameter estimates revealed the model was a good fit to the data. Controlling for baseline flossing, the effect of intentions on behavior was mediated via self-efficacy and planning, with 64 % of the flossing variance accounted for by this set of predictors. Controlling for age and sex did not change the results.
Conclusion
The results extend previous research to further elucidate the mechanisms that help to translate oral hygiene intentions into behavior and make a significant contribution to the cumulative empirical evidence about self-regulatory components in health behavior change.

Similar content being viewed by others
References
World Health Organisation. Oral health [Internet]. 2012 [cited 2015 26 March]. Available from: http://www.who.int/mediacentre/factsheets/fs318/en/.
Gharat AR. Periodontitis and diabetes—a complex relationship. Int J Diabetes Dev Ctries. 2011;3:128–32.
Scannapieco F, Ho A. Potential associations between chronic respiratory disease and periodontal disease: analysis of national health and nutrition examination survey III. J Periodontol. 2001;72:50–6.
Meyer MS, Joshipura K, Giovannucci E, Michaud DS. A review of the relationship between tooth loss, periodontal disease, and cancer. Cancer Causes Control. 2008;19:895–907.
Australian Institute of Health and Welfare. Australia’s health 2014. Canberra: AIHW; 2014. Australia’s health series no 14.
Australian Institute of Health and Welfare. Oral health and dental care in Australia: key facts and figures trends 2014. Canberra: AIHW; 2014.
Petersen P. World Health Organization global policy for improvement of oral health—World Health Assembly 2007. Int Dent J. 2008;58:115–21.
Sambunjak D, Nickerson J, Poklepovic T, Johnson T, Imai P, Tugwell P, et al. Flossing for the management of periodontal diseases and dental caries in adults. Cochrane Database Syst Rev. 2011;12:Cd008829.
Tonetti M, Eickholz P, Loos B, Papapanou P, van der Velden U, Armitage G, et al. Principles in prevention of periodontal diseases. J Clin Periodontol. 2015;42:S5–S11.
American Dental Association. Mouth Healthy. Flossing [Internet]. 2015 [cited 2015 30 November]. Available from: http://www.mouthhealthy.org/en/az-topics/f/flossing.
Australian Dental Association. Tooth decay—Australia’s most prevalent health condition [Internet]. 2012 [cited 2016]. Available from: http://www.ada.org.au/app_cmslib/media/lib/1207/m422161_v1_tooth_decay-australias_most_prevalent_health_condition.pdf.
Buunk-Werkhoven Y, Dijkstra A, van der Schans C. Determinants of oral hygiene behavior: a study based on the theory of planned behavior. Community Dent Oral Epidemiol. 2011;39:250–9.
Gholami M, Knoll N, Schwarzer R. A brief self-regulatory intervention increases dental flossing in adolescent girls. Int J Behav Med. 2015;22:645–51.
Lavin D, Groarke A. Dental floss behaviour: a test of the predictive utility of the theory of planned behaviour and the effects of making implementation intentions. Psychol Health Med. 2005;10:243–52.
Rise J, Åstrøm A, Sutton S. Predicting intentions and use of dental floss among adolescents: an application of the theory of planned behaviour. Psychol Health. 1998;13:223–36.
Schüz B, Sniehotta F, Wiedermann A, Seemann R. Adherence to a daily flossing regimen in university students: effects of planning when, where, how and what to do in the face of barriers. J Clin Periodontol. 2006;33:612–9.
Scheerman JFM, Loveren C, van Meijel B, Dusseldorp E, Wartewig E, Verrips GHW, et al. Psychosocial correlates of oral hygiene behaviour in people aged 9 to 19—a systematic review with meta-analysis. J Community Density and Oral Epidemiology. doi:10.1111/cdoe.12224.
Ellershaw A, Spencer A. Dental attendance patterns and oral health status. Canberra; AIHW; 2011. Dental statistics and research series no. 57 Cat. No. DEN 208.
Sheeran P, Webb TL, Gollwitzer PM. The interplay between goal intentions and implementation intentions. Personal Soc Psychol Bull. 2005;31:87–98.
Schwarzer R. Modeling health behavior change: how to predict and modify the adoption and maintenance of health behaviors. Appl Psychol Int Rev. 2008;57:1–29.
Schwarzer R, Luszczynska A. Health action process approach. In Conner M, Norman P, editors: Predicting and changing health behavior: research and practice with social cognition models. 3rd ed. Oxford University Press; 2015.
Hamilton K, Cox S, White K. Testing a model of physical activity among mothers and fathers of young children: integrating self-determined motivation, planning, and the theory of planned behavior. J Sport Exerc Psychol. 2012;34:124–45.
Zhou G, Gan Y, Miao M, Hamilton K, Knoll N, Schwarzer R. The role of action control and action planning on fruit and vegetable consumption. Appetite. 2015;91:64–8.
Reyes Fernández B, Knoll N, Hamilton K, Schwarzer R. Social-cognitive antecedents of hand washing: action control bridges the planning-behavior gap. Psychol Health. 2016. doi:10.1080/08870446.2016.1174236.
Hamilton K, Vayro C, Schwarzer R. Social-cognitive antecedents of fruit and vegetable consumption in truck drivers: a sequential mediation analysis. J Nutr Educ Behav. 2015;47:379–84.
Hamilton K, Warner L, Schwarzer R. The role of self-efficacy and friend support on adolescent intentions and vigorous exercise. Health Educ Behav. 2016. doi:10.1177/1090198116648266.
Lhakhang P, Gholami M, Knoll N, Schwarzer R. Comparing a motivational and a self-regulatory intervention to adopt an oral self-care regimen: a two-sequential randomized crossover trial. Psychol Health Med. 2015;20:381–92.
Schüz B, Sniehotta FF, Mallach N, Wiedemann AU, Schwarzer R. Predicting transitions from preintentional, intentional and actional stages of change: adherence to oral self-care recommendations. Health Educ Res. 2009;24:64–75.
Zhou G, Sun C, Knoll N, Hamilton K, Schwarzer R. Self-efficacy, planning, and action control in an oral self-care intervention. Health Educ Research. 2015;30:671–81.
Lhakhang P, Hamilton K, Sud N, Sud S, Kroon J, Knoll N, Schwarzer R. Combining self-management cues with incentives to promote interdental cleaning among Indian periodontal disease outpatients. BMC Oral Health. 2016;16:6. doi:10.1186/s12903-016-0164-5.
Schwarzer R, Renner B. Social-cognitive predictors of health behavior: action self-efficacy and coping self-efficacy. Health Psychol. 2000;19:487–95.
Gillholm R, Ettema D, Selart M, Garling T. The role of planning for intention-behavior consistency. Scand J Psycho. 1999;40:241–50.
Orbell S, Hodgkins S, Sheeran P. Implementation intentions and the theory of planned behavior. Pers Soc Psycholol Bull. 1997;23:945–54.
Kwasnicka D, Presseau J, White M, Sniehotta F. Does planning how to cope with anticipated barriers facilitate health-related behavior change? A systematic review. Health Psychol Rev. 2013;7:129–45.
Sniehotta FF, Schwarzer R, Scholz U, Schüz B. Action planning and coping planning for long-term lifestyle change: theory and assessment. Eur J Soc Psychol. 2005;35:565–76.
Ashford S, Edmunds J, French DP. What is the best way to change self-efficacy to promote lifestyle and recreational physical activity? A systematic review with meta-analysis. Br J Health Psychol. 2010;15:265–88.
Gollwitzer PM, Sheeran P. Implementation intentions and goal achievement: a meta-analysis of effects and processes. Adv Exp Soc Psychol. 2006;38:69–119.
Anagnostopoulos F, Buchanan H, Frousiounioti S, Niakas D, Potamianos G. Self-efficacy and oral hygiene beliefs about toothbrushing in dental patients: a model-guided study. Behav Med. 2011;37:132–9.
Buglar ME, White KM, Robinson NG. The role of self-efficacy in dental patients’ brushing and flossing: testing an extended health belief model. Patient Educ Couns. 2010;78:269–72.
Mizutani S, Ekuni D, Furuta M, Tomofuji T, Irie K, Azuma T, et al. Effects of self-efficacy on oral health behaviours and gingival health in university students aged 18 or 19 years old. J Clin Periodontol. 2012;39:844–9.
Pakpour AH, Sniehotta FF. Perceived behavioral control and coping planning predict dental brushing behavior among Iranian adolescents. J Clin Periodontol. 2012;39:132–7.
Bandura A. Self-efficacy: the exercise of control. New York: Freeman; 1997.
Hagger MS, Luszczynska A. Implementation intention and action planning interventions in health contexts: state of the research and proposals for the way forward. Appl Psychol Health Well Being. 2014;6:1–47.
Hayes A. Introduction to mediation, moderation, and conditional process analysis: a regression-based approach. New York: Guilford Press; 2013.
Muthén LK, Muthén BO. Mplus user’s guide. 7th ed. Muthén & Muthén: Los Angeles, CA; 2015.
Petersen PE, Ogawa H. The global burden of periodontal disease: towards integration with chronic disease prevention and control. Periodontol. 2012;60:15–39.
Luszczynska A, Schwarzer R. Planning and self-efficacy in the adoption and maintenance of breast self-examination: a longitudinal study on self-regulatory cognitions. Psychol Health. 2003;18:93–108.
Allan JL, Sniehotta FF, Johnston M. The best laid plans: planning skill determines the effectiveness of action plans and implementation intentions. Ann Behav Med. 2013;46:114–20.
Doran GT. There’s a S.M.A.R.T. way to write management’s goals and objectives. Manage Rev (AMA FORUM). 1981;70:35–6.
Gollwitzer PM. Implementation intentions: strong effects of simple plans. Am Psychol. 1999;54:493–503.
Goodwin CJ. Research in psychology: methods and design. USA: John Wiley & Sons; 2009.
Schüz B, Sniehotta F, Schwarzer R. Stage-specific effects of an action control intervention on dental flossing. Health Educ Res. 2007;22:332–41.
Orbell S, Verplanken B. The automatic component of habit in health behavior: habit as cue-contingent automaticity. Health Psychol. 2010;29:374–83.
Young AF, Powers JR, Bell SL. Attrition in longitudinal studies: who do you lose? ANZJPH. 2006;30:353–61.
McGinley S, Zhang L, Hanks L, O’Neill J. Reducing longitudinal attrition through Facebook. J Hosp Mark Manage. 2015;24:894–900.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Rights and permissions
About this article
Cite this article
Hamilton, K., Bonham, M., Bishara, J. et al. Translating Dental Flossing Intentions into Behavior: a Longitudinal Investigation of the Mediating Effect of Planning and Self-Efficacy on Young Adults. Int.J. Behav. Med. 24, 420–427 (2017). https://doi.org/10.1007/s12529-016-9605-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12529-016-9605-4