Abstract
Background
Comprehensive quantitative evidence on the risk and protective factors for sudden infant death syndrome (SIDS) effects is lacking. We investigated the risk and protective factors related to SIDS.
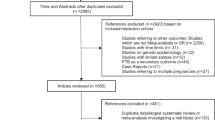
Methods
We conducted an umbrella review of meta-analyses of observational and interventional studies assessing SIDS-related factors. PubMed/MEDLINE, Embase, EBSCO, and Google Scholar were searched from inception until January 18, 2023. Data extraction, quality assessment, and certainty of evidence were assessed by using A Measurement Tool Assessment Systematic Reviews 2 following PRISMA guidelines. According to observational evidence, credibility was graded and classified by class and quality of evidence (CE; convincing, highly suggestive, suggestive, weak, or not significant). Our study protocol was registered with PROSPERO (CRD42023458696). The risk and protective factors related to SIDS are presented as equivalent odds ratios (eORs).
Results
We identified eight original meta-analyses, including 152 original articles, covering 12 unique risk and protective factors for SIDS across 21 countries/regions and five continents. Several risk factors, including prenatal drug exposure [eOR = 7.84 (95% CI = 4.81–12.79), CE = highly suggestive], prenatal opioid exposure [9.55 (95% CI = 4.87–18.72), CE = suggestive], prenatal methadone exposure [9.52 (95% CI = 3.34–27.10), CE = weak], prenatal cocaine exposure [4.38 (95% CI = 1.95–9.86), CE = weak], prenatal maternal smoking [2.25 (95% CI = 1.95–2.60), CE = highly suggestive], postnatal maternal smoking [1.97 (95% CI = 1.75–2.22), CE = weak], bed sharing [2.89 (95% CI = 1.81–4.60), CE = weak], and infants found with heads covered by bedclothes after last sleep [11.01 (95% CI = 5.40–22.45), CE = suggestive], were identified. On the other hand, three protective factors, namely, breastfeeding [0.57 (95% CI = 0.39–0.83), CE = non-significant], supine sleeping position [0.48 (95% CI = 0.37–0.63), CE = suggestive], and pacifier use [0.44 (95% CI = 0.30–0.65), CE = weak], were also identified.
Conclusions
Based on the evidence, we propose several risk and protective factors for SIDS. This study suggests the need for further studies on SIDS-related factors supported by weak credibility, no association, or a lack of adequate research.
Graphical abstract


Similar content being viewed by others
Data availability
The data used in this review was derived from publicly available systematic reviews and meta-analyses.
References
Matthews T. Sudden unexpected infant death: infanticide or SIDS? Lancet. 2005;365:3–4.
Willinger M, James LS, Catz C. Defining the sudden infant death syndrome (SIDS): deliberations of an expert panel convened by the National Institute of Child Health and Human Development. Pediatr Pathol. 1991;11:677–84.
Mortality in the United States, 2021. 2022. https://www.cdc.gov/nchs/products/databriefs/db456.htm#section_4. Accessed 19 Jan 2024.
Park S, Han JH, Hwang J, Yon DK, Lee SW, Kim JH, et al. The global burden of sudden infant death syndrome from 1990 to 2019: a systematic analysis from the Global Burden of Disease study 2019. QJM. 2022;115:735–44.
Glinge C, Rossetti S, Oestergaard LB, Stampe NK, Lynge TH, Skals R, et al. Risk of sudden infant death syndrome among siblings of children who died of sudden infant death syndrome in Denmark. JAMA Netw Open. 2023;6:e2252724.
Makarious L, Teng A, Oei JL. SIDS is associated with prenatal drug use: a meta-analysis and systematic review of 4 238 685 infants. Arch Dis Child Fetal Neonatal Ed. 2022;107:617–23.
Zhang K, Wang X. Maternal smoking and increased risk of sudden infant death syndrome: a meta-analysis. Leg Med (Tokyo). 2013;15:115–21.
Kihal-Talantikite W, Marchetta GP, Deguen S. Infant mortality related to NO2 and PM exposure: systematic review and meta-analysis. Int J Environ Res Public Health. 2020;17:2623.
Blair PS, Mitchell EA, Heckstall-Smith EM, Fleming PJ. Head covering-a major modifiable risk factor for sudden infant death syndrome: a systematic review. Arch Dis Child. 2008;93:778–83.
Vennemann MM, Hense HW, Bajanowski T, Blair PS, Complojer C, Moon RY, et al. Bed sharing and the risk of sudden infant death syndrome: can we resolve the debate? J Pediatr. 2012;160:44–8.e2.
Priyadarshi M, Balachander B, Sankar MJ. Effect of sleep position in term healthy newborns on sudden infant death syndrome and other infant outcomes: a systematic review. J Glob Health. 2022;12:12001.
Hauck FR, Thompson JM, Tanabe KO, Moon RY, Vennemann MM. Breastfeeding and reduced risk of sudden infant death syndrome: a meta-analysis. Pediatrics. 2011;128:103–10.
Hauck FR, Omojokun OO, Siadaty MS. Do pacifiers reduce the risk of sudden infant death syndrome? A meta-analysis. Pediatrics. 2005;116:e716–23.
Lee SW, Koo MJ. PRISMA 2020 statement and guidelines for systematic review and meta-analysis articles, and their underlying mathematics: life Cycle Committee Recommendations. Life Cycle. 2022;2:e9.
Fusar-Poli P, Radua J. Ten simple rules for conducting umbrella reviews. Evid Based Ment Health. 2018;21:95–100.
Murad MH, Wang Z, Chu H, Lin L. When continuous outcomes are measured using different scales: guide for meta-analysis and interpretation. BMJ. 2019;364:k4817.
Lee JS, Lee YA, Shin CH, Suh DI, Lee YJ, Yon DK. Long-term health outcomes of early menarche in women: an umbrella review. QJM. 2022;115:837–47.
Lee SW. Methods for testing statistical differences between groups in medical research: statistical standard and guideline of Life Cycle Committee. Life Cycle. 2022;2:e1.
Solmi M, Toffol MD, Kim JY, Choi MJ, Stubbs B, Thompson T, et al. Balancing risks and benefits of cannabis use: umbrella review of meta-analyses of randomised controlled trials and observational studies. BMJ. 2023;382:e072348.
Lee K, Lee H, Kwon R, Shin YH, Yeo SG, Lee YJ, et al. Global burden of vaccine-associated anaphylaxis and their related vaccines, 1967–2023: a comprehensive analysis of the international pharmacovigilance database. Allergy. 2023. https://doi.org/10.1111/all.15968.
Hahn JW, Yang HR, Moon JS, Chang JY, Lee K, Kim GA, et al. Global incidence and prevalence of autoimmune hepatitis, 1970–2022: a systematic review and meta-analysis. EClinicalMedicine. 2023;65:102280.
Yon DK, Hwang S, Lee SW, Jee HM, Sheen YH, Kim JH, et al. Indoor exposure and sensitization to formaldehyde among inner-city children with increased risk for asthma and rhinitis. Am J Respir Crit Care Med. 2019;200:388–93.
Heathfield LJ, Martin LJ, van der Heyde Y, Molefe I, Ramesar R. Clinical exome sequencing elucidates underlying cause of death in sudden unexpected death of infants: two case reports. Int J Legal Med. 2024;138:693–700.
Chang C, Vivekanandarajah A, Waters KA, Machaalani R. Cell death in the lateral geniculate nucleus, and its possible relationship with nicotinic receptors and sudden infant death syndrome (SIDS). Mol Neurobiol. 2023;60:4120–31.
Spinelli J, Collins-Praino L, Van Den Heuvel C, Byard RW. Evolution and significance of the triple risk model in sudden infant death syndrome. J Paediatr Child Health. 2017;53:112–5.
Lee JS, Shin JI, Kim S, Choi YS, Shin YH, Hwang J, et al. Breastfeeding and impact on childhood hospital admissions: a nationwide birth cohort in South Korea. Nat Commun. 2023;14:5819.
Lavezzi AM. A new theory to explain the underlying pathogenetic mechanism of sudden infant death syndrome. Front Neurol. 2015;6:220.
Abu Y, Roy S. Prenatal opioid exposure and vulnerability to future substance use disorders in offspring. Exp Neurol. 2021;339:113621.
Moon RY, Carlin RF, Hand I. Sleep-related infant deaths: updated 2022 recommendations for reducing infant deaths in the sleep environment. Pediatrics. 2022;150:e2022057990.
Salihu HM, Wilson RE. Epidemiology of prenatal smoking and perinatal outcomes. Early Hum Dev. 2007;83:713–20.
Shin YH, Shin JI, Moon SY, Jin HY, Kim SY, Yang JM, et al. Autoimmune inflammatory rheumatic diseases and COVID-19 outcomes in South Korea: a nationwide cohort study. Lancet Rheumatol. 2021;3:e698–706.
McGrath-Morrow SA, Gorzkowski J, Groner JA, Rule AM, Wilson K, Tanski SE, et al. The effects of nicotine on development. Pediatrics. 2020;145:e20191346.
de Visme S, Korevaar DA, Gras-Le Guen C, Flamant A, Bevacqua M, Stanzelova A, et al. Inconsistency between pictures on baby diaper packaging in Europe and safe infant sleep recommendations. J Pediatr. 2023;264:113763.
Harrington CT, Hafid NA, Waters KA. Butyrylcholinesterase is a potential biomarker for sudden infant death syndrome. EBioMedicine. 2022;80:104041.
Shin H, Park S, Yon H, Ban CY, Turner S, Cho SH, et al. Estimated prevalence and trends in smoking among adolescents in South Korea, 2005–2021: a nationwide serial study. World J Pediatr. 2023;19:366–77.
Kim M, Rhee SY. Trends in prevalence of smoking in South Korea, 2014–2021: a post-hoc secondary analysis. Life Cycle. 2023;3:e14.
Perrone S, Lembo C, Moretti S, Prezioso G, Buonocore G, Toscani G, et al. Sudden infant death syndrome: beyond risk factors. Life (Basel). 2021;11:184.
Tappin D, Mitchell EA, Carpenter J, Hauck F, Allan L. Bed-sharing is a risk for sudden unexpected death in infancy. Arch Dis Child. 2023;108:79–80.
Marinelli KA, Ball HL, McKenna JJ, Blair PS. An integrated analysis of maternal-infant sleep, breastfeeding, and sudden infant death syndrome research supporting a balanced discourse. J Hum Lact. 2019;35:510–20.
Scragg RK, Mitchell EA, Stewart AW, Ford RP, Taylor BJ, Hassall IB, et al. Infant room-sharing and prone sleep position in sudden infant death syndrome. New Zealand Cot Death Study Group. Lancet. 1996;347:7–12.
Nelson EA, Yu LM, Wong D, Wong HY, Yim L. Rolling over in infants: age, ethnicity, and cultural differences. Dev Med Child Neurol. 2004;46:706–9.
Smith RW, Colpitts M. Pacifiers and the reduced risk of sudden infant death syndrome. Paediatr Child Health. 2020;25:205–6.
Kinney HC. Abnormalities of the brainstem serotonergic system in the sudden infant death syndrome: a review. Pediatr Dev Pathol. 2005;8:507–24.
Tong S, Colditz P. Air pollution and sudden infant death syndrome: a literature review. Paediatr Perinat Epidemiol. 2004;18:327–35.
Shaefer SJ. Review finds that bed sharing increases risk of sudden infant death syndrome. Evid Based Nurs. 2012;15:115–6.
Carlin RF, Moon RY. Risk factors, protective factors, and current recommendations to reduce sudden infant death syndrome: a review. JAMA Pediatr. 2017;171:175–80.
Dahl K, Andersen M, Henriksen TB. Association between auditory system pathology and sudden infant death syndrome (SIDS): a systematic review. BMJ Open. 2021;11:e055318.
Goldberg N, Rodriguez-Prado Y, Tillery R, Chua C. Sudden infant death syndrome: a review. Pediatr Ann. 2018;47:e118–23.
Pease A, Turner N, Ingram J, Fleming P, Patrick K, Williams T, et al. Changes in background characteristics and risk factors among SIDS infants in England: cohort comparisons from 1993 to 2020. BMJ Open. 2023;13:e076751.
Moon RY, Carlin RF, Hand I. Evidence base for 2022 updated recommendations for a safe infant sleeping environment to reduce the risk of sleep-related infant deaths. Pediatrics. 2022;150:e2022057991.
Kim JH, Kim JY, Lee J, Jeong GH, Lee E, Lee S, et al. Environmental risk factors, protective factors, and peripheral biomarkers for ADHD: an umbrella review. Lancet Psychiatry. 2020;7:955–70.
IntHout J, Ioannidis JP, Borm GF. The Hartung-Knapp-Sidik-Jonkman method for random effects meta-analysis is straightforward and considerably outperforms the standard DerSimonian-Laird method. BMC Med Res Methodol. 2014;14:25.
Funding
This research was supported by the National Research Foundation of Korea (NRF) grant funded by the Korea government (MSIT; RS-2023-00248157). The funding agencies had no role in the design and conduct of the study: collection, management, analysis, or interpretation of the data; preparation, review, or approval of the manuscript; and the decision to submit the manuscript for publication.
Author information
Authors and Affiliations
Contributions
KTH and LHyeri contributed equally to this work as co-first authors. KJ and YDK contributed equally to this work as co-corresponding authors. KTH, LHyeri, KJ, and YDK contributed to study concept and design, acquisition, analysis, or interpretation of data, drafting of the manuscript, statistical analysis, and study supervision. YDK had full access to all of the data in the study and took responsibility for the integrity of the data and the accuracy of the data analysis, and is the guarantor for this study. All authors contributed to critical revision of the manuscript for important intellectual content and approved the final version before submission. The corresponding authors attest that all listed authors meet authorship criteria and that no others meeting the criteria have been omitted.
Corresponding authors
Ethics declarations
Ethical approval
This systematic review article does not require Institutional Review Board approval. Our systematic review and meta-analysis protocol were registered with PROSPERO (registration number: CRD42023458696).
Conflict of interest
No financial or non-financial benefits have been received or will be received from any party related directly or indirectly to the subject of this article. The authors have no conflict of interest to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kim, T.H., Lee, H., Woo, S. et al. Prenatal and postnatal factors associated with sudden infant death syndrome: an umbrella review of meta-analyses. World J Pediatr (2024). https://doi.org/10.1007/s12519-024-00806-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12519-024-00806-1