Abstract
Background
The intrauterine environment has a profound and long-lasting influence on the health of the offspring. However, its impact on the postnatal catch-up growth of twin children remains unclarified. Therefore, this study aimed to explore the maternal factors in pregnancy associated with twin offspring growth.
Methods
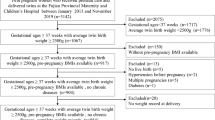
This study included 3142 live twin children born to 1571 mothers from the Beijing Birth Cohort Study conducted from 2016 to 2021 in Beijing, China. Original and corrected weight-for-age standard deviation scores of the twin offspring from birth to 36 months of age were calculated according to the World Health Organization Child Growth Standards. The corresponding weight trajectories were identified by the latent trajectory model. Maternal factors in pregnancy associated with the weight trajectories of the twin offspring were examined after adjustment for potential confounders.
Results
Five weight trajectories of the twin children were identified, with 4.9% (154/3142) exhibiting insufficient catch-up growth, 30.6% (961/3142), and 46.8% (1469/3142) showing adequate catch-up growth from different birth weights, and 15.0% (472/3142) and 2.7% (86/3142) showing various degrees of excessive catch-up growth. Maternal short stature [adjusted odds ratio (OR) = 0.691, 95% confidence interval (CI) = 0.563–0.848, P = 0.0004] and lower total gestational weight gain (GWG) (adjusted OR = 0.774, 95% CI = 0.616–0.972, P = 0.03) were associated with insufficient catch-up growth of the offspring. Maternal stature (adjusted OR = 1.331, 95% CI = 1.168–1.518, P < 0.001), higher pre-pregnancy body mass index (BMI) (adjusted OR = 1.230, 95% CI = 1.090–1.387, P < 0.001), total GWG (adjusted OR = 1.207, 95% CI = 1.068–1.364, P = 0.002), GWG rate (adjusted OR = 1.165, 95% CI = 1.027–1.321, P = 0.02), total cholesterol (TC) (adjusted OR = 1.150, 95% CI = 1.018–1.300, P = 0.03) and low-density lipoprotein-cholesterol (LDL-C) (adjusted OR = 1.177, 95% CI = 1.041–1.330) in early pregnancy were associated with excessive growth of the offspring. The pattern of weight trajectories was similar between monochorionic and dichorionic twins. Maternal height, pre-pregnancy BMI, GWG, TC and LDL-C in early pregnancy were positively associated with excess growth in dichorionic twins, yet a similar association was observed only between maternal height and postnatal growth in monochorionic twins.
Conclusion
This study identified the effect of maternal stature, weight status, and blood lipid profiles during pregnancy on postnatal weight trajectories of the twin offspring, thereby providing a basis for twin pregnancy management to improve the long-term health of the offspring.



Similar content being viewed by others
Data availability
The dataset is available upon reasonable request to the corresponding author.
References
Ananth CV, Chauhan SP. Epidemiology of twinning in developed countries. Semin Perinatol. 2012;36:156–61.
Gestations M. Twin, triplet, and higher-order multifetal pregnancies: ACOG Practice Bulletin, number 231. Obstet Gynecol. 2021;137:e145–62.
Li S, Gao J, Liu J, Hu J, Chen X, He J, et al. Perinatal outcomes and risk factors for preterm birth in twin pregnancies in a Chinese population: a multi-center retrospective study. Front Med (Lausanne). 2021;8:657862.
Zhu X, Huang C, Wu L, Deng Y, Lai X, Gu H, et al. Perinatal outcomes and related risk factors of single vs twin pregnancy complicated by gestational diabetes mellitus: meta-analysis. Comput Math Methods Med. 2022;2022:3557890.
Black RE, Cousens S, Johnson HL, Lawn JE, Rudan I, Bassani DG, et al. Global, regional, and national causes of child mortality in 2008: a systematic analysis. Lancet. 2010;375:1969–87.
Upadhyay RP, Naik G, Choudhary TS, Chowdhury R, Taneja S, Bhandari N, et al. Cognitive and motor outcomes in children born low birth weight: a systematic review and meta-analysis of studies from South Asia. BMC Pediatr. 2019;19:35.
Troutman JA, Sullivan MC, Carr GJ, Fisher J. Development of growth equations from longitudinal studies of body weight and height in the full term and preterm neonate: From birth to four years postnatal age. Birth Defects Res. 2018;110:916–32.
Isaacs EB, Morley R, Lucas A. Early diet and general cognitive outcome at adolescence in children born at or below 30 weeks gestation. J Pediatr. 2009;155:229–34.
Huang X, Liu J, Qi L, Adachi JD, Wu J, Li Z, et al. Birth weight and the risk of cardiovascular outcomes: a report from the large population-based UK Biobank Cohort Study. Front Cardiovasc Med. 2022;9:827491.
Martin A, Connelly A, Bland RM, Reilly JJ. Health impact of catch-up growth in low-birth weight infants: systematic review, evidence appraisal, and meta-analysis. Matern Child Nutr. 2017. https://doi.org/10.1111/mcn.12297.
Belfort MB, Gillman MW, Buka SL, Casey PH, McCormick MC. Preterm infant linear growth and adiposity gain: trade-offs for later weight status and intelligence quotient. J Pediatr. 2013;163:1564-9.e2.
Ong KK, Kennedy K, Castañeda-Gutiérrez E, Forsyth S, Godfrey KM, Koletzko B, et al. Postnatal growth in preterm infants and later health outcomes: a systematic review. Acta Paediatr. 2015;104:974–86.
Nobili V, Alisi A, Panera N, Agostoni C. Low birth weight and catch-up-growth associated with metabolic syndrome: a ten year systematic review. Pediatr Endocrinol Rev. 2008;6:241–7.
Ekelund U, Ong KK, Linné Y, Neovius M, Brage S, Dunger DB, et al. Association of weight gain in infancy and early childhood with metabolic risk in young adults. J Clin Endocrinol Metab. 2007;92:98–103.
Perng W, Rifas-Shiman SL, Kramer MS, Haugaard LK, Oken E, Gillman MW, et al. Early weight gain, linear growth, and mid-childhood blood pressure: a prospective study in project viva. Hypertension. 2016;67:301–8.
Han J, Jiang Y, Huang J, Zhang Y, Zhang Y, Zhang Y, et al. Postnatal growth of preterm infants during the first two years of life: catch-up growth accompanied by risk of overweight. Ital J Pediatr. 2021;47:66.
Huang L, Jiang S, Xu J, Lei X, Zhang J. Associations between prepregnancy body mass index, gestational weight gain and weight catch-up in small-for-gestational-age children. Matern Child Nutr. 2022;18:e13235.
Hoffman DJ, Powell TL, Barrett ES, Hardy DB. Developmental origins of metabolic diseases. Physiol Rev. 2021;101:739–95.
Institute of Medicine (US) and National Research Council (US) Committee to Reexamine IOM Pregnancy Weight Guidelines. Weight gain during pregnancy: reexamining the guidelines. Washington: National Academies Press; 2009.
International Association of Diabetes Pregnancy Study Groups Consensus Panel, Metzger BE, Gabbe SG, Persson B, Buchanan TA, Catalano PA, et al. International association of diabetes and pregnancy study groups recommendations on the diagnosis and classification of hyperglycemia in pregnancy. Diabetes Care. 2010;33:676–82.
Regitz-Zagrosek V, Roos-Hesselink JW, Bauersachs J, Blomstrom-Lundqvist C, Cifkova R, De Bonis M, et al. 2018 ESC Guidelines for the management of cardiovascular diseases during pregnancy. Eur Heart J. 2018;39:3165–241.
Capital Institute of Pediatrics; Coordinating Study Group of Nine Cities on the Physical Growth and Development of Children. Growth standard curves of birth weight, length and head circumference of Chinese newborns of different gestation. Chin J Pediatr. 2020;58:738–46.
WHO Multicentre Growth Reference Study Group. WHO Child Growth Standards: Length/Height-for-Age, Weight-for-Age, Weight-for-Length, Weight-for-Height and Body Mass Index-for-Age: Methods and Development. 2021. https://www.who.int/tools/child-growth-standards. Accessed 15 Oct 2021.
Elhakeem A, Hughes RA, Tilling K, Cousminer DL, Jackowski SA, Cole TJ, et al. Using linear and natural cubic splines, SITAR, and latent trajectory models to characterise nonlinear longitudinal growth trajectories in cohort studies. BMC Med Res Methodol. 2022;22:68.
Deng Y, Yang F, Mu D. First-year growth of 834 preterm infants in a Chinese population: a single-center study. BMC Pediatr. 2019;19:403.
Sinha B, Choudhary TS, Nitika N, Kumar M, Mazumder S, Taneja S, et al. Linear growth trajectories, catch-up growth, and its predictors among north indian small-for-gestational age low birthweight infants: a secondary data analysis. Front Nutr. 2022;9: 827589.
Clemente MG, Capobianco G, Galasso PM, Dessole F, Virdis G, Sanna MG, et al. Postnatal growth in a cohort of sardinian intrauterine growth-restricted infants. Biomed Res Int. 2017;2017:9382083.
Dulloo AG, Jacquet J, Seydoux J, Montani JP. The thrifty “catch-up fat” phenotype: its impact on insulin sensitivity during growth trajectories to obesity and metabolic syndrome. Int J Obes (Lond). 2006;30:S23-35.
Dulloo AG. Thrifty energy metabolism in catch-up growth trajectories to insulin and leptin resistance. Best Pract Res Clin Endocrinol Metab. 2008;22:155–71.
Summermatter S, Marcelino H, Arsenijevic D, Buchala A, Aprikian O, Assimacopoulos-Jeannet F, et al. Adipose tissue plasticity during catch-up fat driven by thrifty metabolism: relevance for muscle-adipose glucose redistribution during catch-up growth. Diabetes. 2009;58:2228–37.
Marcelino H, Veyrat-Durebex C, Summermatter S, Sarafian D, Miles-Chan J, Arsenijevic D, et al. A role for adipose tissue de novo lipogenesis in glucose homeostasis during catch-up growth: a Randle cycle favoring fat storage. Diabetes. 2013;62:362–72.
Desmond C, Casale D. Catch-up growth in stunted children: Definitions and predictors. PLoS ONE. 2017;12:e0189135.
Leger J, Limoni C, Collin D, Czernichow P. Prediction factors in the determination of final height in subjects born small for gestational age. Pediatr Res. 1998;43:808–12.
Woo Baidal JA, Locks LM, Cheng ER, Blake-Lamb TL, Perkins ME, Taveras EM. Risk factors for childhood obesity in the first 1,000 days: a systematic review. Am J Prev Med. 2016;50:761–79.
Heslehurst N, Vieira R, Akhter Z, Bailey H, Slack E, Ngongalah L, et al. The association between maternal body mass index and child obesity: A systematic review and meta-analysis. PLoS Med. 2019;16:e1002817.
Voerman E, Santos S, Patro Golab B, Amiano P, Ballester F, Barros H, et al. Maternal body mass index, gestational weight gain, and the risk of overweight and obesity across childhood: an individual participant data meta-analysis. PLoS Med. 2019;16:e1002744.
Mir SA, Chen L, Burugupalli S, Burla B, Ji S, Smith AAT, et al. Population-based plasma lipidomics reveals developmental changes in metabolism and signatures of obesity risk: a mother-offspring cohort study. BMC Med. 2022;20:242.
Godfrey KM, Reynolds RM, Prescott SL, Nyirenda M, Jaddoe VW, Eriksson JG, et al. Influence of maternal obesity on the long-term health of offspring. Lancet Diabetes Endocrinol. 2017;5:53–64.
Li Y, Pollock CA, Saad S. Aberrant DNA methylation mediates the transgenerational risk of metabolic and chronic disease due to maternal obesity and overnutrition. Genes (Basel). 2021;12:1653.
Tam WH, Ma RCW, Ozaki R, Li AM, Chan MHM, Yuen LY, et al. In utero exposure to maternal hyperglycemia increases childhood cardiometabolic risk in offspring. Diabetes Care. 2017;40:679–86.
Lowe WL Jr, Lowe LP, Kuang A, Catalano PM, Nodzenski M, Talbot O, et al. Maternal glucose levels during pregnancy and childhood adiposity in the Hyperglycemia and Adverse Pregnancy Outcome Follow-up Study. Diabetologia. 2019;62:598–610.
Tward C, Barrett J, Berger H, Kibel M, Pittini A, Halperin I, et al. Does gestational diabetes affect fetal growth and pregnancy outcome in twin pregnancies? Am J Obstet Gynecol. 2016;214:653.e1-8.
Dave ED, Bodnar LM, Vani K, Himes KP. Perinatal outcomes in twin pregnancies complicated by gestational diabetes. Am J Obstet Gynecol MFM. 2021;3:100396.
Ashwal E, Berger H, Hiersch L, Yoon EW, Zaltz A, Shah B, et al. Gestational diabetes and fetal growth in twin compared with singleton pregnancies. Am J Obstetr Gynecol. 2021;225:420.e1-e13.
Hur YM, Shin JS. Effects of chorion type on genetic and environmental influences on height, weight, and body mass index in South Korean young twins. Twin Res Hum Genet. 2008;11:63–9.
Ghi T, Prefumo F, Fichera A, Lanna M, Periti E, Persico N, et al. Development of customized fetal growth charts in twins. Am J Obstetr Gynecol. 2017;216:514.e1-e17.
Lipworth H, Melamed N, Berger H, Geary M, McDonald SD, Murray-Davis B, et al. Maternal weight gain and pregnancy outcomes in twin gestations. Am J Obstetr Gynecol. 2021;225:532.
Bodnar LM, Cartus AR, Parisi SM, Abrams B, Himes KP, Eckhardt CL, et al. Pregnancy weight gain in twin gestations and maternal and child health outcomes at 5 years. Int J Obes (Lond). 2021;45:1382–91.
Ardic C, Usta O, Omar E, Yıldız C, Memis E. Effects of infant feeding practices and maternal characteristics on early childhood obesity. Archivos argentinos de pediatria. 2019;117:26–33.
Acknowledgements
We thank the participants for their contribution to the study and the medical staff for collecting clinical information and blood samples.
Funding
This work was supported by the Scientific Research Common Program of Beijing Municipal Commission of Education (KM202110025007), the National Natural Science Foundation of China (82171671), the National Key Research and Development (2016YFC1000304), and Beijing Hospitals Authority’ Ascent Plan (DFL20191402).
Author information
Authors and Affiliations
Contributions
ZW: conceptualization, formal analysis, funding acquisition, methodology, writing–original draft; ZKS: data curation, investigation, writing–review and editing; YXX: methodology, validation, writing–review & editing; LJY: data curation, investigation; WJ: data curation, investigation; SW: data curation, investigation; LSN: data curation, investigation; WXX: data curation, investigation; GCM: data curation, investigation; LGH: funding acquisition, project administration, resources, writing–review and editing.
Corresponding author
Ethics declarations
Conflict of interest
No financial or non-financial benefits have been received or will be received from any party related directly or indirectly to the subject of this article.
Ethical approval
The study was approved by the ethics committee of Beijing Obstetrics and Gynecology Hospital, Capital Medical University (2018-ky-009-01), and written informed consent were obtained from all the participants or their legal guardian.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zheng, W., Zhang, KX., Yuan, XX. et al. Maternal weight, blood lipids, and the offspring weight trajectories during infancy and early childhood in twin pregnancies. World J Pediatr 19, 961–971 (2023). https://doi.org/10.1007/s12519-023-00703-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12519-023-00703-z