Abstract
Background
The impact of pediatric body mass index (BMI) trajectories on the risk of adolescent hypertension (HTN) determined by three separate visits remains unclear. This longitudinal study aims to identify potential pediatric sex-specific BMI trajectories and to assess their associations with HTN and HTN subtypes.
Methods
Based on the Health Promotion Program for Children and Adolescents (HPPCA) in Suzhou, China, a total of 24,426 participants who had initial normal blood pressure (BP) and had at least four BMI measurements during 2012–2020 were included. HTN was defined as simultaneously having three separate visits of elevated BP in 2020. Latent class growth models were used to explore sex-specific BMI trajectories, whose associations with HTN and HTN subtypes were further examined by logistic regression.
Results
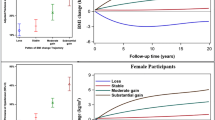
The incidence of HTN determined through three separate visits was 3.34%. Four trajectories were identified for both sexes: low BMI increasing, medium BMI increasing, high BMI increasing, and highest BMI increasing. Compared to the medium BMI increasing group, the odds ratio (95% confidential interval) for developing adolescent HTN of the low, high, and highest BMI increasing groups among boys were 0.54 (0.39, 0.75), 1.90 (1.44, 2.51), and 2.89 (1.90, 4.39), respectively; and the corresponding values for girls were 0.66 (0.48, 0.90), 2.30 (1.72, 3.09), and 4.71 (3.06, 7.26). Similar gradually elevated associations between different trajectories with isolated systolic hypertension, systolic and diastolic hypertension were observed.
Conclusion
Current results emphasized the adverse effects of stable high BMI on HTN and the benefits of maintaining normal weight throughout childhood.



Similar content being viewed by others
Data availability
Data are only available on an approved request to the corresponding author.
References
Yusuf S, Joseph P, Rangarajan S, Islam S, Mente A, Hystad P, et al. Modifiable risk factors, cardiovascular disease, and mortality in 155722 individuals from 21 high-income, middle-income, and low-income countries (PURE): a prospective cohort study. Lancet. 2020;395:795–808.
Roth GA, Abate D, Abate KH, Abay SM, Abbafati C, Abbasi N, et al. Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392:1736–88.
Redwine KM, Acosta AA, Poffenbarger T, Portman RJ, Samuels J. Development of hypertension in adolescents with pre-hypertension. J Pediatr. 2012;160:98–103.
Liang YJ, Xi B, Hu YH, Wang C, Liu JT, Yan YK, et al. Trends in blood pressure and hypertension among Chinese children and adolescents: China Health and Nutrition Surveys 1991–2004. Blood Press. 2011;20:45–53.
Liu K, Li C, Gong H, Guo Y, Hou B, Chen L, et al. Prevalence and risk factors for hypertension in adolescents aged 12 to 17 years: a school-based study in China. Hypertension. 2021;78:1577–85.
Dong J, Dong H, Yan Y, Cheng H, Zhao X, Mi J, et al. Prevalence of hypertension and hypertension phenotypes after three visits in Chinese urban children. J Hypertens. 2022;40:1270–7.
Kollias A, Dafni M, Poulidakis E, Ntineri A, Stergiou GS. Out-of-office blood pressure and target organ damage in children and adolescents: a systematic review and meta-analysis. J Hypertens. 2014;32:2315–31.
Yang L, Sun J, Zhao M, Liang Y, Bovet P, Xi B. Elevated blood pressure in childhood and hypertension risk in adulthood: a systematic review and meta-analysis. J Hypertens. 2020;38:2346–55.
Franks PW, Hanson RL, Knowler WC, Sievers ML, Bennett PH, Looker HC. Childhood obesity, other cardiovascular risk factors, and premature death. N Engl J Med. 2010;362:485–93.
Wang C, Yuan Y, Zheng M, Pan A, Wang M, Zhao M, et al. Association of age of onset of hypertension with cardiovascular diseases and mortality. J Am Coll Cardiol. 2020;75:2921–30.
Gorostidi M, Vinyoles E, Banegas JR, de la Sierra A. Prevalence of white-coat and masked hypertension in national and international registries. Hypertens Res. 2015;38:1–7.
Kollias A, Ntineri A, Stergiou GS. Is white-coat hypertension a harbinger of increased risk? Hypertens Res. 2014;37:791–5.
Zhang Q, Yang L, Zhang Y, Zhao M, Liang Y, Xi B. Hypertension prevalence based on three separate visits and its association with obesity among Chinese children and adolescents. Front Pediatr. 2019;7:307.
Sun J, Steffen LM, Ma C, Liang Y, Xi B. Definition of pediatric hypertension: are blood pressure measurements on three separate occasions necessary? Hypertens Res. 2017;40:496–503.
Flynn JT, Kaelber DC, Baker-Smith CM, Blowey D, Carroll AE, Daniels SR, et al. Clinical practice guideline for screening and management of high blood pressure in children and adolescents. Pediatrics. 2017;140:e20171904.
National Health Commission of the People’s Republic of China. Reference of screening for elevated blood pressure among children and adolescents aged 7–18 years (WS/T 610–2018). Beijing: Standards Press of China; 2018.
Teng H, Hu J, Ge W, Dai Q, Liu J, Xiao C, et al. Body mass index trajectories during 6–18 years old and the risk of hypertension in young adult: a longitudinal study in Chinese population. Int J Hypertens. 2021;2021:6646868.
Wang X, Dong B, Huang S, Ma Y, Zou Z, Ma J, et al. Body mass index trajectory and incident hypertension: results from a longitudinal cohort of Chinese children and adolescents, 2006–2016. Am J Public Health. 2020;110:1689–95.
Fan H, Zhang X. Body mass index trajectory across childhood and subsequent risk of elevated blood pressure. J Clin Hypertens (Greenwich). 2020;22:1902–7.
Parker ED, Sinaiko AR, Kharbanda EO, Margolis KL, Daley MF, Trower NK, et al. Change in weight status and development of hypertension. Pediatrics. 2016;137:e20151662.
Grossman DC, Bibbins-Domingo K, Curry SJ, Barry MJ, Davidson KW, Force USPST, et al. Screening for obesity in children and adolescents: US preventive services task force recommendation statement. JAMA. 2017;317:2417–26.
Rosner B, Cook NR, Daniels S, Falkner B. Childhood blood pressure trends and risk factors for high blood pressure: the NHANES experience 1988–2008. Hypertension. 2013;62:247–54.
Mattsson M, Maher GM, Boland F, Fitzgerald AP, Murray DM, Biesma R. Group-based trajectory modelling for BMI trajectories in childhood: a systematic review. Obes Rev. 2019;20:998–1015.
Rolland-Cachera MF, Deheeger M, Maillot M, Bellisle F. Early adiposity rebound: causes and consequences for obesity in children and adults. Int J Obes (Lond). 2006;30:S11–7.
Meigen C, Keller A, Gausche R, Kromeyer-Hauschild K, Bluher S, Kiess W, et al. Secular trends in body mass index in German children and adolescents: a cross-sectional data analysis via CrescNet between 1999 and 2006. Metabolism. 2008;57:934–9.
Hu J, Chu GP, Huang FF, Zhou YK, Teng CG, Yang HB, et al. Relation of body mass index (BMI) to the prevalence of hypertension in children: a 3 years’ school-based prospective study in Suzhou. China Int J Cardiol. 2016;222:270–4.
Hu J, Liu JY, Wang JX, Shen MZ, Ge WX, Shen H, et al. Unfavorable progression of obesity in children and adolescents due to COVID-19 pandemic: a school-based survey in China. Obesity. 2021;29:1907–15.
Ge W, Hu J, Xiao Y, Liang F, Yi L, Zhu R, et al. COVID-19 related childhood BMI increases in China: a health surveillance based ambispective cohort analysis. Am J Prev Med. 2022;000:1–9.
National Health Commission of the People’s Republic of China. Screening standard for malnutrition of school-age children and adolescents (WS/T 456–2014). Beijing: Standards Press of China; 2014.
National Health Commission of the People’s Republic of China. Screening for overweight and obesity among school-age children and adolescents (WS/T 586–2018). Beijing: Standards Press of China; 2018.
Jones BL, Nagin D, Roeder K. A SAS procedure based on mixture models for estimating developmental trajectories. Soc Method Res. 2001;29:374–93.
Andruff H, Carraro N, Thompson A, Gaudreau P. Latent class growth modeling a tutorial. Quant Meth Psych. 2009;5:11–24.
Wang J, Zhu Y, Jing J, Chen Y, Mai J, Wong SH, et al. Relationship of BMI to the incidence of hypertension: a 4 years’ cohort study among children in Guangzhou, 2007–2011. BMC Public Health. 2015;15:782.
Montazeri P, Fossati S, Clemente DBP, Cirugeda L, Elosua R, Fernandez-Barres S, et al. Early-childhood BMI trajectories in relation to preclinical cardiovascular measurements in adolescence. J Dev Orig Health Dis. 2022;13:322–9.
Ahanchi NS, Ramezankhani A, Munthali RJ, Asgari S, Azizi F, Hadaegh F. Body mass index trajectories from adolescent to young adult for incident high blood pressure and high plasma glucose. PLoS ONE. 2019;14:e0213828.
Munthali RJ, Kagura J, Lombard Z, Norris SA. Childhood adiposity trajectories are associated with late adolescent blood pressure: birth to twenty cohort. BMC Public Health. 2016;16:665.
Oluwagbemigun K, Buyken AE, Alexy U, Schmid M, Herder C, Nothlings U. Developmental trajectories of body mass index from childhood into late adolescence and subsequent late adolescence-young adulthood cardiometabolic risk markers. Cardiovasc Diabetol. 2019;18:9.
Cheung EL, Bell CS, Samuel JP, Poffenbarger T, Redwine KM, Samuels JA. Race and obesity in adolescent hypertension. Pediatrics. 2017;139:e20161433.
Wildman RP, Mackey RH, Bostom A, Thompson T, Sutton-Tyrrell K. Measures of obesity are associated with vascular stiffness in young and older adults. Hypertension. 2003;42:468–73.
Palatini P, Rosei EA, Avolio A, Bilo G, Casiglia E, Ghiadoni L, et al. Isolated systolic hypertension in the young: a position paper endorsed by the European Society of Hypertension. J Hypertens. 2018;36:1222–36.
Acknowledgements
We sincerely appreciate all the children, parents, and workers who were involved in the study.
Funding
This work was supported by Gusu Health Talents Program Training Project in Suzhou, China (GSWS2020100), the National Natural Science Foundation of China (81602911, 82204070, and 82273635), and Priority Academic Program Development of Jiangsu Higher Education Institutions (PAPD).
Author information
Authors and Affiliations
Contributions
GWX: writing–original draft. HD, DZY, HB, LHL, SH, and YHB: data curation, formal analyses. YLP, YZQ, WXN, XY, and LF: writing–review and editing. YJY, HJ: conceptualization. GWX and HD contributed equally to this study. All authors had final approval of the submitted and published versions.
Corresponding authors
Ethics declarations
Conflict of interest
No financial or nonfinancial benefits have been received or will be received from any party related directly or indirectly to the subject of this article.
Ethical approval
All work was carried out with the consent of participants and their parents. This study was approved by the Ethics Committee of Suzhou Center for Disease Prevention and Control (No.SZJK2020-XW001).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ge, WX., Han, D., Ding, ZY. et al. Pediatric body mass index trajectories and the risk of hypertension among adolescents in China: a retrospective cohort study. World J Pediatr 19, 76–86 (2023). https://doi.org/10.1007/s12519-022-00626-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12519-022-00626-1