Abstract
Background
Asthma control in African Americans (AA) is considered more difficult to achieve than in Caucasian Americans (CA). The aim of this study was to compare asthma control over time among AA and CA children whose asthma is managed per NAEPP (EPR-3) guidelines.
Methods
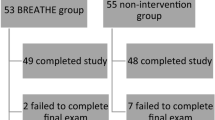
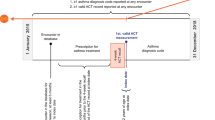
This was a one-year prospective study of children referred by their primary care physicians for better asthma care in a specialty asthma clinic. All children received asthma care per NAEPP guidelines. Results were compared between CA and AA children at baseline and then at three-month intervals for one year.
Results
Of the 345 children, ages 2–17 years (mean = 6.2 ± 4), 220 (63.8%) were CA and 125 (36.2%) were AA. There were no significant differences in demographics other than greater pet ownership in CA families. At baseline, AA children had significantly more visits to the Emergency Department for acute asthma symptoms (mean = 2.3 \(\pm 3)\) compared to CA (1.4 ± 2.3, P = 0.003). There were no other significant differences in acute care utilization, asthma symptoms (mean days/month), or mean asthma control test (ACT) scores at baseline. Within 3–6 months, in both groups, mean ACT scores, asthma symptoms and acute care utilization significantly improved (P < 0.05 for all) and change over time in both groups was comparable except for a significantly greater decrease in ED visits in AA children compared to CA children (P = 002).
Conclusion
Overall, improvement in asthma control during longitudinal assessment was similar between AA and CA children because of consistent use of NAEPP asthma care guidelines.
Similar content being viewed by others
Data availability and material
Data set will be available if asked.
References
Centers for Disease Control and Prevention (CDC). Asthma. Data, Statistics, and Surveillance. CDC’s National Asthma Control Program. https://www.cdc.gov/asthma/nacp.htm (2021). Accessed 21 Jan 2021.
Ford JG, Meyer IH, Sternfels P, Findley SE, McLean DE, Fagan JK, Richardson L. Patterns and predictors of asthma-related emergency department use in Harlem. Chest. 2001;120:1129–35.
Akinbami LJ, Moorman JE, Simon AE, Schoendorf KC. Trends in racial disparities for asthma outcomes among children 0 to 17 years, 2001-2010. J Allergy Clin Immunol. 2014;134:547–553.e5.
Centers for Disease Control and Prevention National Center for Health Statistics. National Health Interview Survey, 2015. Table 4–1: Current asthma prevalence percents by age. https://www.cdc.gov/asthma/nhis/2015/table4-1.htm. Accessed 28 Feb 2017.
Centers for Disease Control and Prevention National Center for Health Statistics. Asthma as the Underlying Cause of Death. https://www.cdc.gov/asthma/asthma_stats/asthma_underlying_death.html. Accessed 10 Apr 2018.
Majellano EC, Clark VL, Winter NA, Gibson PG, McDonald VM. Approaches to the assessment of severe asthma: barriers and strategies. J Asthma Allergy. 2019;23:235–51.
Baiardini I, Braido F, Baiardini F, Bonini M, Compalati E, Canonica GW. Why do doctors and patients not follow guidelines? Curr Opin Allergy Clin Immunol. 2009;9:228–33.
Weinberger M. Seventeen years of asthma guidelines: why hasn’t the outcome improved for children? J Pediatr. 2009;154:786–8.
Expert Panel Report 3 (EPR-3). Guidelines for the diagnosis and management of asthma-summary report 2007. J Allergy Clin Immunol. 2007;2:S94–138.
Sheikh SI, Ryan-Wenger NA, Pitts J, Nemastil CJ, Palacios S. Impact of asthma severity on long-term asthma control. J Asthma. 2020;58:725–34.
Asthma Control Test (ACT) and Childhood Asthma Control Test (c-ACT) http://www.asthma.com/additional-resources/childhood-asthma-control-test.html. Copyright 2002, by QualityMetric Incorporated. Last updated 2019. Accessed 20 Jan 2020.
Centers for Disease Control and Prevention; National Asthma Control Program (NACP). Asthma’s Impact on the Nation. Data, Statistics, and Surveillance. Mortality data by State and Year. 2019. https://www.cdc.gov/asthma/data-visualizations/mortality-data.htm#anchor_1569600183140. Accessed 23 Sep 2019.
Heron M, Hoyert DL, Murphy SL, Xu J, Kochanek KD, Tejada-Vera B. Deaths: Final Data for 2006. National Vital Statistics Reports; 57(14). Hyattsville, MD: National Center for Health Statistics. 2009. https://www.cdc.gov/nchs/data/nvsr/nvsr57/nvsr57_14.pdf. Accessed 19 May 2020.
Akinbami LJ, Moorman JE, Garbe PL, Sondik EJ. Status of childhood asthma in the United States, 1980–2007. Pediatrics. 2009;123:S131–45.
Akinbami LJ, Schoendorf KC. Trends in childhood asthma: prevalence, health care utilization, and mortality. Pediatrics. 2002;110:315–22.
Asthma and Allergy Foundation of America, National Pharmaceutical Council. Ethnic Disparities in the Burden and Treatment of Asthma. http://www.aafa.org/media/Ethnic-Disparities-Burden-Treatment-Asthma-Report.pdf. Accessed 14 Nov 2020.
Davidson AE, Klein DE, Settipane GA, Alario AJ. Access to care among children visiting the emergency room with acute exacerbations of asthma. Ann Allergy. 1994;72:469–73.
Lozano P, Connell FA, Koepsell TD. Use of health services by african-american children with asthma on medicaid. JAMA. 1995;274:469–73.
Shields AE, Comstock C, Weiss KB. Variations in asthma care by race/ethnicity among children enrolled in a state Medicaid program. Pediatrics. 2004;113:496–504.
Diaz T, Sturm T, Matte T, Bindra M, Lawler K, Findley S, et al. Medication use among children with asthma in East Harlem. Pediatrics. 2000;105:1188–93.
Warman KL, Silver EJ, Stein RE. Asthma symptoms, morbidity, and anti-inflammatory use in inner-city children. Pediatrics. 2001;108:277–82.
Ortega AN, Gergen PJ, Paltiel AD, Bauchner H, Belanger KD, Leaderer BP. Impact of site of care, race, and Hispanic ethnicity on medication use for childhood asthma. Pediatrics. 2002;109:E1.
Finkelstein JA, Brown RW, Schneider LC, Weiss ST, Quintana JM, Goldmann DA, et al. Quality of care for preschool children with asthma: the role of social factors and practice setting. Pediatrics. 1995;95:389–94.
Halterman JS, Aligne CA, Auinger P, McBride JT, Szilagyi PG. Inadequate therapy for asthma among children in the United States. Pediatrics. 2000;105:272–6.
Lieu TA, Lozano P, Finkelstein JA, Chi FW, Jensvold NG, Capra AM, et al. Racial/ ethnic variation in asthma status and management practices among children in managed medicaid. Pediatrics. 2002;109:857–65.
Finkelstein JA, Lozano P, Farber HJ, Miroshnik I, Lieu TA. Underuse of controller medications among medicaid-insured children with asthma. Arch Pediatr Adolesc Med. 2002;156:562–7.
Cloutier MM, Salo PM, Akinbami LJ, Cohn RD, Wilkerson JC, Diette GB, et al. Clinician agreement, self-efficacy, and adherence with the guidelines for the diagnosis and management of asthma. J Allergy Clin Immunol Pract. 2018;6:886–94.e4.
Cloutier MM, Hall CB, Wakefield DB, Bailit H. Use of asthma guidelines by primary care providers to reduce hospitalizations and emergency department visits in poor, minority, urban children. J Pediatr. 2005;146:591–7.
Szefler SJ. Advances in pediatric asthma in 2014: moving toward a population health perspective. J Allergy Clin Immunol. 2015;135:644–52.
Cloutier MM, Wakefield DB, Carlisle PS, Bailit HL, Hall CB. The effect of easy breathing on asthma management and knowledge. Arch Pediatr Adolesc Med. 2002;156:1045–51.
Cloutier MM, Wakefield DB, Sangeloty-Higgins P, Delaronde S, Hall CB. Asthma guideline use by pediatricians in private practices and asthma morbidity. Pediatrics. 2006;118:1880–7.
Funding
None.
Author information
Authors and Affiliations
Contributions
Conceptualization: SIS. Data curation and formal analysis: NAR-W. Methodology: SIS, JP, RB, LU. Supervision: SIS, RB, GP, LU. Writing—original draft: SIS, NAR-W, JP, RB, GP, LU. Writing—review and editing: SIS, NAR-W, JP, RB, GP, LU. We have seen and approved the final version submitted for publication and take full responsibility for the manuscript.
Corresponding author
Ethics declarations
Ethical approval
This study was approved by the Institutional Review Board of Nationwide Children’s Hospital Research Center (IRB11-00,174). Informed consent and child assent was waived.
Conflict of interest
No financial or non-financial benefits have been received or will be received from any party related directly or indirectly to the subject of this article. None of the authors serves as a current or past editorial board member of WJP.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Sheikh, S.I., Ryan-Wenger, N.A., Pitts, J. et al. Impact of guideline adherence and race on asthma control in children. World J Pediatr 17, 500–507 (2021). https://doi.org/10.1007/s12519-021-00458-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12519-021-00458-5