Abstract
Background
Dent disease is a rare tubulopathy characterized by manifestations of proximal tubular dysfunction, which occurs almost exclusively in males. It mainly presents symptoms in early childhood and may progress to end-stage renal failure between the 3rd and 5th decades of human life. According to its various genetic basis and to clinical signs and symptoms, researchers define two forms of Dent disease (Dent diseases 1 and 2) and suggest that these forms are produced by mutations in the CLCN5 and OCRL genes, respectively. Dent diseases 1 and 2 account for 60% and 15% of all Dent disease cases, and their genetic cause is generally understood. However, the genetic cause of the remaining 25% of Dent disease cases remains unidentified.
Data sources
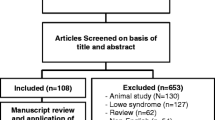
All relevant peer-reviewed original articles published thus far have been screened out from PubMed and have been referenced.
Results
Genetic testing has been used greatly to identify mutation types of CLCN5 and OCRL gene, and next-generation sequencing also has been used to identify an increasing number of unknown genotypes. Gene therapy may bring new hope to the treatment of Dent disease. The abuse of hormones and immunosuppressive agents for the treatment of Dent disease should be avoided to prevent unnecessary harm to children.
Conclusions
The current research progress in classification, genetic heterogeneity, diagnosis, and treatment of Dent disease reviewed in this paper enables doctors and researchers to better understand Dent disease and provides a basis for improved prevention and treatment.
Similar content being viewed by others
References
Ehlayel AM, Copelovitch L. Update on Dent disease. Pediatr Clin N Am. 2019;66:169–78.
Dent CE, Friedman M. Hypercalciuric rickets associated with renal tubular damage. Arch Dis Child. 1964;39:240–9.
Wrong OM, Norden AG, Feest TG. Dent's disease; a familial proximal renal tubular syndrome with low-molecular-weight proteinuria, hypercalciuria, nephrocalcinosis, metabolic bone disease, progressive renal failure and a marked male predominance. QJM. 1994;87:473–93.
Bignon Y, Alekvo A, Frachon N, Lahuna O, Jean-Baptiste Doh-Egueli C, Deschênes G, et al. A novel CLCN5 pathogenic mutation supports Dent disease with normal endosomal acidification. Hum Mutat. 2018;39:1139–49.
Devuyst O, Thakker RV. Dent's disease. Orphanet J Rare Dis. 2010;5:28.
Blanchard A, Curis E, Guyon-Roger T, Kahila D, Treard C, Baudouin V, et al. Observations of a large Dent disease cohort. Kidney Int. 2016;90:430–9.
Claverie-Martin F, Ramos-Trujillo E, Garcia-Nieto V. Dent's disease: clinical features and molecular basis. Pediatr Nephrol. 2011;26:693–704.
Sekine T, Komoda F, Miura K, Takita J, Shimadzu M, Matsuyama T, et al. Japanese Dent disease has a wider clinical spectrum than Dent disease in Europe/USA: genetic and clinical studies of 86 unrelated patients with low-molecular-weight proteinuria. Nephrol Dial Transpl. 2014;29:376–84.
Solanki AK, Arif E, Morinelli T, Wilson RC, Hardiman G, Deng P, et al. A novel CLCN5 mutation associated with focal segmental glomerulosclerosis and podocyte injury. Kidney Int Rep. 2018;3:1443–53.
Fervenza FC. A patient with nephrotic-range proteinuria and focal global glomerulosclerosis. Clin J Am Soc Nephrol. 2013;8:1979–87.
Beara-Lasic L, Cogal A, Mara K, Enders F, Mehta RA, Haskic Z, et al. Prevalence of low molecular weight proteinuria and Dent disease 1 CLCN5 mutations in proteinuric cohorts. Pediatr Nephrol. 2019. https://doi.org/10.1007/s00467-019-04210-0.
Mansour-Hendili L, Blanchard A, Le Pottier N, Roncelin I, Lourdel S, Treard C, et al. Mutation update of the CLCN5 gene responsible for Dent disease 1. Hum Mutat. 2015;36:743–52.
Ye Q, Shen Q, Rao J, Zhang A, Zheng B, Liu X, et al. Multicenter study of the clinical features and mutation gene spectrum of Chinese children with Dent disease. Clin Genet. 2020;97:407–17.
Zhang H, Wang C, Yue H, Hu WW, Gu JM, He JM, et al. Identification of a novel mutation in the CLCN5 gene in a Chinese family with Dent-1 disease. Nephrology (Carlton). 2014;19:80–3.
Wang X, Anglani F, Beara-Lasic L, Mehta AJ, Vaughan LE, Herrera HL. Glomerular pathology in Dent disease and its association with kidney function. Clin J Am Soc Nephrol. 2016;11:2168–76.
Zaniew M, Bökenkamp A, Kołbuc M, La Scola C, Baronio F, Niemirska A, et al. Long-term renal outcome in children with OCRL mutations: retrospective analysis of a large international cohort. Nephrol Dial Transpl. 2018;33:85–94.
Bökenkamp A, Böckenhauer D, Cheong HI, Hoppe B, Tasic V, Unwin R, et al. Dent-2 disease: a mild variant of Lowe syndrome. J Pediatr. 2009;155:94–9.
Marzuillo P, Caiazzo R, Coppola C, Camponesco O, Miraglia Del Giudice E, Argenziano G, et al. Polyclonal gammopathy in an adolescent affected by Dent disease 2 and hidradenitis suppurativa. Int J Dermatol. 2020. https://doi.org/10.1111/ijd.14789.
Marzuillo P, Piccolo V, Mascolo M, Apicella A, Argenziano G, Della Vecchia N, et al. Patients affected by dent disease 2 could be predisposed to hidradenitis suppurativa. J Eur Acad Dermatol Venereol. 2018;32:e309–11.
Picollo A, Pusch M. Chloride/proton antiporter activity of mammalian CLC proteins ClC-4 and ClC-5. Nature. 2005;436:420–3.
Dutzler R, Campbell EB, Cadene M, Chait BT, Mackinnon R. X-ray structure of a ClC chloride channel at 3.0 Å reveals the molecular basis of anion selectivity. Nature. 2002;415:287–94.
Novarino G, Weinert S, Rickheit G, Jentsch TJ. Endosomal chloride-proton exchange rather than chloride conductance is crucial for renal endocytosis. Science. 2010;328:1398–401.
Günther W, Lüchow A, Cluzeaud F, Vandewalle A, Jentsch TJ. ClC-5, the chloride channel mutated in Dent's disease, colocalizes with the proton pump in endocytotically active kidney cells. Proc Natl Acad Sci USA. 1998;95:8075–88.
Claverie-Martín F, Ramos-Trujillo E, García-Nieto V. Dent's disease: clinical features and molecular basis. Pediatr Nephrol. 2011;26:693–704.
Günther W, Piwon N, Jentsch TJ. The ClC-5 chloride channel knock-out mouse—an animal model for Dent's disease. Pflugers Arch. 2003;445:456–62.
Wellhauser L, D'Antonio C, Bear CE. ClC transporters: discoveries and challenges in defining the mechanisms underlying function and regulation of ClC-5. Pflugers Arch. 2010;460:543–57.
Matsumoto A, Matsui I, Mori T, Sakaguchi Y, Mizui M, Ueda Y, et al. A case of severe osteomalacia with Dent disease caused by a novel intronic mutation of the CLCN5 gene. Internal Med. 2018;57:3603–10.
Tosetto E, Ghiggeri GM, Emma F, Barbano G, Carrea A, Vezzoli G, et al. Phenotypic and genetic heterogeneity in Dent's disease—the results of an Italian collaborative study. Nephrol Dial Transpl. 2006;21:2452–63.
Lourdel S, Grand T, Burgos J, González W, Sepúlveda FV, Teulon J. ClC-5 mutations associated with Dent's disease: a major role of the dimer interface. Pflugers Arch. 2012;463:247–56.
Zhang Y, Fang XY, Xu H, Shen Q. Genetic analysis of Dent's disease and functional research of CLCN5 mutations. DNA Cell Biol. 2017;36:1151–8.
Grand T, L'Hoste S, Mordasini D, Defontaine N, Keck M, Pennaforte T, et al. Heterogeneity in the processing of CLCN5 mutants related to Dent disease. Hum Mutat. 2011;32:476–83.
Attree O, Olivos IM, Okabe I, Bailey LC, Nelson DL, Lewis RA, et al. The Lowe's oculocerebrorenal syndrome gene encodes a protein highly homologous to inositol polyphosphate-5-phosphatase. Nature. 1992;358:239–42.
Hoopes RR Jr, Shrimpton AE, Knohl SJ, Hueber P, Hoppe B, Matyus J, et al. Dent disease with mutations in OCRL1. Am J Hum Genet. 2005;76:260–7.
De Matteis MA, Staiano L, Emma F, Devuyst O. The 5-phosphatase OCRL in Lowe syndrome and Dent disease 2. Nat Rev Nephrol. 2017;13:455–70.
Staiano L, De Leo MG, Persico M, De Matteis MA. Mendelian disorders of PI metabolizing enzymes. Biochim Biophys Acta. 2015;1851:867–81.
Song E, Luo N, Alvarado JA, Lim M, Walnuss C, Neely D, et al. Ocular pathology of oculocerebrorenal syndrome of Lowe: novel mutations and genotype–phenotype analysis. Sci Rep. 2017;7:1442.
Stenson PD, Ball EV, Mort M, Phillips AD, Shiel JA, Thomas NS, et al. Human Gene Mutation Database (HGMD): 2003 update. Hum Mutat. 2003;21:577–81.
Erb BC, Velázquez H, Gisser M, Shugrue CA, Reilly RF. cDNA cloning and localization of OCRL-1 in rabbit kidney. Am J Physiol. 1997;273:F790–5.
Oltrabella F, Pietka G, Ramirez IB, Mironov A, Starborg T, Drummond IA, et al. The Lowe syndrome protein OCRL1 is required for endocytosis in the zebrafish pronephric tubule. PLoS Genet. 2015;11:e1005058.
Mehta ZB, Pietka G, Lowe M. The cellular and physiological functions of the Lowe syndrome protein OCRL1. Traffic. 2014;15:471–87.
Lowe CU, Terrey M, Maclachlan EA. Organic-aciduria, decreased renal ammonia production, hydrophthalmos, and mental retardation; a clinical entity. AMA Am J Dis Child. 1952;83:164–84.
Festa BP, Berquez M, Gassama A, Amrein I, Ismail HM, Samardzija M, et al. OCRL deficiency impairs endolysosomal function in a humanized mouse model for Lowe syndrome and Dent disease. Hum Mol Genet. 2019;28:1931–46.
Addis M, Meloni C, Tosetto E, Ceol M, Cristofaro R, Melis MA, et al. An atypical Dent's disease phenotype caused by co-inheritance of mutations at CLCN5 and OCRL genes. Eur J Hum Genet. 2013;21:687–90.
Li F, Yue Z, Xu T, Chen M, Zhong L, Liu T, et al. Dent disease in Chinese children and findings from heterozygous mothers: phenotypic heterogeneity, fetal growth, and 10 novel mutations. J Pediatr. 2016;174:204–10.e1.
Frishberg Y, Dinour D, Belostotsky R, Becker-Cohen R, Rinat C, Feinstein S, et al. Dent's disease manifesting as focal glomerulosclerosis: is it the tip of the iceberg? Pediatr Nephrol. 2009;24:2369–73.
Bogdanović R, Draaken M, Toromanović A, Dordević M, Stajić N, Ludwig M. A novel CLCN5 mutation in a boy with Bartter-like syndrome and partial growth hormone deficiency. Pediatr Nephrol. 2010;25:2363–8.
Zhang H, Wang F, Xiao H, Yao Y. The ratio of urinary α1-microglobulin to microalbumin can be used as a diagnostic criterion for tubuloproteinuria. Intractable Rare Dis Res. 2018;7:46–50.
He G, Zhang H, Wang F, Liu X, Xiao H, Yao Y. Diagnosis and treatment of Dent disease in 10 Chinese boys. Intractable Rare Dis Res. 2017;6:41–5.
Levinson SS. Urine protein electrophoresis and immunofixation electrophoresis supplement one another in characterizing proteinuria. Ann Clin Lab Sci. 2000;30:79–84.
Raja KA, Schurman S, D'Mello RG, Blowey D, Goodyer P, Van Why C, et al. Responsiveness of hypercalciuria to thiazide in Dent's disease. J Am Soc Nephrol. 2002;13:2938–44.
Cebotaru V, Kaul S, Devuyst O, Cai H, Racusen L, Guggino WB, et al. High citrate diet delays progression of renal insufficiency in the ClC-5 knockout mouse model of Dent's disease. Kidney Int. 2005;68:642–52.
Vaisbich MH, Henriques Ldos S, Igarashi T, Sekine T, Seki G, Koch VH. The long-term use of enalapril and hydrochlorothiazide in two novel mutations patients with Dent's disease type 1. J Bras Nefrol. 2012;34:78–81.
Vrljicak K, Batinić D, Milosević D, Nizić-Stancin L, Ludwig M. A boy with Dent-2 disease. Coll Antropol. 2011;35:925–8.
Gabriel SS, Belge H, Gassama A, Debaix H, Luciani A, Fehr T, et al. Bone marrow transplantation improves proximal tubule dysfunction in a mouse model of Dent disease. Kidney Int. 2017;91:842–55.
Sheffer-Babila S, Chandra M, Speiser PW. Growth hormone improves growth rate and preserves renal function in Dent disease. J Pediatr Endocrinol Metab. 2008;21:279–86.
Funding
The study was supported by National Natural Foundation of China (81470939 & 81770710), Natural Science Foundation of Zhejiang Province (LH14H050002, LY15H050001, LQ18H050001), and Ai You Foundation.
Author information
Authors and Affiliations
Contributions
JYY wrote the initial draft. HLM revised the manuscript. QXF and MJH reviewed and revised the manuscript. All authors approved the final version.
Corresponding author
Ethics declarations
Ethical approval
Not needed.
Conflict of interest
All authors disclosed no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Jin, YY., Huang, LM., Quan, XF. et al. Dent disease: classification, heterogeneity and diagnosis. World J Pediatr 17, 52–57 (2021). https://doi.org/10.1007/s12519-020-00357-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12519-020-00357-1