Abstract
Background
Women who had delivered a macrosomic newborn will have a higher risk to deliver another macrosomia. We aimed to examine the recurrence risk of macrosomia in the subsequent pregnancy and the implications in long-term child health.
Methods
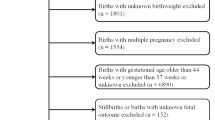
Data from the Collaborative Perinatal Project, a longitudinal birth cohort with 54,371 singleton births, were used. 401 recurrent macrosomic infants (macro-macro) and 1327 normal weight babies with a macrosomia in the last pregnancy (macro-normal) were selected to explore risk factors for recurrent macrosomia. Furthermore, 768 newly onset macrosomia with normal birthweight infant in previous pregnancies (normal-macro) were identified to examine long-term health effects of recurrent macrosomia.
Results
The recurrent rate of macrosomia was 23.2% [95% confidence interval (CI) 21.2%, 25.2%]. White race, higher pre-pregnant body mass index (BMI), more gestational weight gain, male infant and more prior macrosomic infants were significant risk factors for recurrent macrosomia. At 4 years of age, recurrent macrosomic infants had a higher BMI (16.7 vs. 16.1 kg/m2, adjusted β: 0.36, 95% CI: 0.12, 0.60) and a higher risk of overweight and obesity (adjusted OR: 1.56, 95% CI: 1.10, 2.23) than infants with normal birthweight after a previous macrosomic sibling. There was no significant difference between recurrent macrosomia and newly onset macrosomia in child outcomes after adjustment for covariates.
Conclusions
Fetal macrosomia has a high recurrence rate in the following pregnancy. Higher maternal pre-pregnant BMI and gestational weight gain are still important risk factors for recurrence of macrosomia, which in turn increases the risk for childhood obesity.

Similar content being viewed by others
References
Bonellie SR, Raab GM. Why are babies getting heavier? Comparison of Scottish births from 1980 to 1992. BMJ. 1997;315:1205.
Mocanu EV, Greene RA, Byrne BM, Turner MJ. Obstetric and neonatal outcome of babies weighing more than 4.5 kg: an analysis by parity. Eur J Obstet Gynecol Reprod Biol. 2000;92:229–33.
Sultan AH, Kamm MA, Hudson CN, Bartram CI. Third degree obstetric anal sphincter tears: risk factors and outcome of primary repair. BMJ. 1994;308:887–91.
Nesbitt TS, Gilbert WM, Herrchen B. Shoulder dystocia and associated risk factors with macrosomic infants born in California. Am J Obstet Gynecol. 1998;179:476–80.
Rich-Edwards JW, Colditz GA, Stampfer MJ, Willett WC, Gillman MW, Hennekens CH, et al. Birthweight and the risk for type 2 diabetes mellitus in adult women. Ann Intern Med. 1999;130:278–84.
Gale CR, Martyn CN, Kellingray S, Eastell R, Cooper C. Intrauterine programming of adult body composition. J Clin Endocrinol Metab. 2001;86:267–72.
Jolly MC, Sebire NJ, Harris JP, Regan L, Robinson S. Risk factors for macrosomia and its clinical consequences: a study of 350,311 pregnancies. Eur J Obstet Gynecol Reprod Biol. 2003;111:9–14.
Boulet SL, Alexander GR, Salihu HM, Pass M. Macrosomic births in the united states: determinants, outcomes, and proposed grades of risk. Am J Obstet Gynecol. 2003;188:1372–8.
Kristensen P, Susser E, Irgens LM, Mehlum IS, Corbett K, Bjerkedal T. The association of high birth weight with intelligence in young adulthood: a cohort study of male siblings. Am J Epidemiol. 2014;180:876–84.
Eide MG, Oyen N, Skjærven R, Bjerkedal T. Associations of birth size, gestational age, and adult size with intellectual performance: evidence from a cohort of Norwegian men. Pediatr Res. 2007;62:636–42.
Zhao D, Huang L, Luo Z, Zhang J, Yu X, Zhang Y. Childhood health outcomes in term, large-for-gestational-age babies with different postnatal growth patterns. Am J Epidemiol. 2018;187:507–14.
Hemachandra AH, Howards PP, Furth SL, Klebanoff MA. Birth weight, postnatal growth, and risk for high blood pressure at 7 years of age: results from the Collaborative Perinatal Project. Pediatrics. 2007;119:e1264–70.
Kwok MK, Au Yeung SL, Leung GM, Schooling CM. Birth weight, infant growth, and adolescent blood pressure using twin status as an instrumental variable in a Chinese birth cohort: “Children of 1997”. Ann Epidemiol. 2014;24:509–15.
Seidman DS, Laor A, Gale R, Stevenson DK, Mashiach S, Danon YL. Birth weight and intellectual performance in late adolescence. Obstet Gynecol. 1992;79:543–6.
Richards M, Hardy R, Kuh D, Wadsworth ME. Birth weight and cognitive function in the British 1946 birth cohort: longitudinal population based study. BMJ. 2001;322:199–203.
Hardy JB. The collaborative perinatal project: lessons and legacy. Ann Epidemiol. 2003;13:303–11.
Klebanoff MA. The Collaborative Perinatal Project: a 50-year retrospective. Paediatr Perinat Epidemiol. 2009;23:2–8.
Terry MB, Flom J, Tehranifar P, Susser E. The role of birth cohorts in studies of adult health: the New York women’s birth cohort. Paediatr Perinat Epidemiol. 2009;23:431–45.
Institute of Medicine (US) and National Research Council (US) Committee to Reexamine IOM Pregnancy Weight Guidelines, Rasmussen KM, Yaktine AL. Weight gain during pregnancy: reexamining the guidelines. Washington, DC: The National Academies Press; 2009.
Cole TJ, Bellizzi MC, Flegal KM, Dietz WH. Establishing a standard definition for child overweight and obesity worldwide: international survey. BMJ. 2000;320:1240.
Hiersch L, Shinar S, Melamed N, Aviram A, Hadar E, Yogev Y, et al. Birthweight and large for gestational age trends in non-diabetic women with three consecutive term deliveries. Arch Gynecol Obstet. 2018;298:725–30.
Alberico S, Montico M, Barresi V, Monasta L, Businelli C, Soini V, et al. The role of gestational diabetes, pre-pregnancy body mass index and gestational weight gain on the risk of newborn macrosomia: results from a prospective multicentre study. BMC Pregnancy Childbirth. 2014;14(1):23.
Sparano S, Ahrens W, De Henauw S, Marild S, Molnar D, Moreno LA, et al. Being macrosomic at birth is an independent predictor of overweight in children: results from the IDEFICS study. Matern Child Health J. 2013;17:1373–81.
Matte TD, Bresnahan M, Begg MD, Susser E. Influence of variation in birth weight within normal range and within sibships on IQ at age 7 years: cohort study. BMJ. 2001;323:310–4.
Boyd ME, Usher RH, Mclean FH. Fetal macrosomia: prediction, risks, proposed management. Obstet Gynecol. 1983;61:715–22.
Myrianthopoulos NC, French KS. An application of the US Bureau of the Census socioeconomic index to a large, diversified patient population. Soc Sci Med. 1968;2:283–99.
Lucas A, Fewtrell MS, Cole TJ. Fetal origins of adult disease—the hypothesis revisited. BMJ. 1999;319:245.
Arah OA. The role of causal reasoning in understanding Simpson’s paradox, Lord’s paradox, and the suppression effect: covariate selection in the analysis of observational studies. Emerg Themes Epidemiol. 2008;5:5.
Zhou L, He G, Zhang J, Xie R, Walker M, Wen SW. Risk factors of obesity in preschool children in an urban area in China. Eur J Pediatr. 2011;170:1401–6.
Mehta SH, Kruger M, Sokol RJ. Being too large for gestational age precedes childhood obesity in African Americans. Am J Obstet Gynecol. 2011;204(265):e1–5.
Breslau N. Psychiatric sequelae of low birth weight. Epidemiol Rev. 1995;17:96–106.
Record RG, McKEOWN T, Edwards JH. The relation of measured intelligence to birth weight and duration of gestation. Ann Hum Genet. 1969;33:71–9.
Huxley R, Neil A, Collins R. Unravelling the fetal origins hypothesis: is there really an inverse association between birthweight and subsequent blood pressure? Lancet. 2002;360:659–65.
Lawlor DA, Leon DA, Rasmussen F. Growth trajectory matters: interpreting the associations among birth weight, concurrent body size, and systolic blood pressure in a cohort study of 378,707 Swedish men. Am J Epidemiol. 2007;165:1405–12.
Evagelidou EN, Kiortsis DN, Bairaktari ET, Giapros VI, Cholevas VK, Tzallas CS, et al. Lipid profile, glucose homeostasis, blood pressure, and obesity-anthropometric markers in macrosomic offspring of nondiabetic mothers. Diabetes Care. 2006;29:1197–201.
Mullett MD, Cottrell L, Lilly C, Gadikota K, Dong L, Hobbs G, et al. Association between birth characteristics and coronary disease risk factors among fifth graders. J Pediatr. 2014;164:78–82.
Li Y, Wu J, Yu J, Gao E, Meads C, Afnan M, et al. Is fetal macrosomia related to blood pressure among adolescents? A birth cohort study in China. J Hum Hypertens. 2013;27:686–92.
Ornoy A. Growth and neurodevelopmental outcome of children born to mothers with pregestational and gestational diabetes. Pediatr Endocrinol Rev. 2005;3:104–13.
Funding
None.
Author information
Authors and Affiliations
Contributions
JZ and HDC conceived the research. FF analyzed data and drafted the manuscript. All authors were involved in revising the paper critically and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethical approval
Anonymized data were used for this study, rendering an ethical approval unnecessary by the Institutional Review Board of Xinhua Hospital.
Conflict of interest
All authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Fang, F., Zhang, QY., Zhang, J. et al. Risk factors for recurrent macrosomia and child outcomes. World J Pediatr 15, 289–296 (2019). https://doi.org/10.1007/s12519-019-00249-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12519-019-00249-z