Abstract
Background
Mizoribine (MZR) is an immunosuppressant used to treat adult nephropathy. There is little experience with the drug in treating Chinese children with frequently relapsing nephrotic syndrome (FRNS). We investigated the efficacy and safety for treating MZR with FRNS. Furthermore, the relationship between efficacy and serum concentration was investigated.
Methods
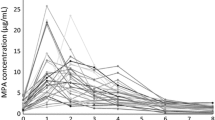
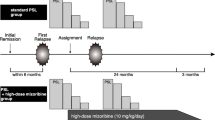
A prospective multicenter observational 12-month study was performed for evaluating the usefulness of MZR with FRNS. Serum MZR concentration was measured, and the relationships between pharmacokinetic parameters (Cmax, AUC), number of relapses, and urinary protein were evaluated.
Results
Eighty-two pediatric patients from four hospitals were treated with MZR and prednisone. MZR treatment significantly reduced the number of relapses and steroid doses. A correlation between pharmacokinetic parameters and relapses was observed, which fits well with the sigmoidal Emax model. Even in the relationship between pharmacokinetic parameters and urinary proteins, it was recognized that there was a threshold in the pharmacokinetic parameters for the therapeutic effect similar to the results obtained with the sigmoidal Emax model. Eleven patients (13.4%) experienced mild adverse events.
Conclusions
MZR therapy was effective in reducing the number of relapses and steroid doses. No severe adverse reactions were observed. Therapeutically effective serum concentrations were estimated to be Cmax ≥ about 2 μg/mL or AUC ≥ about 10 μg h/mL. MZR and steroid treatment were effective and safe for pediatric FRNS.



Similar content being viewed by others
References
KDIGO Clinical Practice Guideline for Glomerulonephritis. Chapter 3: Steroid-sensitive nephrotic syndrome in children. Kidney Int. 2012;2:163–71.
Koskimies O, Vilska J, Rapola J, Hallman N. Long-term outcome of primary nephrotic syndrome. Arch Dis Child. 1982;57:544–8.
Tarshish P, Tobin JN, Bernstein J, Edelmann CM Jr. Prognostic significance of the early course of minimal change nephrotic syndrome: report of the International Study of Kidney Disease in Children. J Am Soc Nephrol. 1997;8:769–76.
Kyrieleis HA, Löwik MM, Pronk I, Cruysberg HR, Kremer JA, Oyen WJ, et al. Long-term outcome of biopsy-proven, frequently relapsing minimal-change nephrotic syndrome in children. Clin J Am Soc Nephrol. 2009;4:1593–600.
Niaudet P, Broyer M, Habib R. Treatment of idiopathic nephrotic syndrome with cyclosporin A in children. Clin Nephrol. 1991;35(Suppl 1):S31–6.
El-Husseini A, El-Basuony F, Mahmoud I, Sheashaa H, Sabry A, Hassan R, et al. Long-term effects of cyclosporine in children with idiopathic nephrotic syndrome: a single-centre experience. Nephrol Dial Transplant. 2005;20:2433–8.
Dötsch J, Dittrich K, Plank C, Rascher W. Is tacrolimus for childhood steroid dependent nephrotic syndrome better than ciclosporin A? Nephrol Dial Transplant. 2006;21:1761–3.
Behrend M. Adverse gastrointestinal effects of mycophenolate mofetil: aetiology, incidence and management. Drug Saf. 2001;24:645–63.
Koyama H, Tsuji M. Genetic and biochemical studies on the activation and cytotoxic mechanism of Bredinin, a potent inhibitor of purine biosynthesis in mammalian cells. Biochem Pharmacol. 1983;32:3547–53.
Kusumi T, Tsuda M, Katsunuma T, Yamamura M. Dual Inhibitory effect of bredinin. Cell Biochem Funct. 1989;7:201–4.
Turka LA, Dayton J, Sinclair G, Thompson CB, Mitchell BS. Guanine ribonucleotide depletion inhibits T cell activation. Mechanism of action of the immunosuppressive drug mizoribine. J Clin Invest. 1991;87:940–8.
Takahashi S, Wakui H, Gustafsson JA, Zilliacus J, Itoh H. Functional interaction of the immunosuppressant mizoribine with the 14-3-3 protein. Biochem Biophys Res Commun. 2000;274:87–92.
Kawasaki Y, Takano K, Isome M, Suzuki J, Suyama K, Kanno H, et al. Efficacy of single dose of oral mizoribine pulse therapy two times per week for frequently relapsing nephrotic syndrome. J Nephrol. 2007;20:52–6.
Ohtomo Y, Fujinaga S, Takada M, Murakami H, Akashi S, Shimizu T, et al. High-dose mizoribine therapy for childhood-onset frequently relapsing steroid-dependent nephrotic syndrome with cyclosporin nephrotoxicity. Pediatr Nephrol. 2005;20:1744–9.
Fujinaga S, Hirano D, Nishizaki N, Someya T, Ohtomo Y, Ohtsuka Y, et al. Single daily high-dose mizoribine therapy for children with steroid-dependent nephrotic syndrome prior to cyclosporine administration. Pediatr Nephrol. 2011;26:479–83.
Kawasaki Y. Mizoribine: a new approach in the treatment of renal disease. Clin Dev Immunol. 2009;2009:681482.
Xing S, Yang J, Zhang X, Zhou P. Comparative efficacy and safety of mizoribine with mycophenolate mofetil for Asian renal transplantation—a meta-analysis. Clin Biochem. 2014;47:663–9.
Hosotsubo H, Takahara S, Taenaka N. Simplified high-performance liquid chromatographic method for determination of mizoribine in human serum. J Chromatogr. 1988;432:340–5.
Ishida K, Kaneda H, Uemura O, Ushijima K, Ohta K, Goto Y, et al. Evaluation of limited sampling designs to estimate maximal concentration and area under the curve of mizoribine in pediatric patients with renal disease. Drug Metab Pharmacokinet. 2011;26:71–8.
Kuroda T, Hirose S, Tanabe N, Sato H, Nakatsue T, Ajiro J, et al. Mizoribine therapy for patients with lupus nephritis: the association between peak mizoribine concentration and clinical efficacy. Mod Rheumatol. 2007;17:206–12.
Tanaka H, Tsugawa K, Nakahata T, Kudo M, Suzuki K, Ito E. Implication of the peak serum level of mizoribine for control of the serum anti-dsDNA antibody titer in patients with lupus nephritis. Clin Nephrol. 2005;63:417–22.
Choe S, Lee D. Parameter estimation for sigmoid Emax models in exposure–response relationship. Transl Clin Pharmacol. 2017;25:74–84.
Yoshioka K, Ohashi Y, Sakai T, Ito H, Yoshikawa N, Nakamura H, et al. A multicenter trial of mizoribine compared with placebo in children with frequently relapsing nephrotic syndrome. Kidney Int. 2000;58:317–24.
Yoshikawa N, Nakanishi K, Ishikura K, Hataya H, Iijima K, Honda M. Japanese Pediatric IgA Nephropathy Treatment Study Group. Pediatr Nephrol. 2008;23:757–63.
Saito T, Iwano M, Matsumoto K, Mitarai T, Yokoyama H, Yorioka N, et al. Mizoribine therapy combined with steroids and mizoribine blood concentration monitoring for idiopathic membranous nephropathy with steroid-resistant nephrotic syndrome. Clin Exp Nephrol. 2017;21:961–70.
Sonda K, Takahashi K, Tanabe K, Funchinoue S, Hayasaka Y, Kawaguchi H, et al. Clinical pharmacokinetic study of mizoribine in renal transplantation patients. Transpl Proc. 1996;28:3643–8.
Funding
This study was supported by a grant from the medical innovation team project of Jiangsu Province, China (grant number CXTDA2017022). The authors thank the participants and their parents, and other persons who assisted in undertaking this study. The funders had no role in drafting or submitting this manuscript.
Author information
Authors and Affiliations
Contributions
YFG, LPR, XQD, and QS contributed to the study design, collection, evaluation, and interpretation of the data. XYJ, ZWY, HX, and ZKX contributed to the study design. All authors contributed to the critical revision and final approval of the manuscript.
Corresponding author
Ethics declarations
Ethical approval
This study was approved by the Institutional Ethics Committee of Nanjing University School of Medicine.
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Xia, ZK., Gao, YF., Rong, LP. et al. Usefulness of mizoribine administration in children with frequently relapsing nephrotic syndrome, and the relationship between pharmacokinetic parameters and efficacy: a multicenter prospective cohort study in China. World J Pediatr 15, 262–269 (2019). https://doi.org/10.1007/s12519-019-00241-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12519-019-00241-7