Abstract
Background
Bloodstream infections (BSIs) cause significant morbidity and mortality of children worldwide. The aim of this study was to investigate BSI in children and determine the identity of causative organism and their susceptibility patterns in a metropolitan public hospital in Australia.
Methods
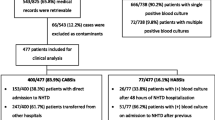
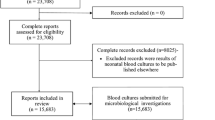
We retrospectively reviewed children aged 0–16 years admitted to a public hospital from January 1, 2010 to August 31, 2014 inclusive, and whose blood cultures revealed bacteraemia. Data were collected regarding patient demographics, species of bacteria isolated, antimicrobial susceptibility of these isolates, and clinical outcomes.
Results
Out of 96 patients with BSI, 55 (57.3%) were males. The median age was 3.35 years (IQR 0.44–7.46), and there were 2 mortalities. Common sites of infection were the respiratory tract (16.6%, n = 16), bone and joints (15.6%, n = 15) and the urinary tract (11.5%, n = 11). The most frequent isolates were Staphylococcus aureus (27.0%), Escherichia coli (14.0%) and Streptococcus pneumoniae (12.0%). Whilst most bacterial isolates displayed susceptibility (> 90%) to common antimicrobial agents, only 57.1% (8/14) of Escherichia coli isolates were susceptible to ampicillin and 58.3% (7/12) were susceptible to co-trimoxazole.
Conclusions
Gram-positive bacteria accounted for the majority of pediatric BSIs, of which invasive pneumococcal disease remains a noteworthy cause. The majority of isolates, except Escherichia coli, were susceptible to commonly used antimicrobials. This study confirms the knowledge of high rates of resistance of Escherichia coli to ampicillin. Therefore, empirical treatment should still include gentamicin. Monitoring of resistance patterns is warranted to ensure that antibiotic therapy remains appropriate.
Similar content being viewed by others
References
Plunkett A, Tong J. Sepsis in children. BMJ. 2015;350:h3017.
Watson RS, Carcillo JA. Scope and epidemiology of pediatric sepsis. Pediatr Crit Care Med. 2005;6(Suppl 3):S3–5.
Goldstein B, Giroir B, Randolph A, International Consensus Conference on Pediatric Sepsis. International pediatric sepsis consensus conference: definitions for sepsis and organ dysfunction in pediatrics. Pediatr Crit Care Med. 2005;6:2–8.
Mangia CMF, Kissoon N, Carcillo JA. Sepsis and septic shock: a global overview. J Pediat Infect Dis. 2009;4:71–6.
Kissoon N, Carcillo JA, Espinosa V, Argent A, Devictor D, Madden M, et al. World federation of pediatric intensive care and critical care societies: global sepsis initiative. Pediatr Crit Care Med. 2011;12:494–503.
Black RE, Morris SS, Bryce J. Where and why are 10 million children dying every year? Lancet. 2003;361:2226–34.
Rhodes A, Evans LE, Alhazzani W, Levy MM, Antonelli M, Ferrer R, et al. Surviving sepsis campaign: international guidelines for management of sepsis and septic shock: 2016. Intensive Care Med. 2017;43:304–77.
Okeke IN, Laxminarayan R, Bhutta ZA, Duse AG, Jenkins P, O’Brien TF, et al. Antimicrobial resistance in developing countries. Part I: recent trends and current status. Lancet Infect Dis. 2005;5:481–93.
Aiken AM, Allegranzi B, Scott JA, Mehtar S, Pittet D, Grundmann H. Antibiotic resistance needs global solutions. Lancet Infect Dis. 2014;14:550–1.
Downie L, Armiento R, Subhi R, Kelly J, Clifford V, Duke T. Community-acquired neonatal and infant sepsis in developing countries: efficacy of WHO’s currently recommended antibiotics—systematic review and meta-analysis. Arch Dis Child. 2013;98:146–54.
Voss A, Milatovic D, Wallrauch-Schwarz C, Rosdahl VT, Braveny I. Methicillin-resistant Staphylococcus aureus in Europe. Eur J Clin Microbiol Infect Dis. 1994;13:50–5.
Bertrand X, Dowzicky MJ. Antimicrobial susceptibility among gram-negative isolates collected from intensive care units in North America, Europe, the Asia-Pacific Rim, Latin America, the Middle East, and Africa Between 2004 and 2009 as part of the Tigecycline Evaluation and Surveillance Trial. Clin Ther. 2012;34:124–37.
Lubowski TJ, Woon JL, Hogan P, Hwang CC. Differences in antimicrobial susceptibility among hospitals in an integrated health system. Infect Control Hosp Epidemiol. 2001;22:379–82.
Greenhow TL, Hung YY, Herz AM. Changing epidemiology of bacteremia in infants aged 1 week to 3 months. Pediatrics. 2012;129:e590–6.
Choffnes ER, Relman DA, Mack A. Antibiotic resistance: implications for global health and novel intervention strategies: workshop summary. Washington: National Academic Press; 2010.
Basmaci R, Bielicki J, Daniels R, Kissoon N, Ellis S, Balasegaram M, et al. Management of children with multidrug-resistant sepsis in low-income and middle-income countries. Lancet Child Adolesc Health. 2018;2:8–10.
Liu C, Bayer A, Cosgrove SE, Daum RS, Fridkin SK, Gorwitz RJ, et al. Clinical practice guidelines by the infectious diseases society of america for the treatment of methicillin-resistant Staphylococcus aureus infections in adults and children: executive summary. Clin Infect Dis. 2011;52:285–92.
Khaertynov KS, Anokhin VA, Rizvanov AA, Davidyuk YN, Semyenova DR, Lubin SA, et al. Virulence factors and antibiotic resistance of Klebsiella pneumoniae strains isolated from neonates with sepsis. Front Med (Lausanne). 2018;5:225.
Laxminarayan R, Matsoso P, Pant S, Brower C, Røttingen JA, Klugman K, et al. Access to effective antimicrobials: a worldwide challenge. Lancet. 2016;387:168–75.
MacDougall C, Polk RE. Antimicrobial stewardship programs in health care systems. Clin Microbiol Rev. 2005;18:638–56.
Cruickshank M, Ferguson J, Bull A. Reducing harm to patients from health care associated infection: the role of surveillance. Chapter 3: surgical site infection—an abridged version. Healthc Infect. 2009;14:109–14.
National Safety and Quality Health Service Standards: Australian Commission on Safety and Quality in Health Care. 2012. Accessed 10 Oct 2018.
Adam HJ, Baxter MR, Davidson RJ, Rubinstein E, Fanella S, Karlowsky JA, et al. Comparison of pathogens and their antimicrobial resistance patterns in paediatric, adult and elderly patients in Canadian hospitals. J Antimicrob Chemoth. 2013;68(Suppl 1):i31–7.
Boggan JC, Navar-Boggan AM, Jhaveri R. Pediatric-specific antimicrobial susceptibility data and empiric antibiotic selection. Pediatrics. 2012;130:e615–22.
Horan TC, Andrus M, Dudeck MA. CDC/NHSN surveillance definition of health care-associated infection and criteria for specific types of infections in the acute care setting. Am J Infect Control. 2008;36:309–32.
Er J, Wallis P, Maloney S, Norton R. Paediatric bacteraemias in tropical Australia. J Paediatr Child Health. 2015;51:437–42.
Engelman D, Hofer A, Davis JS, Carapetis JR, Baird RW, Giffard PM, et al. Invasive Staphylococcus aureus infections in children in tropical Northern Australia. J Pediatric Infect Dis Soc. 2014;3:304–11.
Henderson KL, Johnson AP, Muller-Pebody B, Charlett A, Gilbert R, Sharland M. The changing aetiology of paediatric bacteraemia in England and Wales, 1998–2007. J Med Microbiol. 2010;59:213–9.
Orrett FA, Changoor E. Bacteremia in children at a regional hospital in Trinidad. Int J Infect Dis. 2007;11:145–51.
Laupland KB, Gregson DB, Vanderkooi OG, Ross T, Kellner JD. The changing burden of pediatric bloodstream infections in Calgary, Canada, 2000–2006. Pediatr Infect Dis J. 2009;28:114–7.
Sharma M, Goel N, Chaudhary U, Aggarwal R, Arora DR. Bacteraemia in children. Indian J Pediatr. 2002;69:1029–32.
Dramowski A, Cotton MF, Rabie H, Whitelaw A. Trends in paediatric bloodstream infections at a South African referral hospital. BMC Pediatr. 2015;15:33.
Doit C, Mariani-Kurkdjian P, Mahjoub-Messai F, Bidet P, Bonacorsi S, Carol A, et al. Epidemiology of pediatric community-acquired bloodstream infections in a children hospital in Paris, France, 2001–2008. Diagn Microbiol Infect Dis. 2010;66:332–5.
Madrid L, Seale AC, Kohli-Lynch M, Edmond KM, Lawn JE, Heath PT, et al. Infant Group B Streptococcal disease incidence and serotypes worldwide: systematic review and meta-analyses. Clin Infect Dis. 2017;65(Suppl 2):S160–72.
Polin RA, Committee on Fetus and Newborn. Management of neonates with suspected or proven early-onset bacterial sepsis. Pediatrics. 2012;129:1006–15.
Allen UD, MacDonald N, Fuite L, Chan F, Stephens D. Risk factors for resistance to “first-line” antimicrobials among urinary tract isolates of Escherichia coli in children. Can Med Assoc J. 1999;160:1436–40.
Sepsis NEONATAL First Dose. Empirical Parenteral Antibiotic Guideline v2.1. 2013. Accessed 10 Oct 2018.
Sepsis PAEDIATRIC First Dose. Empirical Parenteral Antibiotic Guideline v2.1. 2013. Accessed 10 Oct 2018.
Versporten A, Bielicki J, Drapier N, Sharland M, Goossens H, ARPEC project group. The Worldwide Antibiotic Resistance and Prescribing in European Children (ARPEC) point prevalence survey: developing hospital-quality indicators of antibiotic prescribing for children. J Antimicrob Chemother. 2016;71:1106–17.
Aldeyab MA, Monnet DL, Lopez-Lozano JM, Hughes CM, Scott MG, Kearney MP, et al. Modelling the impact of antibiotic use and infection control practices on the incidence of hospital-acquired methicillin-resistant Staphylococcus aureus: a time-series analysis. J Antimicrob Chemother. 2008;62:593–600.
Fuchs A, Bielicki J, Mathur S, Sharland M, Van Den Anker JN. Antibiotic Use for Sepsis in Neonates and Children: 2016 Evidence Update. WHO Reviews. Accessed 16 Nov 2018.
Funding
None.
Author information
Authors and Affiliations
Contributions
SMS contributed to data acquisition, data analysis and interpretation, and drafting of the manuscript. JW contributed to conception and design, data analysis and interpretation, and revision of the manuscript. PM contributed to obtaining of the ethics approval, data analysis and interpretation, revision of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
This study was approved by Human Research Ethics Committee of South Western Sydney Local Health District.
Conflict of interest
No financial or nonfinancial benefits have been received or will be received from any party related directly or indirectly to the subject of this article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Shakur, S.M., Whitehall, J. & Mudgil, P. Pediatric bloodstream infections in metropolitan Australia. World J Pediatr 15, 161–167 (2019). https://doi.org/10.1007/s12519-018-00221-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12519-018-00221-3