Abstract
Background
Considering the fact that Pakistan is amongst the countries with very high neonatal mortality rates, we conducted a research study to determine the possible causes and characteristics of neonates presenting dead to the emergency department of tertiary public health care facilities of Pakistan using verbal autopsies.
Methods
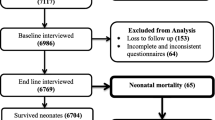
A descriptive case series study was conducted in emergency department/pediatrics ward/neonatal ward/nursery unit of ten tertiary care public health facilities, situated in seven major cities of Pakistan from November, 2011 to June, 2013. Precoded verbal autopsy proforma was used to collect information regarding cause of death, family narratives and other associated risks accountable for pathway to mortality.
Results
We identified 431 neonates presenting dead to the emergency department (238 males and 193 females). Sepsis (26.7%), birth asphyxia (18.8%) and persistent pulmonary arrest (17.2%) were main primary causes of brought death. Around 72% brought dead neonates were referred from doctors/health care facilities and more than 28% caregivers mentioned that they were not informed about the diagnosis/ailment of their deceased newborn.
Conclusions
Findings of our study suggest that infectious disease remains the main primary cause of neonatal mortality. Underweight in newborns (64%) was estimated as a leading associated risk. Delays in referrals to respective health care facility enlightened the concern of sub-standard prerequisites of neonatal care that could be one of the major contributing risk factor of high mortality rates.
Similar content being viewed by others
References
Bartlett LA, Mawji S, Whitehead S, Crouse C, Dalil S, Ionete D, et al. Where giving birth is a forecast of death: maternal mortality in four districts of Afghanistan, 1999-2002. Lancet 2005;365:864–870.
Black RE, Cousens S, Johnson HL, Lawn JE, Rudan I, Bassani DG, et al. Global, regional, and national causes of child mortality in 2008: a systematic analysis. Lancet 2010;375:1969–1987.
Stoll BJ. The global impact of neonatal infection. Clin Perinatol 1997;24:1–21.
College of Physicians and Surgeons, Pakistan. CPSP Reproductive health, a manual for physician. Karachi: CPSP, 2002.
World Health Organization. Health action in crises: Pakistan, The present context. 2008. http://www.who.int/hac/crises/pak/Pakistan_Aug08.pdf (accessed December 30, 2014).
Mahmood A, Sultan M. Child Health. Pakistan Demographic and Health Survey 2006-07. Islamabad, Pakistan: National Institute of Population Studies and Macro International Inc., 2008: 123–145.
Bhutta ZA, Hyder AA, Ali N. Defining a new challenge for health systems: Perinatal health in Pakistan. In: Bhutta ZA, eds. Perinatal and newborn care in South Asia: Priorities and action. Pakistan: Oxford University Press, 2007: 1–30.
Darmstadt GL, Bhutta ZA, Cousens S, Adam T, Walker N, de Bernis L, et al. Evidence-based, cost-effective interventions: how many newborn babies can we save? Lancet 2005;365:977–988.
Jehan I, Harris H, Salat S, Zeb A, Mobeen N, Pasha O, et al. Neonatal mortality, risk factors and causes: a prospective population-based cohort study in urban Pakistan. Bull. World Health Organ 2009;87:130–138.
Save the Children USA. Saving Newborns Lives Initiative. State of the World’s Newborns. Save the Children USA: Washington, DC, 2001.
Fikree FF, Gray RH. Demographic survey of the level and determinants of perinatal mortality in Karachi, Pakistan. Paediatr Perinat Epidemiol 1996;10:86–96.
Jalil F, Lindblad BS, Hanson LÅ, Khan SR, Yaqoob M, Karlberg J. Early child health in Lahore, Pakistan: IX. Perinatal events. Acta Paediatr Suppl 1993;82:95–107.
World Health Organization. World population data sheet. 2004. http://www.prb.org/pdf04/04worlddatasheet_eng.pdf (Accessed September 23, 2014).
Black RE, Coldham C, Kalter H, Quigley MA, Ross D, Snow RW. A standard verbal autopsy method for investigating causes of death in infants and children. Geneva: World Health Organization, 1999.
Bang AT, Bang RA. Diagnosis of causes of childhood deaths in developing countries by verbal autopsy: suggested criteria. The SEARCH Team. Bull World Health Organ 1992;70:499–507.
World Health Organization. Technical consultation on verbal autopsy tools. Geneva: World Health Organization, 2005.
Anker M. The effect of misclassification error on reported causespecifi c mortality fractions from verbal autopsy. Int J Epidemiol 1997;26:1090–1096.
Black RE, Morris SS, Bryce J. Where and why are 10 million children dying every year? Lancet 2003;361:2226–2234.
Bhutta ZA. Epidemiology of neonatal sepsis in Pakistan: an analysis of available evidence and implications for care. J Coll Physicians Surg Pak 1996;6:12–17.
Ahmed MF. Infant mortality in Bangladesh: a review of recent evidence. J Biosoc Sci 1991;23:327–336.
Fauveau V, Wojtyniak B, Mostafa G, Sarder AM, Chakraborty J. Perinatal mortality in Matlab, Bangladesh: a community-based study. Int J Epidemiol 1990;19:606–612.
Fikree FF, Berendes HW. Risk factors for term intrauterine growth retardation: a community-based study in Karachi. Bull World Health Organ 1994;72:581–587.
UNDP. Infants with low birth weight. http://hdrstats.undp.org/indicators/67.html (accessed December 17, 2014).
Najmi RS. Distribution of birth weights of hospital born Pakistani infants. J Pak Med Assoc 2000;50:121–124.
Naheed I, Yasin A. Determinants of low birth weight babies (A prospective study of associated factors and outcome). Ann King Edward Med Coll 2000;6:361.
Aziz S, Billoo AG, Samad NJ. Impact of socioeconomic conditions on prenatal mortality in Karachi. J Pak Med Assoc 2001;51:354–359.
Mustufa MA, Korejo R, Shahid A, Nasim S. Infection remains a leading cause of neonatal mortality among infants delivered at a tertiary hospital in Karachi, Pakistan. J Infect Dev Ctries 2014;8:1470–1475.
Das J, Hammer J, Leonard K. The quality of medical advice in low-income countries. J Econ Perspect 2008;22:93–114.
Jashnani KD, Rupani AB, Wani RJ. Maternal mortality: an autopsy audit. J Postgrad Med 2009;55:12–16.
Ramanathan M. Addressing the’third delay’in maternal mortality: need for reform. Indian J Med Ethics 2009;6:211–212.
DiGiuseppe DL, Aron DC, Ranbom L, Harper DL, Rosenthal GE. Reliability of birth certificate data: a multi-hospital comparison to medical records information. Matern Child Health J 2002;6:169–179.
Roohan PJ, Josberger RE, Acar J, Dabir P, Feder HM, Gagliano PJ. Validation of birth certificate data in New York State. J Community Health 2003;28:335–346.
Lydon-Rochelle MT, Holt VL, Cárdenas V, Nelson JC, Easterling TR, Gardella C, et al. The reporting of pre-existing maternal medical conditions and complications of pregnancy on birth certificates and in hospital discharge data. Am J Obstet Gynecol 2005;193:125–134.
Rossen J, Okland I, Nilsen OB, Eggebo TM. Is there an increase of postpartum hemorrhage, and is severe hemorrhage associated with more frequent use of obstetric interventions? Acta Obstet Gynecol Scand 2010;89:1248–1255.
Shamsa A, Bai J, Raviraj P, Gyaneshwar R. Mode of delivery and its associated maternal and neonatal outcomes. Open J Obstet Gynecol 2013;3:307–312.
Acknowledgements
All the authors are thankful to PMRC for providing funds. The project was Conducted under PMRC grant no.4-17-1/09/RDC/Multicenter/Verbal Autopsy/NICH.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Mustufa, M.A., Sheikh, M.A., Taseer, IuH. et al. Trajectory of cause of death among brought dead neonates in tertiary care public facilities of Pakistan: A multicenter study. World J Pediatr 13, 57–62 (2017). https://doi.org/10.1007/s12519-016-0063-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12519-016-0063-5