Abstract
Background
Little was known about the therapeutic result of rhabdomyosarcomas (RMSs) and other malignant tumors until the end of the last century in China. Very few prospective clinical research results have been reported. We designed a RS-99 protocol under close cooperation of a multidisciplinary team including surgeons, radiologists, pathologists, and pediatric oncologists at Shanghai Children’s Medical Center. This study aimed to improve the prognosis of childhood solid tumors and analyze the results of different tumors with the same protocol, including RMSs, the Ewing sarcoma family of tumors (ESFTs), and ex-cranial germ cell tumors (GCTs).
Methods
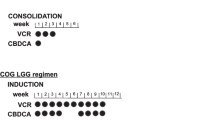
Sixty-six patients with malignant solid tumors [RMS (n=30), GCT (n=22), and ESFT (n=14)] were enrolled on the RS-99 protocol from October 1998 to October 2006. They were 34 girls and 32 boys aged 9 to 194 months. The protocol involved surgery, radiotherapy and chemotherapy which included VCP (vincristine, cisdiaminedichloroplatinum, and cyclophosphamide) and IEV (etoposide, vincristine and ifosfamide) for the low-risk group, AVCP (adriamycin, vincristine, cisdiaminedichloroplatinum, and cyclophosphamide) and IEV for the intermediate-risk group and high-risk group. Peripheral blood stem cell transplantation was suggested for the high-risk group. Radiotherapy was only given for RMS and ESFT. Differences in survival between the groups were determined by comparison of entire survival curves and tested by the Kaplan-Meier method and the log-rank tests.
Results
The 5-year event-free survival (EFS) for the whole group (RMS, ESFT and GCT) was 60%. The 5-year EFS for children with RMS was 35% (95% CI 16–54), GCT was 79% (95% CI 70–88) and ESFT was 72% (95% CI 58–86). The 5-year EFS showed that the patients with RMS in the retroperitoneum-pelvis did not have a better result than those with tumors in other sites (P=0.604). The histological classification of RMS exerted prognostic influence on the estimated 5-year EFS (P=0.04). Tumor stage and risk group were also contributive to prognosis (P=0.008). For GCT patients, the primary sites of tumors and their histological classification did not influence the therapeutic result (P=0.814). The 5-year EFS was 100% in stage I and II versus 62% in stage III and IV patients (P=0.02). Because of the small number of patients, we did not analyze the prognostic factors for patients with ESFT. No organ failure or functional impairment occurred in the patients enrolled in the RS-99 protocol. One ESFT patient developed a second cancer.
Conclusions
The RS-99 protocol is well tolerated and is reasonable for the 3 different tumors. Risk-based grouping protocol design is needed and the protocol for high risk RMS should be revised.
Similar content being viewed by others
References
Pappo AS, Shapiro DN, Crist WM, Maurer HM. Biology and therapy of pediatric rhabdomyosarcoma. J Clin Oncol 1995;13:2123–2139.
Raney RB, Anderson JR, Barr FG, Donaldson SS, Pappo AS, Qualman SJ, et al. Rhabdomyosarcoma and undifferentiated sarcoma in the first two decades of life: a selective review of the Intergroup Rhabdomyosarcoma Study Group experience and rationale for Intergroup Rhabdomyosarcoma Study V. J Pediatr Hematol Oncol 2001;23:215–220.
Pappo AS, Meza JL, Donaldson SS, Wharam MD, Wiener ES, Qualman SJ, et al. Treatment of localized nonorbital, nonparameningeal head and neck rhabdomyosarcoma: lessons learned from intergroup rhabdomyosarcoma studies III and IV. J Clin Oncol 2003;21:638–645.
Crist WM, Anderson JR, Meza JL, Fryer C, Raney RB, Ruymann FB, et al. Intergroup rhabdomyosarcoma study-IV: results for patients with nonmetastatic disease. J Clin Oncol 2001;19:3091–3102.
Lertkhachonsuk R, Manchana T, Termrungruanglert W, Vasuratna A, Sittisomwong T, Worasethsin P, et al. Outcome of recurrent and persistent disease of malignant ovarian germ cell tumor: a retrospective analysis at King Chulalongkorn Memorial Hospital. J Med Assoc Thail 2006;89:138–144.
Kolb EA, Kushner BH, Gorlick R, Laverdiere C, Healey JH, LaQuaglia MP, et al. Long-term event-free survival after intensive chemotherapy for Ewing’s family of tumors in children and young adults. J Clin Oncol 2003;21:3423–3430.
Lu KH, Gershenson DM. Update on the management of ovarian germ cell tumors. J Reprod Med 2005;50:417–425.
Koscielniak E, Harms D, Henze G, Jürgens H, Gadner H, Herbst M, et al. Results of treatment for soft tissue sarcoma in childhood and adolescence: a final report of the German Cooperative Soft Tissue Sarcoma Study CWS-86. J Clin Oncol 1999;17:3706–3719.
Lawrence W Jr, Anderson JR, Gehan EA, Maurer H. Pretreatment TNM staging of childhood rhabdomyosarcoma: a report of the Intergroup Rhabdomyosarcoma Study Group. Cancer 1997;80:1165–1170.
Meyers PA, Krailo MD, Ladanyi M, Chan KW, Sailer SL, Dickman PS, et al. High-dose melphalan, etoposide, totalbody irradiation, and autologous stemcell reconstitution as consolidation therapy for high-risk Ewing’s sarcoma does not improve prognosis. J Clin Oncol 2001;19:2812–2820.
Duchesne GM, Stenning SP, Aass N, Mead GM, Fosså SD, Oliver RT, et al. Radiotherapy after chemotherapy for metastatic seminoma—a diminishing role. MRC Testicular Tumour Working Party. Eur J Cancer 1997;33:829–835.
Pizzo PA, Poplack DG. Principles and practice of pediatric oncology. Philadelphia: Lippincott Williams & Wilkins, 2002:1017–1050.
Breitfeld PP, Lyden E, Raney RB, Teot LA, Wharam M, Lobe T, et al. Ifosfamide and etoposide are superior to vincristine and melphalan for pediatric metastatic rhabdomyosarcoma when administered with irradiation and combination chemotherapy: a report from the Intergroup Rhabdomyosarcoma Study Group. J Pediatr Hematol Oncol 2001;23:334–337.
Donaldson SS, Meza J, Breneman JC, Crist WM, Laurie F, Qualman SJ, et al. Results from the IRS-IV randomized trial of hyperfractionated radiotherapy in children with rhabdomyosarcoma—a report from the IRSG. Int J Radiat Oncol Biol Phys 2001;51:718–728.
Carli M, Colombatti R, Oberlin O, Bisogno G, Treuner J, Koscielniak E, et al. European intergroup studies (MMT4-89 and MMT4-91) on childhood metastatic rhabdomyosarcoma: final results and analysis of prognostic factors. J Clin Oncol 2004;22:4787–4794.
Flamant F, Rodary C, Rey A, Praquin MT, Sommelet D, Quintana E, et al. Treatment of non-metastatic rhabdomyosarcomas in childhood and adolescence: results of the second study of the International Society of Paediatric Oncology: MMT84. Eur J Cancer 1998;34:1050–1062.
George DW, Foster RS, Hromas RA, Einhorn LH. Update on late relapse of germ cell tumor: a clinical and molecular analysis. J Clin Oncol 2003;21:113–122.
Modak S, Gardner S, Dunkel IJ, Balmaceda C, Rosenblum MK, Miller DC, et al. Rosenblum. Thiotepa-based high-dose chemotherapy with autologous stem-cell rescue in patients with recurrent or progressive CNS germ cell tumors. J Clin Oncol 2004;22:1934–1943.
Bacci G, Ferrari S, Longhi A, Donati D, Barbieri E, Forni C, et al. Role of surgery in local treatment of Ewing’s sarcoma of the extremities in patients undergoing adjuvant and neoadjuvant chemotherapy. Oncol Rep 2004;11:111–120.
Dunst J, Schuck A. Role of radiotherapy in Ewing tumors. Pediatr Blood Cancer 2004;42:465–470.
Grier HE, Krailo MD, Tarbell NJ, Link MP, Fryer CJ, Pritchard DJ, et al. Addition of ifosfamide and etoposide to standard chemotherapy for Ewing’s sarcoma and primitive neuroectodermal tumor of bone. N Engl J Med 2003;348:694–701.
Meyers PA. High-dose therapy with autologous stem cell rescue for pediatric sarcomas. Curr Opin Oncol 2004;16:120–125.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Cai, JY., Tang, JY., Pan, C. et al. Results of RS-99 protocol for childhood solid tumors. World J Pediatr 6, 43–49 (2010). https://doi.org/10.1007/s12519-010-0005-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12519-010-0005-6