Abstract
Due to a tremendous increase in imaging usage in the last decades, in particular of myocardial perfusion imaging with radionuclide tracers, significant concerns have been recently raised on the possible harmful effect of the exposure of patients and health care operators to ionizing radiation. Recent estimates indicate that cardiac imaging procedures account for almost 40 % of the cumulative dose for imaging procedures. Thus, pertinent scientific associations published recommendations directed to limit patients’ exposure. The key points in the dose optimization process, including appropriate patients selection, stress test and study protocol, new processing software and new hardware, are described.


Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Shaw LJ, Hendel R, Borges-Neto S, et al. Prognostic value of normal exercise and adenosine 99m Tc-tetrofosmin SPECT imaging: results from the multicenter registry of 4,728 patients. J Nucl Med. 2003;44:134–9.
Underwood SR, Anagnostopoulos C, Cerqueira M, et al. Myocardial perfusion scintigraphy: the evidence. Eur J Nucl Med Mol Imaging. 2004;31:261–91.
Parker MW, Iskandar A, Limone B, et al. Diagnostic accuracy of cardiac positron emission tomography versus single photon emission computed tomography for coronary artery disease. Clinical perspective: a bivariate meta-analysis. Circ Cardiovasc Imaging. 2012;5:700–7.
Cremer P, Hachamovicth R, Tamarappoo B. Clinical decision making with myocardial perfusion imaging in patients with known or suspected coronary artery disease. Semin Nucl Med. 2014;44:320–9. Interesting review on the usefulness of MPI in the clinical decision making process.
Berrington de Gonzalez A, Mahesh M, Kim KP, et al. Projected cancer risks from computed tomographic scans performed in the United States in 2007. Arch Intern Med. 2009;169:2071–7.
Committee to Assess Health Risks from Exposure to Low Levels of Ionizing Radiation, Nuclear and Radiation Studies Board, Division on Earth and Life Studies, National Research Council of the National Academies. Health risks from exposure to low levels of ionizing radiation: BEIR VII phase 2. Washington, DC: National Academies Press; 2006.
Hill KD, Einstein AJ. New approaches to reduce radiation exposure. Trends Cardiovasc Med. 2015. A review on the possible strategies to contain patients’ radiation exposure .
Gerber TC, Carr JJ, Arai AE, et al. Ionizing radiation in cardiac imaging: a science advisory from the American Heart Association Committee on Cardiac Imaging of the Council on Clinical Cardiology and Committee on Cardiovascular Imaging and Intervention of the Council on Cardiovascular Radiology and Intervention. Circulation. 2009;119:1056–65.
Cerqueira MD, Allman KC, Ficaro EP, et al. Recommendations for reducing radiation exposure in myocardial perfusion imaging. J Nucl Cardiol. 2010;17(4):709–18.
Shaw LJ, Marwick TH, Zoghbi WA, et al. Why all the focus on cardiac imaging? J Am Coll Cardiol Img. 2010;3:789–94.
Fazel R, Gerber TC, Balter S, et al. Approaches to enhancing radiation safety in cardiovascular imaging: a scientific statement from the American Heart Association. Circulation. 2014;130(19):1730–48. Recommendations from a scientific society, the American Heart Association, to limit radiation exposure from cardiovascular imaging modalities employing ionizing radiation.
Farrell MB, Tilkemeier P, S Jerome, Shaw L. Recommended vs observed radiation doses for myocardial perfusion imaging: results from the intersocietal accreditation commissiondatabase. J Nucl Cardiol. 2014;21 (4):799 (Abstr). A comparison “on the field” between recommended and tracer activity effectively administered to patients undergoing MPI.
Einstein AJ, Pascual TN, Mercuri M, et al. INCAPS Investigators Group. Current worldwide nuclear cardiology practices and radiation exposure: results from the 65 country IAEA Nuclear Cardiology Protocols Cross-Sectional Study (INCAPS). Eur Heart J. 2015;36(26):1689–96. A multicenter worldwide survey on the practice of nuclear cardiology, including an assessment of the tracer activity administered. Only 30 % of the laboratories achieved the goal of ≤9 mSv.
ICRP. Radiation dose to patients from radiopharmaceuticals - addendum 3 to ICRP Publication 53. ICRP Publication 106. Ann ICRP. 2008;38(1-2):1–197.
Andersson M, Johansson L, Minarik D, Leide-Svegborn S, Mattsson S. Effective dose to adult patients from 338 radiopharmaceuticals estimated using ICRP biokinetic data, ICRP/ICRU computational reference phantoms and ICRP 2007 tissue weighting factors. EJNMMI Phys. 2014;1(1):9. New data on the effective dose from a lot of tracer, including those used in MPI, that significantly reduce the estimated effective dose from the commonly used MPI protocols.
Verberne HJ, Acampa W, Anagnostopoulos C, et al. EANM procedural guidelines for radionuclide myocardial perfusion imaging with SPECT and SPECT/CT: 2015 revision. Eur J Nucl Med Mol Imaging. 2015;42:1929–40. doi:10.1007/s00259-015-3139-x. The new procedural guidelines from the European Association of Nuclear Medicine significantly reduce the tracer activity recommended for MPI in comparison to the previous ones.
Einstein AJ, Johnson LL, Bokhari S, et al. Agreement of visual estimation of coronary artery calcium from low-dose CT attenuation correction scans in Hybrid PET/CT and SPECT/CT with standard Agatston score. J Am Coll Cardiol. 2010;56:1914–21.
Russell Jr RO, Sutton MG, Udelson JE, et al. ACC/AHA/ASNC guidelines for the clinical use of cardiac radionuclide imaging. J Am Coll Cardiol. 2003;108:1404–18.
Gibbons RJ, Miller TD, Hodge D, et al. Application of appropriateness criteria to stress single-photon emission computed tomography sestamibi studies and stress echocardiograms in an academic medical center. J Am Coll Cardiol. 2008;51:1283–9.
Hendel RC, Cerqueira M, Douglas PS, et al. A multicenter assessment of the use of single-photon emission computed tomography myocardial perfusion imaging with appropriateness criteria. J Am Coll Cardiol. 2010;55:156–62.
Gibbons RJ, Askew JW, Hodge D, Kaping B, Carryer DJ, Miller T. Appropriate use criteria for stress single-photon emission computed tomography sestamibi studies a quality improvement project. Circulation. 2011;123:499–503.
Gholamrezanezhad A, Shirafkan A, Mirpour S, et al. Appropriateness of referrals for single-photon emission computed tomography myocardial perfusion imaging (SPECT-MPI) in a developing community: a comparison between 2005 and 2009 versions of ACCF/ASNC appropriateness criteria. J Nucl Cardiol. 2011;18:1044–52.
Moralidis E, Papadimitriou N, Stathaki M, et al. A multicenter evaluation of the appropriate use of single-photon emission tomography myocardial perfusion imaging in Greece. J Nucl Cardiol. 2013;20:275–83.
Medolago G, Marcassa C, Alkraisheh A, Campini R, Ghilardi A, Giubbini R. Applicability of the appropriateness use criteria for SPECT myocardial perfusion imaging in Italy. Preliminary results. Eur J Nucl Med Mol Imaging. 2014;41:1695–700. A multicenter report on another experience outside USA, that confirms the relationship between the referring physician specialty and the AUC implementation.
Mehta R, Ward RP, Chandra S, Agarwal R, Williams KA. Evaluation of the American College of Cardiology Foundation/American Society of Nuclear Cardiology appropriateness criteria for SPECT myocardial perfusion imaging. J Nucl Cardiol. 2008;15:337–44.
Druz RS, Phillips LM, Sharifova G. Clinical evaluation of the appropriateness use criteria for single-photon emission-computed tomography: differences by patient population, physician specialty, and patient outcomes. ISRN Cardiol. 2011;2011. doi:10.5402/2011/798318
Nelson KH, Willens HJ, Hendel RC. Utilization of radionuclide myocardial perfusion imaging in two health care systems: assessment with the 2009 ACCF/ASNC/AHA appropriateness use criteria. J Nucl Cardiol. 2012;19(1):37–42.
Saifi S, Taylor AJ, Allen J, Hendel R. The use of a learning community and online evaluation of utilization for SPECT myocardial perfusion imaging. J Am Coll Cardiol Imaging. 2013;6:823–9.
Chinnaiyan KM, Peyser P, Goraya T. Impact of a continuous quality improvement initiative on appropriate use of coronary computed tomography angiography. Results from a multicenter, statewide registry, the Advanced Cardiovascular Imaging Consortium. J Am Coll Cardiol. 2012;60:1185–91.
Fraser AG, Buser PT, Bax JJ, et al. The future of cardiovascular imaging and non-invasive diagnosis: a joint statement from the European Association of Echocardiography, the Working Groups on Cardiovascular Magnetic Resonance, Computers in Cardiology, and Nuclear Cardiology, of the European Society of Cardiology, the European Association of Nuclear Medicine, and the Association for European Paediatric Cardiology. Eur Heart J. 2006;27(14):1750–3.
Windecker S, Kolh P, Alfonso F, et al. 2014 ESC/EACTS Guidelines on myocardial revascularization. Eur Heart J. 2014;35:2541–619. This Guidelines provide a summary of the appropriateness of different imaging modalities in the context of CAD diagnosis.
Iskandrian AS, Segal BL. Value of exercise thallium-201 imaging in patients with diagnostic and non diagnostic exercise electrocardiograms. Am J Cardiol. 1981;48(2):233–8.
Manganelli F, Spadafora M, Varrella P, et al. Addition of atropine to submaximal exercise stress testing in patients evaluated for suspected ischaemia with SPECT imaging: a randomized, placebo-controlled trial. Eur J Nucl Med Mol Imaging. 2011;38(2):245–51.
Ross MI, Wu E, Wilkins JT, et al. Safety and feasibility of adjunctive regadenoson injection at peak exercise during exercise myocardial perfusion imaging: the Both Exercise and Regadenoson Stress Test (BERST) trial. J Nucl Cardiol. 2013;20(2):197–204.
Einstein AJ, Johnson LL, DeLuca AJ, et al. Radiation dose and prognosis of ultra-low-dose stress-first myocardial perfusion SPECT in patients with chest pain using a high-efficiency camera. J Nucl Med. 2015;56(4):545–51.
Duvall WL, Baber U, Levine EJ, Croft LB, Henzlova MJ. A model for the prediction of a successful stress-first Tc-99m SPECT MPI. J Nucl Cardiol. 2012;19:1124–34.
Chang SM, Nabi F, Xu J, Raza U, Mahmarian JJ. Normal stress-only versus standard stress/rest myocardial perfusion imaging: similar patient mortality with reduced radiation exposure. J Am Coll Cardiol. 2010;55:221–30.
Ferreira MJ, Cunha MJ, Albuquerque A, et al. Prognosis of normal stress-only gated-SPECT myocardial perfusion imaging: a single center study. Int J Cardiovasc Imaging. 2013;29:1639–44.
Gemignani AS, Muhlebach SG, Abbott BG, Roye GD, Harrington DT, Arrighi JA. Stress-only or stress/rest myocardial perfusion imaging in patients undergoing evaluation for bariatric surgery. J Nucl Cardiol. 2011;18:886–92.
Gibson PB, Demus D, Noto R, Hudson W, Johnson LL. Low event rate for stress- only perfusion imaging in patients evaluated for chest pain. J Am Coll Cardiol. 2002;39:999–1004.
Duvall WL, Guma KA, Kamen J, et al. Reduction in occupational and patient radiation exposure from myocardial perfusion imaging: impact of stress-only imaging and high-efficiency SPECT camera technology. J Nucl Med. 2013;54:1251–7.
Heller GV, Bateman TM, Johnson LL, et al. Clinical value of attenuation correction in stress-only Tc-99m sestamibi SPECT imaging. J Nucl Cardiol. 2004;11:273–81.
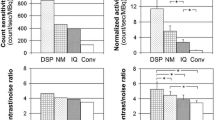
Zoccarato O, Scabbio C, De Ponti E, et al. Comparative analysis of iterative reconstruction algorithms with resolution recovery for cardiac SPECT studies. A multi-center phantom study. J Nucl Cardiol. 2014;21(1):135–48. In this experimental study employing an anthropomorphic phantom, a comparison among the different commercial software solutions allowing for low-counts studies, is described. Moreover, a comparison among the different hardware/software combinations is also reported.
Ahlman MA, Nietert PJ, Wahlquist AE, et al. A single CT for attenuation correction of both rest and stress SPECT myocardial perfusion imaging: a retrospective feasibility study. Int J Clin Exp Med. 2014;7(1):148–55. A feasibility study on the possibility to use a single CT scan for both stress and rest attenuation correction. This would skip the second CT scan, with a reduction in patients’ exposure.
Vija AH, Hawman EG, Engdahl JC. Analysis of a SPECT OSEM reconstruction method with 3D beam modeling and optional attenuation correction: Phantom studies. Nucl Sci Symp Conf Rec. 2003;4:2662–6.
Zoccarato O, Campini R, Marcassa C, Calza P. Performance of a new iterative reconstruction algorithm for cardiac short-time SPECT: preliminary results in an antropomorphic cardiac phantom study. Comput Cardiol. 2008;35:329–32.
DePuey EG, Bommireddipalli S, Clark J, Thompson L, Srour Y. Wide beam reconstruction “quarter-time” gated myocardial perfusion SPECT functional imaging: a comparison to “full-time” ordered subset expectation maximum. J Nucl Cardiol. 2009;16:736–52.
Marcassa C, Campini R, Zoccarato O, Calza P. Wide beam reconstruction for half-dose or half-time cardiac gated-SPECT acquisitions. optimization of resources and reduction in radiation exposure. Eur J Nucl Med Mol Imaging. 2011;38:499–508.
Venero CV, Heller GV, Bateman TM, et al. A multicenter evaluation of a new post-processing method with depth-dependent collimator resolution applied to fulltime and half-time acquisitions without and with simultaneously acquired attenuation correction. J Nucl Cardiol. 2009;16:714–25.
De Lorenzo A, Fonseca LM, Landesmann MC, Lima RS. Comparison between short-acquisition myocardial perfusion SPECT reconstructed with a new algorithm and conventional acquisition with filtered backprojection processing. Nucl Med Commun. 2010;31:552–7.
Imbert L, Marie PY. CZT cameras: a technological jump for myocardial perfusion SPECT. J Nucl Cardiol. 2015. doi:10.1007/s12350-015-0216-2. A comment of the impact of the new cameras architecture (CTZ and confocal collimators) on fast track or low dose protocols, with the possibilities, in theory, to allow for an estimation of the perfusion reserve.
Oddstig J, Hedeer F, Jögi J, Carlsson M, Hindorf C, Engblom H. Reduced administered activity, reduced acquisition time, and preserved image quality for the new CZT camera. J Nucl Cardiol. 2013;20(1):38–44.
van Dijk JD, Jager PL, Ottervanger JP, et al. Minimizing patient-specific tracer dose in myocardial perfusion imaging using CZT SPECT. J Nucl Med Technol. 2015;43(1):36–40.
Sharir T, Pinskiy M, Pardes A, et al. Comparison of the diagnostic accuracies of very low stress-dose with standard-dose myocardial perfusion imaging: automated quantification of one-day, stress-first SPECT using a CZT camera. J Nucl Cardiol. 2015. doi:10.1007/s12350-015-0130-7.
Gunalp B. Role of cardiac ultrafast cameras with CZT solid-state detectors and software developments on radiation absorbed dose reduction to the patients. Radiat Prot Dosim. 2015;165(1-4):461–3. A review summarizing the impact of new CZT detectors and new software reconstruction algorithms on reducing patients’ dose.
Perrin M, Djaballah W, Moulin F, et al. Stress-first protocol for myocardial perfusion SPECT imaging with semiconductor cameras: high diagnostic performances with significant reduction in patient radiation doses. Eur J Nucl Med Mol Imaging. 2015;42(7):1004–11.
Caobelli F, Kaiser SR, Thackeray JT, et al. IQ SPECT allows a significant reduction in administered dose and acquisition time for myocardial perfusion imaging: evidence from a phantom study. J Nucl Med. 2014;55:2064–70. A first study assessing the efficacy of a particular collimators design in increasing camera’s efficiency, thus allowing short time or low dose studies.
Caobelli F, Thackeray JT, Soffientini A, Bengel FM, Pizzocaro C, Guerra UP. Feasibility of one-eighth time gated myocardial perfusion SPECT functional imaging using IQ-SPECT. Eur J Nucl Med Mol Imaging. 2015. doi:10.1007/s00259-015-3142-2. An extreme estimation on how “as short as possible” SPECT acquisition time could be, with the use of new confocal collimators.
Marcassa C, Zoccarato O, Campini R, Calza P. Temporal evolution of administered activity in cardiac gated-SPECT and patients’ effective dose. Analysis of an historical series. Eur J Nucl Med Mol Imaging. 2013;40:325–30. A single center report on the effect of different tracer activities (according to Recommendations, a weight-based approach, and a low-dose approach) on patients’ and operators’ exposure.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of Interest
Claudio Marcassa and Orazio Zoccarato declare that they have no conflicts of interest.
Human and Animal Rights and Informed Consent
All studies by the authors that are cited in references and involve human subjects were performed after approval by the appropriate institutional review boards. When required, written informed consent was obtained from all participants.
Additional information
This article is part of the Topical Collection on Cardiac Nuclear Imaging
Rights and permissions
About this article
Cite this article
Marcassa, C., Zoccarato, O. Radiation Dose Reduction from Radionuclide Myocardial Perfusion Imaging. Curr Cardiovasc Imaging Rep 9, 4 (2016). https://doi.org/10.1007/s12410-015-9364-7
Published:
DOI: https://doi.org/10.1007/s12410-015-9364-7