Abstract
Individuals with attention-deficit/hyperactivity disorder (ADHD) show pervasive impairments across family, peer, and school or work functioning that may extend throughout the day. Psychostimulants are highly effective medications for the treatment of ADHD, and the development of long-acting stimulant formulations has greatly expanded the treatment options for individuals with ADHD. Strategies for the formulation of long-acting stimulants include the combination of immediate-release and delayed-release beads, and an osmotic-release oral system. A recent development is the availability of the first prodrug stimulant, lisdexamfetamine dimesylate (LDX). LDX itself is inactive but is cleaved enzymatically, primarily in the bloodstream, to release d-amphetamine (d-AMP). Several clinical trials have demonstrated that long-acting stimulants are effective in reducing ADHD symptoms compared with placebo. Analog classroom and simulated adult workplace environment studies have shown that long-acting stimulants produce symptom reduction for at least 12 h. Long-acting stimulants exhibit similar tolerability and safety profiles to short-acting equivalents. While variations in gastric pH and motility can alter the availability and absorption of stimulants released from long-acting formulations, the systemic exposure to d-AMP following LDX administration is unlikely to be affected by gastrointestinal conditions. Long-acting formulations may also improve adherence and lower abuse potential compared with their short-acting counterparts. The development of long-acting stimulants provides physicians with an increased range of medication options to help tailor treatment for individuals with ADHD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Attention-deficit/hyperactivity disorder (ADHD) is a common neurobehavioral disorder that is estimated to affect 5–12 % of children and persists into adulthood in more than half of cases (Biederman and Faraone 2005; Polanczyk et al. 2007). ADHD is characterized by the core symptoms of inattention, hyperactivity, and impulsivity (American Psychiatric Association 2000). In addition, individuals with ADHD exhibit functional impairments that include poor intrafamily interactions, low academic achievement and conduct problems in children and adolescents, and increased risk of lower educational attainment, behavior leading to arrests and traffic violations, unemployment, and divorce in adults (Able et al. 2007; Barkley et al. 2006; Biederman et al. 2006a; Kessler et al. 2006; Klassen et al. 2004; Sawyer et al. 2002).
Clinical guidelines for the treatment for ADHD generally recommend an individualized, multimodal plan which includes pharmacotherapy, behavioral, and educational interventions (American Academy of Pediatrics 2011; Canadian Attention Deficit Hyperactivity Disorder Resource Alliance (CADDRA) 2011; National Institute for Health and Clinical Excellence 2009; Pliszka 2007). For many years, short-acting formulations of the psychostimulants methylphenidate (MPH) and amphetamine (AMP) were the mainstay of ADHD pharmacotherapy. However, despite their well-documented efficacy, durations of action in the range 3–6 h posed significant challenges and limitations in their treatment for ADHD (Antshel et al. 2011). The requirement for repeated dosing during the day may cause embarrassment and stigma for the patient, difficulties associated with storing scheduled drugs, especially in a school environment, fragmented coverage, poor adherence, and the potential for the diversion of drug for non-medical use (Swanson 2003; Wolraich et al. 2001). In response to these challenges, long-acting psychostimulants were developed to relieve ADHD symptoms throughout the day without the need for repeat dosing and to improve adherence compared with short-acting agents (Adler and Nierenberg 2010; Christensen et al. 2010; Ramos-Quiroga et al. 2008; Spencer et al. 2011; van den Ban et al. 2010).
The variation in the pharmacokinetic properties of the different formulations of long-acting psychostimulant therapies is reflected in their pharmacodynamic properties including their onset, magnitude, and duration of symptom relief. Treatment strategies should be based on an understanding of the efficacy and safety profile of each formulation, paired with individual patient needs. Long-acting psychostimulants, as well as the non-stimulant atomoxetine, are recommended as first-line pharmacotherapies in many countries for the management of ADHD in children, adolescents, and adults (American Academy of Pediatrics 2011; Canadian Attention Deficit Hyperactivity Disorder Resource Alliance (CADDRA) 2011; National Institute for Health and Clinical Excellence 2009; Pliszka 2007). This article will review the different controlled-release and prodrug delivery systems of long-acting stimulants, and examine the impact of these formulations on their pharmacokinetics, efficacy, safety, and adherence.
Long-acting stimulant formulations
The long-acting psychostimulants that have been approved for the treatment for ADHD can be categorized according to the technology that has been utilized to extend or delay the release of the active agent (Fig. 1) (Table 1). The first generation of long-acting stimulants included sustained-release formulations of MPH (MPH-SR) that utilized a wax-matrix-based technology to deliver a single, prolonged pulse of MPH. With a duration of action of up to 8 h, some authors consider these preparations to be intermediate- rather than long-acting (Dopheide 2009), and their efficacy may be inferior to multiple-dose regimens of the immediate-release formulations (Swanson and Volkow 2009). The flat (zero-order) drug delivery profile of MPH-SR may account for the development of acute drug tolerance in response to exposure to relatively high drug levels over a prolonged period (Swanson 2003).
Delivery systems of long-acting psychostimulants used in the treatment for ADHD. Not shown are the delivery systems of MPH-SR and Novo-MPH ER-C. MPH-SR is an extended-release formulation in tablet form that uses a wax-based matrix to achieve prolonged release (Ermer et al. 2010b). The delivery mechanism of Novo-MPH ER-C has not been published (Canadian Attention Deficit Hyperactivity Disorder Resource Alliance (CADDRA)). CR controlled-release, d-AMP d-amphetamine, LDX lisdexamfetamine dimesylate, MAS mixed amphetamine salts, MPH methylphenidate, SR sustained-release, XR extended-release
Several controlled-release (CR) stimulant formulations were developed that combined a rapid onset of action with extended coverage throughout the day. One strategy for the biphasic delivery of stimulants is to mix beads with different drug release profiles. CR capsules contain beads that incorporate MPH (MPH-CR) or d-AMP (AMP-CR) with distinct immediate- and delayed-release profiles (Fig. 1). CR-mixed AMP salts comprise equal proportions of four AMP salts, d-AMP saccharate, d,l-AMP aspartate monohydrate, d-AMP sulfate, and d,l-AMP sulfate. Each capsule contains immediate-release and enteric-coated delayed-release beads in a 1:1 ratio (Shire Canada Inc.; Tulloch et al. 2002). Several stimulant drugs are based on combinations of beads with immediate- and extended-release profiles, but the proportions of the total dose of active ingredient in the two phases of delivery vary.
An alternative technology designed to deliver the controlled and biphasic delivery of stimulant medication is the osmotic-release oral system methylphenidate (OROS-MPH). OROS-MPH utilizes osmotic pressure to control the rate of delivery of the active ingredient, racemic MPH. Each capsule consists of a three-compartment core that is enclosed by a semipermeable membrane that, in turn, is surrounded by a drug overcoat (Fig. 1). After ingestion, the drug overcoat provides immediate release of MPH (22 % of the dose) (McBurnett and Starr 2011). Aqueous fluid enters the osmotic pump compartment from the gastrointestinal tract and delivers the remaining dose at a first-order rate from the core through a laser-drilled exit port (Janssen Inc.; Swanson et al. 2004). A concentration gradient exists between the two drug compartments, which also modifies the rate of drug release. OROS-MPH has a smooth ascending plasma concentration profile, which is thought to minimize the development of acute tolerance and maintain full efficacy across the day (Swanson et al. 2003).
Lisdexamfetamine dimesylate (LDX) is the first prodrug stimulant. Rather than utilizing a mechanical or physical mechanism to achieve a prolonged duration of action, LDX is a prodrug in which d-AMP is covalently bound to the amino acid lysine. LDX itself is therapeutically inactive but, after oral administration, enzymatic hydrolysis of LDX releases the therapeutically active moiety d-AMP (Pennick 2010). The rate of enzymatic conversion controls the rate at which d-AMP becomes available. The resulting pharmacokinetic profile is dose-proportional and monophasic and reflects the gradual conversion of LDX to d-AMP over the post-dose period (Boellner et al. 2010). As enzymatic hydrolysis occurs mostly in the bloodstream (Pennick 2010), the metabolic conversion of LDX to d-AMP is unlikely to be affected by variations in gastric pH or gastrointestinal transit time (Ermer et al. 2010b; Haffey et al. 2009; Krishnan and Zhang 2008). Thus, pharmacokinetic studies have shown that the rate of d-AMP absorption and metabolism is more consistent and predictable between and within individuals with LDX than with extended-release mixed amphetamine salts (MAS-XR) (Biederman et al. 2007a; Ermer et al. 2010a). Furthermore, the rate of d-AMP delivery following administration of LDX is reported to be unaffected by concurrent administration of the acid-suppressing drug omeprazole, whereas a shortened time to peak concentration of d-AMP was observed when MAS-XR was taken with omeprazole (Haffey et al. 2009) (Table 1).
Efficacy of long-acting stimulants
Clinical trial evidence supports the efficacy of long-acting stimulants. Tables 2 and 3 present a summary of short-term (≤13-weeks), randomized, controlled clinical efficacy trials of long-acting psychostimulants. The control of symptoms throughout the day and into the early evening is likely to be an important factor in the overall efficacy of ADHD pharmacotherapies (Coghill et al. 2008).
Methylphenidate sustained-release
There are limited clinical trial data of MPH-SR in children with ADHD (Table 2). In a comparison of immediate-release MPH (MPH-IR), with MPH-SR, controlled-release d-AMP, and pemoline in boys with ADHD, sustained-release MPH demonstrated efficacy versus placebo in some behavioral measures, some performance-based tasks, and structured assessments by counselors on the Abbreviated Conners’ Teachers Rating Scale (ACTRS), but not on the teacher-rated ACTRS (Pelham et al. 1990). MPH-SR has a duration of effect of approximately 8 h (Novartis Pharmaceuticals Canada Inc.).
Methylphenidate controlled-release
MPH-CR has shown significant efficacy in reducing ADHD symptoms (Table 2). In children with ADHD, both MPH-CR and IR-MPH yielded similar, statistically significant reductions from baseline in Conners’ Parent Rating Scale-Revised scores (CPRS-R)(Weiss et al. 2007). However, superior symptom reduction with IR-MPH versus MPH-CR was observed based on Conners’ Teacher Rating Scale-Revised (CTRS-R). In adults with ADHD, MPH-CR yielded significantly better Clinical Global Impressions-Improvement (CGI-I) ratings versus placebo after 2 weeks (Jain et al. 2007). Using an analog classroom crossover protocol, Schachar et al. (2008) compared MPH-CR and IR-MPH with placebo in children with ADHD. Significant improvements versus placebo were seen with MPH-CR for up to 10 h post-dosing, based on change from baseline on Inattention/Overactivity With Aggression-Conners’ scale (IOWA-C) overall and subscores for inattention/overactivity and aggression/defiance.
Osmotic-release oral system methylphenidate
OROS-MPH has demonstrated efficacy in ADHD symptom reduction in children, adolescents, and adults (Table 2). In a 4-week, parallel-group, placebo-controlled study, OROS-MPH was significantly more effective than placebo in children with ADHD, based on endpoint scores for the Inattention/Overactivity subscale of the IOWA Conners’ Teacher Rating Scale (Wolraich et al. 2001). In a 2-week, parallel-group study, OROS-MPH significantly reduced ADHD Rating Scale IV (ADHD-RS-IV) scores in adolescents with ADHD compared with placebo (Wilens et al. 2006a). Similar improvements compared with placebo in the symptoms of ADHD have been described in adults treated with OROS-MPH (Adler et al. 2009; Biederman et al. 2006b; Medori et al. 2008).
In a head-to-head trial, subtle variations of timing and magnitude of symptom control were observed between MPH-CD and OROS-MPH. Although MPH-CD showed greater efficacy in the morning hours, OROS-MPH exhibited longer-lasting efficacy, extending up to 12 h following a single morning dose (Pelham et al. 2001). Head-to-head comparisons of long-acting MPH (MPH-LA) and OROS-MPH in children with ADHD using analog classroom protocols over 8–12 h found that both active treatments improved Permanent Product Measure of Performance (PERMP) math test scores for the number of problems answered correctly (PERMP-C) (Lopez et al. 2003) and Swanson, Kotkin, Agler, M-Flynn, and Pelham Rating Scale (SKAMP)-deportment and SKAMP-Attention scores (Silva et al. 2005). While both treatments were generally effective and well tolerated, superiority of one treatment over the other in such laboratory school settings is dependent on the formulation with the highest expected plasma MPH concentration across the post-dosing period (Swanson et al. 2004). Placebo-controlled analog classroom studies indicate that OROS-MPH has a duration of action of at least 12.5 h (the last time point assessed) in children with ADHD (Armstrong et al. 2012; Murray et al. 2011; Wigal et al. 2011).
Mixed amphetamine salts extended-release
A number of randomized controlled clinical trials have shown that controlled-release MAS (MAS-CR) is effective versus placebo for reducing ADHD symptoms in children, adolescents, and adults (Table 3) (Biederman et al. 2002; Spencer et al. 2006b; Weisler et al. 2006). An analog classroom trial in children showed that a significant effect of MAS-CR over placebo emerged at 1.5 h post-dosing and was maintained for up to 12 h, based on improvements from baseline at end point in SKAMP-D and math test scores (McCracken et al. 2003).
Dextroamphetamine controlled-release
Studies of the efficacy of controlled-release AMP (AMP-CR) in participants with ADHD are limited. Pelham et al. compared treatment arms with AMP-CR, IR-MPH, MPH-SR, and pemoline in boys. Although all treatments were superior to placebo in some behavioral measures, only pemoline and AMP-XR were superior to placebo by the teacher-rated ACTRS. The duration of efficacy was characterized as within 2 h of ingestion and up to 9 h post-dose (Pelham et al. 1990). In an analog classroom trial of AMP-CR in children, objective actometer measures and parent ratings of behavior were improved compared with placebo from 1.75 to 12 h following a single morning dose. The effects of AMP-CR were “less robust” than those of IR-MAS in the morning hours after dosing but were extended for 3–6 h longer (James et al. 2001).
Lisdexamfetamine dimesylate
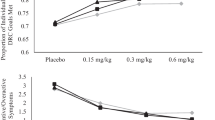
The efficacy of LDX compared with placebo in reducing the symptoms of ADHD has been demonstrated in patients across the lifespan (Table 3). In 4-week trials of LDX 30, 50, and 70 mg in children, adolescents, and adults with ADHD, all doses of LDX demonstrated significant improvements in ADHD-RS-IV scores compared with placebo (Adler et al. 2008; Biederman et al. 2007b; Findling et al. 2011). Mean rates of response (defined as >30 % improvement in ADHD-RS-IV scores and CGI-I ratings of much improved or very much improved) were approximately 80 % at end point in children treated with LDX 70 mg compared with less than 20 % for placebo (Biederman et al. 2007b). Furthermore, improvements compared to placebo in CPRS-R scores in children with ADHD were maintained until 6 pm following an early morning dose (Biederman et al. 2007b). In an analog classroom study in children with ADHD, the therapeutic effects of LDX extended from 1.5 to 13 h post-dose (the first and last time points assessed) based on improvements in SKAMP and PERMP scores (Wigal et al. 2009). In a simulated adult workplace environment study, the therapeutic effects of LDX were maintained from 2 to 14 h post-dose (the first and last time points measured) in adults with ADHD, as shown by improvements in PERMP scores versus placebo (Wigal et al. 2010). The demonstration that the efficacy of LDX is maintained for at least 13 h in children and 14 h in adults suggests that this prodrug may be the longest-acting stimulant treatment for ADHD.
Meta-analyses of the effectiveness of long-acting stimulants
Meta-analyses have compared efficacy outcomes from multiple studies of different stimulant formulations (Faraone 2009, 2012; Faraone and Glatt 2010). In an analysis of 32 trials of 16 medications in youths with ADHD, the mean effect size for long-acting stimulants was 0.95 compared with 0.99 for immediate-release stimulants (Faraone 2009). Similarly, in 19 trials of 13 ADHD drugs in adults, mean effect sizes were 0.73 and 0.96 for long-acting and immediate-release stimulants, respectively (Faraone and Glatt 2010). A meta-analysis of efficacy studies in children with ADHD, based only on ADHD Rating Scale and Clinical Global Impressions outcomes, found that a pooled effect size for LDX of approximately 1.5 was significantly (p < 0.001) greater than the pooled effect size of the other medications (Faraone 2012). In adult studies, LDX effect sizes were similar to those of other medications. Using numbers-needed-to-treat (NNT) to compare the efficacy of stimulants medications across 23 clinical trials in children and adolescents, NNT (95 % confidence intervals) were slightly lower (i.e., fewer patients were required to see a positive effect) for formulations of AMP (2.0 [1.7, 2.2]) than MPH (2.6 [2.4, 2.8]), although mean NNT values were not calculated for long-acting and immediate-release formulations (Faraone et al. 2006).
Safety of psychostimulants
Short- and long-acting psychostimulants share similar adverse event profiles (Banaschewski et al. 2006). Adverse events most commonly associated with the use of psychostimulants to treat ADHD include neurological (headache, dizziness, insomnia, seizures), psychiatric (mood/anxiety, tics, psychosis), and gastrointestinal (abdominal pain, poor appetite leading to weight loss/slowed growth) effects. In general, these events are mild and/or temporary (Graham et al. 2011). Areas of particular concern in the use of psychostimulants to treat ADHD include their effects on growth and cardiovascular parameters, and their potential for abuse.
Effect on weight and growth
An analysis of 20 longitudinal studies found that long-term psychostimulant use in children with ADHD resulted in statistically significant delays in growth versus age-related norms (Faraone et al. 2008). Effects appeared to be dose-related, were more apparent for weight than height, were similar between MPH and AMP formulations, and, in many cases, appeared to normalize over time despite continued treatment (Faraone et al. 2008). In the MTA (Multimodal Treatment Study of Children with ADHD), the largest longitudinal study of children with ADHD, average relative size of patient (a composite of height and weight as z scores) was negatively related to the average cumulative exposure to psychostimulants. Growth slowing for newly medicated versus untreated participants was found for the first 14 months, was attenuated at 24 months, and was non-significant at 36 months (Murray et al. 2008; Swanson et al. 2007). Nevertheless, it is recommended that height and weight are monitored in patients receiving stimulant medications, including long-acting formulations.
Cardiovascular events
Cardiovascular safety concerns with psychostimulant ADHD medications were raised based on rare occurrences of sudden death and other cardiac events (Vetter et al. 2008). Psychostimulants modulate cardiovascular contractility and heart rate via sympathomimetic effects (Wilens et al. 2006b), and changes in vital signs have been noted with MPH and AMP treatments, including increases in systolic and diastolic blood pressure (~2–6 mmHg) and heart rate (~8 beats per minute) (Wilens et al. 2005). In clinical trials of psychostimulants in children and adults, no clinically significant changes in atrial or ventricular conduction or repolarization have been observed (Wilens et al. 2006b). An elevated risk of cardiac-related emergency visits with current psychostimulant use versus non-use has been reported (Winterstein et al. 2007; Winterstein et al. 2009), but in the majority of healthy children with no history of or current cardiovascular abnormalities, psychostimulants produced cardiovascular effects of minimal clinical significance (Findling et al. 2001, 2005; Safer 1992; Wilens et al. 2006b). Similarly, a large, retrospective, population-based cohort study concluded that ADHD medication use in children and young and middle-aged adults was not associated with an increased risk of serious cardiovascular events compared with non-use (Cooper et al. 2011; Habel et al. 2011). However, when treatment with any psychostimulant formulation is contemplated in a patient with structural heart disease, or in a patient who has a personal or a family history of syncope or sudden death, respectively, a pediatric or cardiologic consultation prior to ADHD pharmacological treatment is strongly advised (Graham et al. 2011).
Abuse, misuse, and diversion
Prescription stimulants are classified as controlled substances, and their abuse, misuse, and diversion are important public health and safety concerns (Kollins 2008; Wilens et al. 2008). Since euphoria and drug “liking” are linked to a more rapid rate of absorption and delivery to the brain (Volkow and Swanson 2003), it follows that controlling the rate of stimulant release may modify its potential for abuse. Support for a lower abuse potential for long-acting compared with short-acting stimulants includes greater subjective responses for immediate-release stimulants than OROS-MPH in healthy adults (Parasrampuria et al. 2007; Spencer et al. 2006a). The formulation of stimulants as once-daily medications also reduces the likelihood of diversion by removing the requirement for drug administration at school.
Many long-acting stimulants can be manipulated to facilitate more rapid absorption of the active ingredient, for example by crushing or dissolving the medications in order to facilitate intranasal or parenteral administration (Mao et al. 2011). However, the physical characteristics of stimulant formulations, such as the non-deformable shell of the OROS-MPH capsule, may make them more difficult to break, cut, or crush. The prodrug design of LDX means that the rate of active d-AMP release is limited by the rate of enzymatic conversion, regardless of the route of drug administration or capsule intactness. Thus, the plasma concentration–time profile of intranasal LDX in healthy men is similar to that following oral administration (Ermer et al. 2011). In individuals with a history of stimulant abuse, scores in the Drug Rating Questionnaire-Subject liking scale for oral LDX (≤100 mg) were no different to placebo, whereas the equivalent oral dose of d-AMP (40 mg) was favored over placebo (Jasinski and Krishnan 2009a). Similarly, unlike intravenous d-AMP 20 mg, an equivalent intravenous dose of LDX (50 mg) did not produce subjective abuse-related liking scores (Jasinski and Krishnan 2009a, b).
Adherence
Non-adherence to medication for chronic illnesses is estimated to be approximately 50 % (World Health Organization 2003). In ADHD, the prevalence of medication discontinuation or non-adherence is reported to range from 13 to 64 % (Adler and Nierenberg 2010). After 14 months of treatment with MPH in the MTA study, analysis of saliva samples indicated that only 53.5 % of patients were adherent at every assay point and that almost 25 % of patients were non-adherent at 50 % or more of their assays (Pappadopulos et al. 2009). Studies that have examined the impact of formulation on adherence and persistence of stimulant medications for ADHD include several retrospective claims analyses (Christensen et al. 2010; Marcus et al. 2005; Sanchez et al. 2005). The largest of these identified over 60,000 newly treated patients with ADHD (Christensen et al. 2010). This analysis indicated that the mean (SD) adherence (defined as the ratio of the number of days therapy supplied to the total number of days persistent) to long-acting stimulants (0.56 [0.32]) was significantly greater (p < 0.0001) than that for short- (0.43 [0.35]) and intermediate-acting (0.47 [0.35]) stimulants. Similarly, the mean (SD) persistence (defined as the number of days out of 365 days plus the index day that the patient remained on their index therapy) on long-acting stimulants (239.5 [145.8]) was significantly greater (p < 0.0001) than for short- (186.7 [154.8]) or intermediate-acting (185.6 [153.4]) stimulants (Christensen et al. 2010). Furthermore, a chart review of Spanish adults with ADHD found that the switch from short-acting MPH to long-acting MPH was associated with a significant improvement in all items of the Simplified Medication Adherence Questionnaire (Ramos-Quiroga et al. 2008). These data suggest that the choice of formulation has important consequences on the adherence and persistence of ADHD stimulant medications.
Treatment individualization
Evidence-based ADHD guidelines recognize that medication strategies should be tailored for the individual. Among the factors to consider when selecting an appropriate medication for a patient with ADHD are drug class and the formulation required to give the desired pharmacokinetic and pharmacodynamic profiles. The choice of medications for ADHD includes both stimulants and non-stimulants. With regard to stimulants, although mean responses to MPH and AMP are similar, individuals may respond differently to the two drugs. As reviewed by Arnold (2000), approximately 28 % will respond preferentially to AMP, 17 % will respond preferentially to MPH, and less than 13 % will not respond to either (Arnold 2000). Where stimulant medications are indicated, the selection of formulation should be based both on clinical requirements and on the preferences of the patient and/or their family. Short- and long-acting formulations provide treatment options ranging from approximately 4 h to, in the case of LDX, more than 13 h in children (Wigal et al. 2009) and more than 14 h in adults (Wigal et al. 2010). It is important to note that suboptimal response to one class or formulation of stimulant does not predict failure of another. Thus, a recent post hoc analysis found that the clinical effectiveness and rates of remission in children with ADHD who were treated with LDX were similar in patients with a previous suboptimal response to MPH treatment to those of the overall study population (Jain et al. 2011).
Conclusions
The development of controlled-release formulations of stimulants and the stimulant prodrug LDX has greatly increased the number of pharmacological treatment options for patients with ADHD. At equivalent systemic exposures, the efficacy and safety of long-acting stimulants appear to be equivalent to short-acting formulations. However, long-acting medications offer several potential benefits to patients. Long-acting stimulants offer efficacy for at least 13–14 h without augmentation. The convenience of once-daily dosing may contribute to improved adherence of long-acting stimulants compared with short-acting stimulants. Prodrug technology may also provide lower inter- and intra-patient variability in exposure than mechanical controlled-release systems. Furthermore, long-acting stimulants may be less prone to abuse than their short-acting counterparts. Thus, the development of long-acting formulations of stimulants provides important additional treatment options for the management of ADHD.
References
Able SL, Johnston JA, Adler LA, Swindle RW (2007) Functional and psychosocial impairment in adults with undiagnosed ADHD. Psychol Med 37(1):97–107. doi:10.1017/S0033291706008713
Adler LD, Nierenberg AA (2010) Review of medication adherence in children and adults with ADHD. Postgrad Med 122(1):184–191. doi:10.3810/pgm.2010.01.2112
Adler LA, Goodman DW, Kollins SH, Weisler RH, Krishnan S, Zhang Y, Biederman J (2008) Double-blind, placebo-controlled study of the efficacy and safety of lisdexamfetamine dimesylate in adults with attention-deficit/hyperactivity disorder. J Clin Psychiatry 69(9):1364–1373
Adler LA, Zimmerman B, Starr HL, Silber S, Palumbo J, Orman C, Spencer T (2009) Efficacy and safety of OROS methylphenidate in adults with attention-deficit/hyperactivity disorder: a randomized, placebo-controlled, double-blind, parallel group, dose-escalation study. J Clin Psychopharmacol 29(3):239–247. doi:10.1097/JCP.0b013e3181a390ce
American Academy of Pediatrics (2011) ADHD: clinical Practice Guideline for the diagnosis, evaluation, and treatment of attention-deficit/hyperactivity disorder in children and adolescents. Pediatrics 128:1007–1022
American Psychiatric Association (2000) Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision (DSM-IV-TR). American Psychiatric Association, Washington DC
Antshel KM, Hargrave TM, Simonescu M, Kaul P, Hendricks K, Faraone SV (2011) Advances in understanding and treating ADHD. BMC Med 9:72. doi:10.1186/1741-7015-9-72
Armstrong RB, Damaraju CV, Ascher S, Schwarzman L, O’Neill J, Starr HL (2012) Time course of treatment effect of OROS(R) methylphenidate in children with ADHD. J Atten Disord 16:697–705. doi:10.1177/1087054711425772
Arnold LE (2000) Methylphenidate vs. amphetamine: comparative review. J Atten Disord 3(4):200–211. doi:10.1177/108705470000300403
Banaschewski T, Coghill D, Santosh P, Zuddas A, Asherson P, Buitelaar J, Danckaerts M, Dopfner M, Faraone SV, Rothenberger A, Sergeant J, Steinhausen HC, Sonuga-Barke EJ, Taylor E (2006) Long-acting medications for the hyperkinetic disorders. A systematic review and European treatment guideline. Eur Child Adolesc Psychiatry 15(8):476–495. doi:10.1007/s00787-006-0549-0
Barkley RA, Fischer M, Smallish L, Fletcher K (2006) Young adult outcome of hyperactive children: adaptive functioning in major life activities. J Am Acad Child Adolesc Psychiatry 45(2):192–202. doi:10.1097/01.chi.0000189134.97436.e2
Biederman J, Faraone SV (2005) Attention-deficit hyperactivity disorder. Lancet 366(9481):237–248. doi:10.1016/s0140-6736(05)66915-2
Biederman J, Lopez FA, Boellner SW, Chandler MC (2002) A randomized, double-blind, placebo-controlled, parallel-group study of SLI381 (Adderall XR) in children with attention-deficit/hyperactivity disorder. Pediatrics 110(2 Pt 1):258–266
Biederman J, Faraone SV, Spencer TJ, Mick E, Monuteaux MC, Aleardi M (2006a) Functional impairments in adults with self-reports of diagnosed ADHD: a controlled study of 1001 adults in the community. J Clin Psychiatry 67(4):524–540
Biederman J, Mick E, Surman C, Doyle R, Hammerness P, Harpold T, Dunkel S, Dougherty M, Aleardi M, Spencer T (2006b) A randomized, placebo-controlled trial of OROS methylphenidate in adults with attention-deficit/hyperactivity disorder. Biol Psychiatry 59(9):829–835. doi:10.1016/j.biopsych.2005.09.011
Biederman J, Boellner SW, Childress A, Lopez FA, Krishnan S, Zhang Y (2007a) Lisdexamfetamine dimesylate and mixed amphetamine salts extended-release in children with ADHD: a double-blind, placebo-controlled, crossover analog classroom study. Biol Psychiatry 62(9):970–976. doi:10.1016/j.biopsych.2007.04.015
Biederman J, Krishnan S, Zhang Y, McGough JJ, Findling RL (2007b) Efficacy and tolerability of lisdexamfetamine dimesylate (NRP-104) in children with attention-deficit/hyperactivity disorder: a phase III, multicenter, randomized, double-blind, forced-dose, parallel-group study. Clin Ther 29(3):450–463
Boellner SW, Stark JG, Krishnan S, Zhang Y (2010) Pharmacokinetics of lisdexamfetamine dimesylate and its active metabolite, d-amphetamine, with increasing oral doses of lisdexamfetamine dimesylate in children with attention-deficit/hyperactivity disorder: a single-dose, randomized, open-label, crossover study. Clin Ther 32(2):252–264. doi:10.1016/j.clinthera.2010.02.011
Canadian Attention Deficit Hyperactivity Disorder Resource Alliance (CADDRA) CADDRA response to new ADHD Generic Medication: Novo-Methylphenidate ER-C. June 3, 2010. http://www.caddra.ca/cms4/index.php?option=com_content&view=article&id=181&Itemid=356&lang=en. Accessed March 1, 2012
Canadian Attention Deficit Hyperactivity Disorder Resource Alliance (CADDRA) (2011) Canadian ADHD Practice Guidelines (CAP-Guidelines). http://wwwcaddraca/cms4/pdfs/caddraGuidelines2011pdf. Accessed January 2013
Casas M, Rosler M, Sandra Kooij JJ, Ginsberg Y, Ramos-Quiroga JA, Heger S, Berwaerts J, Dejonckheere J, van der Vorst E, Schauble B (2011) Efficacy and safety of prolonged-release OROS methylphenidate in adults with attention deficit/hyperactivity disorder: a 13-week, randomized, double-blind, placebo-controlled, fixed-dose study. World J Biol Psychiatry. doi:10.3109/15622975.2011.600333
Christensen L, Sasane R, Hodgkins P, Harley C, Tetali S (2010) Pharmacological treatment patterns among patients with attention-deficit/hyperactivity disorder: retrospective claims-based analysis of a managed care population. Curr Med Res Opin 26(4):977–989. doi:10.1185/03007991003673617
Coghill D, Soutullo C, d’Aubuisson C, Preuss U, Lindback T, Silverberg M, Buitelaar J (2008) Impact of attention-deficit/hyperactivity disorder on the patient and family: results from a European survey. Child Adolesc Psychiatry Ment Health 2(1):31. doi:10.1186/1753-2000-2-31
Cooper WO, Habel LA, Sox CM, Chan KA, Arbogast PG, Cheetham TC, Murray KT, Quinn VP, Stein CM, Callahan ST, Fireman BH, Fish FA, Kirshner HS, O’Duffy A, Connell FA, Ray WA (2011) ADHD drugs and serious cardiovascular events in children and young adults. N Engl J Med 365(20):1896–1904. doi:10.1056/NEJMoa1110212
Dopheide JA (2009) The role of pharmacotherapy and managed care pharmacy interventions in the treatment of ADHD. Am J Manag Care 15(5 Suppl):S141–S150
Ermer J, Homolka R, Martin P, Buckwalter M, Purkayastha J, Roesch B (2010a) Lisdexamfetamine dimesylate: linear dose-proportionality, low intersubject and intrasubject variability, and safety in an open-label single-dose pharmacokinetic study in healthy adult volunteers. J Clin Pharmacol 50(9):1001–1010. doi:10.1177/0091270009357346
Ermer JC, Adeyi BA, Pucci ML (2010b) Pharmacokinetic variability of long-acting stimulants in the treatment of children and adults with attention-deficit hyperactivity disorder. CNS Drugs 24(12):1009–1025. doi:10.2165/11539410-000000000-00000
Ermer JC, Dennis K, Haffey MB, Doll WJ, Sandefer EP, Buckwalter M, Page RC, Diehl B, Martin PT (2011) Intranasal versus oral administration of lisdexamfetamine dimesylate: a randomized, open-label, two-period, crossover, single-dose, single-centre pharmacokinetic study in healthy adult men. Clin Drug Investig 31(6):357–370. doi:10.2165/11588190-000000000-00000
Faraone SV (2009) Using Meta-analysis to Compare the Efficacy of Medications for Attention-Deficit/Hyperactivity Disorder in Youths. P T 34(12):678–694
Faraone SV (2012) Understanding the effect size of lisdexamfetamine dimesylate for treating ADHD in children and adults. J Atten Disord 16(2):128–137. doi:10.1177/1087054710379738
Faraone SV, Glatt SJ (2010) A comparison of the efficacy of medications for adult attention-deficit/hyperactivity disorder using meta-analysis of effect sizes. J Clin Psychiatry 71(6):754–763. doi:10.4088/JCP.08m04902pur
Faraone SV, Biederman J, Spencer TJ, Aleardi M (2006) Comparing the efficacy of medications for ADHD using meta-analysis. MedGenMed 8(4):4
Faraone SV, Biederman J, Morley CP, Spencer TJ (2008) Effect of stimulants on height and weight: a review of the literature. J Am Acad Child Adolesc Psychiatry 47(9):994–1009. doi:10.1097/CHI.ObO13e31817eOea7
Findling RL, Short EJ, Manos MJ (2001) Short-term cardiovascular effects of methylphenidate and adderall. J Am Acad Child Adolesc Psychiatry 40(5):525–529. doi:10.1097/00004583-200105000-00011
Findling RL, Biederman J, Wilens TE, Spencer TJ, McGough JJ, Lopez FA, Tulloch SJ (2005) Short- and long-term cardiovascular effects of mixed amphetamine salts extended release in children. J Pediatr 147(3):348–354. doi:10.1016/j.jpeds.2005.03.014
Findling RL, Childress AC, Cutler AJ, Gasior M, Hamdani M, Ferreira-Cornwell MC, Squires L (2011) Efficacy and safety of lisdexamfetamine dimesylate in adolescents with attention-deficit/hyperactivity disorder. J Am Acad Child Adolesc Psychiatry 50(4):395–405. doi:10.1016/j.jaac.2011.01.007
Gonzalez MA, Pentikis HS, Anderl N, Benedict MF, DeCory HH, Dirksen SJ, Hatch SJ (2002) Methylphenidate bioavailability from two extended-release formulations. Int J Clin Pharmacol Ther 40(4):175–184
Graham J, Banaschewski T, Buitelaar J, Coghill D, Danckaerts M, Dittmann RW, Dopfner M, Hamilton R, Hollis C, Holtmann M, Hulpke-Wette M, Lecendreux M, Rosenthal E, Rothenberger A, Santosh P, Sergeant J, Simonoff E, Sonuga-Barke E, Wong IC, Zuddas A, Steinhausen HC, Taylor E (2011) European guidelines on managing adverse effects of medication for ADHD. Eur Child Adolesc Psychiatry 20(1):17–37. doi:10.1007/s00787-010-0140-6
Habel LA, Cooper WO, Sox CM, Chan KA, Fireman BH, Arbogast PG, Cheetham TC, Quinn VP, Dublin S, Boudreau DM, Andrade SE, Pawloski PA, Raebel MA, Smith DH, Achacoso N, Uratsu C, Go AS, Sidney S, Nguyen-Huynh MN, Ray WA, Selby JV (2011) ADHD medications and risk of serious cardiovascular events in young and middle-aged adults. JAMA 306(24):2673–2683. doi:10.1001/jama.2011.1830
Haffey MB, Buckwalter M, Zhang P, Homolka R, Martin P, Lasseter KC, Ermer JC (2009) Effects of omeprazole on the pharmacokinetic profiles of lisdexamfetamine dimesylate and extended-release mixed amphetamine salts in adults. Postgrad Med 121(5):11–19. doi:10.3810/pgm.2009.09.2048
Jain U, Hechtman L, Weiss M, Ahmed TS, Reiz JL, Donnelly GA, Harsanyi Z, Darke AC (2007) Efficacy of a novel biphasic controlled-release methylphenidate formula in adults with attention-deficit/hyperactivity disorder: results of a double-blind, placebo-controlled crossover study. J Clin Psychiatry 68(2):268–277
Jain R, Babcock T, Burtea T, Dirks B, Adeyi B, Scheckner B, Lasser R (2011) Efficacy of lisdexamfetamine dimesylate in children with attention-deficit/hyperactivity disorder previously treated with methylphenidate: a post hoc analysis. Child Adolesc Psychiatry Ment Health 5(1):35. doi:10.1186/1753-2000-5-35
James RS, Sharp WS, Bastain TM, Lee PP, Walter JM, Czarnolewski M, Castellanos FX (2001) Double-blind, placebo-controlled study of single-dose amphetamine formulations in ADHD. J Am Acad Child Adolesc Psychiatry 40(11):1268–1276. doi:10.1097/00004583-200111000-00006
Janssen Inc. Concerta® Product Monograph. Revised December 5, 2011. http://www.janssen.ca/product/98. Accessed 2 July 2012. Janssen Inc., Toronto, Ontario
Jasinski DR, Krishnan S (2009a) Abuse liability and safety of oral lisdexamfetamine dimesylate in individuals with a history of stimulant abuse. J Psychopharmacol 23(4):419–427. doi:10.1177/0269881109103113
Jasinski DR, Krishnan S (2009b) Human pharmacology of intravenous lisdexamfetamine dimesylate: abuse liability in adult stimulant abusers. J Psychopharmacol 23(4):410–418. doi:10.1177/0269881108093841
Kessler RC, Adler L, Barkley R, Biederman J, Conners CK, Demler O, Faraone SV, Greenhill LL, Howes MJ, Secnik K, Spencer T, Ustun TB, Walters EE, Zaslavsky AM (2006) The prevalence and correlates of adult ADHD in the United States: results from the National Comorbidity Survey Replication. Am J Psychiatry 163(4):716–723. doi:10.1176/appi.ajp.163.4.716
Klassen AF, Miller A, Fine S (2004) Health-related quality of life in children and adolescents who have a diagnosis of attention-deficit/hyperactivity disorder. Pediatrics 114(5):e541–e547. doi:10.1542/peds.2004-0844
Kollins SH (2008) ADHD, substance use disorders, and psychostimulant treatment: current literature and treatment guidelines. J Atten Disord 12(2):115–125. doi:10.1177/1087054707311654
Krishnan S, Zhang Y (2008) Relative bioavailability of lisdexamfetamine 70-mg capsules in fasted and fed healthy adult volunteers and in solution: a single-dose, crossover pharmacokinetic study. J Clin Pharmacol 48(3):293–302. doi:10.1177/0091270007310381
Lopez F, Silva R, Pestreich L, Muniz R (2003) Comparative efficacy of two once daily methylphenidate formulations (Ritalin LA and Concerta) and placebo in children with attention deficit hyperactivity disorder across the school day. Paediatr Drugs 5(8):545–555
Mao AR, Babcock T, Brams M (2011) ADHD in adults: current treatment trends with consideration of abuse potential of medications. J Psychiatr Pract 17(4):241–250. doi:10.1097/01.pra.0000400261.45290.bd
Marcus SC, Wan GJ, Kemner JE, Olfson M (2005) Continuity of methylphenidate treatment for attention-deficit/hyperactivity disorder. Arch Pediatr Adolesc Med 159(6):572–578. doi:10.1001/archpedi.159.6.572
McBurnett K, Starr HL (2011) OROS methylphenidate hydrochloride for adult patients with attention deficit/hyperactivity disorder. Expert Opin Pharmacother 12(2):315–324. doi:10.1517/14656566.2011.546058
McCracken JT, Biederman J, Greenhill LL, Swanson JM, McGough JJ, Spencer TJ, Posner K, Wigal S, Pataki C, Zhang Y, Tulloch S (2003) Analog classroom assessment of a once-daily mixed amphetamine formulation, SLI381 (Adderall XR), in children with ADHD. J Am Acad Child Adolesc Psychiatry 42(6):673–683. doi:10.1097/01.CHI.0000046863.56865.FE
McGough JJ, Biederman J, Greenhill LL, McCracken JT, Spencer TJ, Posner K, Wigal S, Gornbein J, Tulloch S, Swanson JM (2003) Pharmacokinetics of SLI381 (ADDERALL XR), an extended-release formulation of Adderall. J Am Acad Child Adolesc Psychiatry 42(6):684–691. doi:10.1097/01.CHI.0000046850.56865.CB
Medori R, Ramos-Quiroga JA, Casas M, Kooij JJ, Niemela A, Trott GE, Lee E, Buitelaar JK (2008) A randomized, placebo-controlled trial of three fixed dosages of prolonged-release OROS methylphenidate in adults with attention-deficit/hyperactivity disorder. Biol Psychiatry 63(10):981–989. doi:10.1016/j.biopsych.2007.11.008
Murray DW, Arnold LE, Swanson J, Wells K, Burns K, Jensen P, Hechtman L, Paykina N, Legato L, Strauss T (2008) A clinical review of outcomes of the multimodal treatment study of children with attention-deficit/hyperactivity disorder (MTA). Curr Psychiatry Rep 10(5):424–431
Murray DW, Childress A, Giblin J, Williamson D, Armstrong R, Starr HL (2011) Effects of OROS methylphenidate on academic, behavioral, and cognitive tasks in children 9 to 12 years of age with attention-deficit/hyperactivity disorder. Clin Pediatr (Phila) 50(4):308–320. doi:10.1177/0009922810394832
National Institute for Health and Clinical Excellence (2009) Diagnosis and management of ADHD in children, young people and adults. National Clinical Practice Guideline Number 72. London, UK. http://www.nice.org.uk/nicemedia/pdf/ADHDFullGuideline.pdf. Accessed 2 July 2012
Novartis Pharmaceuticals Canada Inc. Ritalin® SR Product Monograph. Revised September 14, 2011. Novartis Pharmaceuticals Canada Inc., Dorval, Quebec
Pappadopulos E, Jensen PS, Chait AR, Arnold LE, Swanson JM, Greenhill LL, Hechtman L, Chuang S, Wells KC, Pelham W, Cooper T, Elliott G, Newcorn JH (2009) Medication adherence in the MTA: saliva methylphenidate samples versus parent report and mediating effect of concomitant behavioral treatment. J Am Acad Child Adolesc Psychiatry 48(5):501–510. doi:10.1097/CHI.0b013e31819c23ed
Parasrampuria DA, Schoedel KA, Schuller R, Gu J, Ciccone P, Silber SA, Sellers EM (2007) Assessment of pharmacokinetics and pharmacodynamic effects related to abuse potential of a unique oral osmotic-controlled extended-release methylphenidate formulation in humans. J Clin Pharmacol 47(12):1476–1488. doi:10.1177/0091270007308615
Pelham WE Jr, Sturges J, Hoza J, Schmidt C, Bijlsma JJ, Milich R, Moorer S (1987) Sustained release and standard methylphenidate effects on cognitive and social behavior in children with attention deficit disorder. Pediatrics 80(4):491–501
Pelham WE Jr, Greenslade KE, Vodde-Hamilton M, Murphy DA, Greenstein JJ, Gnagy EM, Guthrie KJ, Hoover MD, Dahl RE (1990) Relative efficacy of long-acting stimulants on children with attention deficit-hyperactivity disorder: a comparison of standard methylphenidate, sustained-release methylphenidate, sustained-release dextroamphetamine, and pemoline. Pediatrics 86(2):226–237
Pelham WE, Gnagy EM, Burrows-Maclean L, Williams A, Fabiano GA, Morrisey SM, Chronis AM, Forehand GL, Nguyen CA, Hoffman MT, Lock TM, Fielbelkorn K, Coles EK, Panahon CJ, Steiner RL, Meichenbaum DL, Onyango AN, Morse GD (2001) Once-a-day Concerta methylphenidate versus three-times-daily methylphenidate in laboratory and natural settings. Pediatrics 107(6):E105. doi:10.1542/peds.107.6.e105
Pennick M (2010) Absorption of lisdexamfetamine dimesylate and its enzymatic conversion to d-amphetamine. Neuropsychiatr Dis Treat 6:317–327
Pliszka S (2007) Practice parameter for the assessment and treatment of children and adolescents with attention-deficit/hyperactivity disorder. J Am Acad Child Adolesc Psychiatry 46(7):894–921. doi:10.1097/chi.0b013e318054e724
Polanczyk G, de Lima MS, Horta BL, Biederman J, Rohde LA (2007) The worldwide prevalence of ADHD: a systematic review and metaregression analysis. Am J Psychiatry 164(6):942–948. doi:10.1176/appi.ajp.164.6.942
Quinn D, Bode T, Reiz JL, Donnelly GA, Darke AC (2007) Single-dose pharmacokinetics of multilayer-release methylphenidate and immediate-release methylphenidate in children with attention-deficit/hyperactivity disorder. J Clin Pharmacol 47(6):760–766. doi:10.1177/0091270007299759
Ramos-Quiroga JA, Bosch R, Castells X, Valero S, Nogueira M, Gomez N, Yelmo S, Ferrer M, Martinez Y, Casas M (2008) Effect of switching drug formulations from immediate-release to extended-release OROS methylphenidate : a chart review of Spanish adults with attention-deficit hyperactivity disorder. CNS Drugs 22(7):603–611
Shire Canada Inc. Adderall XR® Product Monograph. December 20, 2011. Shire Canada Inc., Saint-Laurent, Quebec
Shire Canada Inc. Vyvanse® Product Monograph. December 21, 2011. Shire Canada Inc., Saint-Laurent, Quebec
Safer DJ (1992) Relative cardiovascular safety of psychostimulants used to treat attention-deficit hyperactivity disorder. J Child Adolesc Psychopharmacol 2(4):279–290. doi:10.1089/cap.1992.2.279
Sanchez RJ, Crismon ML, Barner JC, Bettinger T, Wilson JP (2005) Assessment of adherence measures with different stimulants among children and adolescents. Pharmacotherapy 25(7):909–917
Sawyer MG, Whaites L, Rey JM, Hazell PL, Graetz BW, Baghurst P (2002) Health-related quality of life of children and adolescents with mental disorders. J Am Acad Child Adolesc Psychiatry 41(5):530–537. doi:10.1097/00004583-200205000-00010
Schachar R, Ickowicz A, Crosbie J, Donnelly GA, Reiz JL, Miceli PC, Harsanyi Z, Darke AC (2008) Cognitive and behavioral effects of multilayer-release methylphenidate in the treatment of children with attention-deficit/hyperactivity disorder. J Child Adolesc Psychopharmacol 18(1):11–24. doi:10.1089/cap.2007.0039
Silva R, Muniz R, Pestreich LK, Brams M, Childress A, Lopez FA (2005) Efficacy of two long-acting methylphenidate formulations in children with attention- deficit/hyperactivity disorder in a laboratory classroom setting. J Child Adolesc Psychopharmacol 15(4):637–654. doi:10.1089/cap.2005.15.637
Spencer TJ, Biederman J, Ciccone PE, Madras BK, Dougherty DD, Bonab AA, Livni E, Parasrampuria DA, Fischman AJ (2006a) PET study examining pharmacokinetics, detection and likeability, and dopamine transporter receptor occupancy of short- and long-acting oral methylphenidate. Am J Psychiatry 163(3):387–395. doi:10.1176/appi.ajp.163.3.387
Spencer TJ, Wilens TE, Biederman J, Weisler RH, Read SC, Pratt R (2006b) Efficacy and safety of mixed amphetamine salts extended release (Adderall XR) in the management of attention-deficit/hyperactivity disorder in adolescent patients: a 4-week, randomized, double-blind, placebo-controlled, parallel-group study. Clin Ther 28(2):266–279. doi:10.1016/j.clinthera.2006.02.011
Spencer TJ, Mick E, Surman CB, Hammerness P, Doyle R, Aleardi M, Kotarski M, Williams CG, Biederman J (2011) A randomized, single-blind, substitution study of OROS methylphenidate (Concerta) in ADHD adults receiving immediate release methylphenidate. J Atten Disord 15(4):286–294. doi:10.1177/1087054710367880
Swanson J (2003) Compliance with stimulants for attention-deficit/hyperactivity disorder: issues and approaches for improvement. CNS Drugs 17(2):117–131
Swanson JM, Volkow ND (2009) Psychopharmacology: concepts and opinions about the use of stimulant medications. J Child Psychol Psychiatry 50(1–2):180–193. doi:10.1111/j.1469-7610.2008.02062.x
Swanson J, Gupta S, Lam A, Shoulson I, Lerner M, Modi N, Lindemulder E, Wigal S (2003) Development of a new once-a-day formulation of methylphenidate for the treatment of attention-deficit/hyperactivity disorder: proof-of-concept and proof-of-product studies. Arch Gen Psychiatry 60(2):204–211
Swanson JM, Wigal SB, Wigal T, Sonuga-Barke E, Greenhill LL, Biederman J, Kollins S, Nguyen AS, DeCory HH, Hirshe Dirksen SJ, Hatch SJ (2004) A comparison of once-daily extended-release methylphenidate formulations in children with attention-deficit/hyperactivity disorder in the laboratory school (the COMACS Study). Pediatrics 113(3 Pt 1):e206–e216
Swanson JM, Elliott GR, Greenhill LL, Wigal T, Arnold LE, Vitiello B, Hechtman L, Epstein JN, Pelham WE, Abikoff HB, Newcorn JH, Molina BS, Hinshaw SP, Wells KC, Hoza B, Jensen PS, Gibbons RD, Hur K, Stehli A, Davies M, March JS, Conners CK, Caron M, Volkow ND (2007) Effects of stimulant medication on growth rates across 3 years in the MTA follow-up. J Am Acad Child Adolesc Psychiatry 46(8):1015–1027. doi:10.1097/chi.0b013e3180686d7e
Tulloch SJ, Zhang Y, McLean A, Wolf KN (2002) SLI381 (Adderall XR), a two-component, extended-release formulation of mixed amphetamine salts: bioavailability of three test formulations and comparison of fasted, fed, and sprinkled administration. Pharmacotherapy 22(11):1405–1415
van den Ban E, Souverein PC, Swaab H, van Engeland H, Egberts TC, Heerdink ER (2010) Less discontinuation of ADHD drug use since the availability of long-acting ADHD medication in children, adolescents and adults under the age of 45 years in the Netherlands. Atten Defic Hyperact Disord 2(4):213–220. doi:10.1007/s12402-010-0044-9
Vetter VL, Elia J, Erickson C, Berger S, Blum N, Uzark K, Webb CL (2008) Cardiovascular monitoring of children and adolescents with heart disease receiving medications for attention deficit/hyperactivity disorder [corrected]: a scientific statement from the American Heart Association Council on Cardiovascular Disease in the Young Congenital Cardiac Defects Committee and the Council on Cardiovascular Nursing. Circulation 117(18):2407–2423. doi:10.1161/circulationaha.107.189473
Volkow ND, Swanson JM (2003) Variables that affect the clinical use and abuse of methylphenidate in the treatment of ADHD. Am J Psychiatry 160(11):1909–1918
Weisler RH, Biederman J, Spencer TJ, Wilens TE, Faraone SV, Chrisman AK, Read SC, Tulloch SJ (2006) Mixed amphetamine salts extended-release in the treatment of adult ADHD: a randomized, controlled trial. CNS Spectr 11(8):625–639
Weiss M, Hechtman L, Turgay A, Jain U, Quinn D, Ahmed TS, Yates T, Reiz JL, Donnelly GA, Harsanyi Z, Darke AC (2007) Once-daily multilayer-release methylphenidate in a double-blind, crossover comparison to immediate-release methylphenidate in children with attention-deficit/hyperactivity disorder. J Child Adolesc Psychopharmacol 17(5):675–688. doi:10.1089/cap.2006.0101
Wigal SB, Kollins SH, Childress AC, Squires L (2009) A 13-h laboratory school study of lisdexamfetamine dimesylate in school-aged children with attention-deficit/hyperactivity disorder. Child Adolesc Psychiatry Ment Health 3(1):17. doi:10.1186/1753-2000-3-17
Wigal T, Brams M, Gasior M, Gao J, Squires L, Giblin J (2010) Randomized, double-blind, placebo-controlled, crossover study of the efficacy and safety of lisdexamfetamine dimesylate in adults with attention-deficit/hyperactivity disorder: novel findings using a simulated adult workplace environment design. Behav Brain Funct 6:34. doi:10.1186/1744-9081-6-34
Wigal SB, Wigal T, Schuck S, Brams M, Williamson D, Armstrong RB, Starr HL (2011) Academic, behavioral, and cognitive effects of OROS(R) methylphenidate on older children with attention-deficit/hyperactivity disorder. J Child Adolesc Psychopharmacol 21(2):121–131. doi:10.1089/cap.2010.0047
Wilens TE, Hammerness PG, Biederman J, Kwon A, Spencer TJ, Clark S, Scott M, Podolski A, Ditterline JW, Morris MC, Moore H (2005) Blood pressure changes associated with medication treatment of adults with attention-deficit/hyperactivity disorder. J Clin Psychiatry 66(2):253–259
Wilens TE, McBurnett K, Bukstein O, McGough J, Greenhill L, Lerner M, Stein MA, Conners CK, Duby J, Newcorn J, Bailey CE, Kratochvil CJ, Coury D, Casat C, Denisco MJ, Halstead P, Bloom L, Zimmerman BA, Gu J, Cooper KM, Lynch JM (2006a) Multisite controlled study of OROS methylphenidate in the treatment of adolescents with attention-deficit/hyperactivity disorder. Arch Pediatr Adolesc Med 160(1):82–90. doi:10.1001/archpedi.160.1.82
Wilens TE, Prince JB, Spencer TJ, Biederman J (2006b) Stimulants and sudden death: what is a physician to do? Pediatrics 118(3):1215–1219. doi:10.1542/peds.2006-0942
Wilens TE, Adler LA, Adams J, Sgambati S, Rotrosen J, Sawtelle R, Utzinger L, Fusillo S (2008) Misuse and diversion of stimulants prescribed for ADHD: a systematic review of the literature. J Am Acad Child Adolesc Psychiatry 47(1):21–31. doi:10.1097/chi.0b013e31815a56f1
Winterstein AG, Gerhard T, Shuster J, Johnson M, Zito JM, Saidi A (2007) Cardiac safety of central nervous system stimulants in children and adolescents with attention-deficit/hyperactivity disorder. Pediatrics 120(6):e1494–e1501. doi:10.1542/peds.2007-0675
Winterstein AG, Gerhard T, Shuster J, Saidi A (2009) Cardiac safety of methylphenidate versus amphetamine salts in the treatment of ADHD. Pediatrics 124(1):e75–e80. doi:10.1542/peds.2008-3138
Wolraich ML, Greenhill LL, Pelham W, Swanson J, Wilens T, Palumbo D, Atkins M, McBurnett K, Bukstein O, August G (2001) Randomized, controlled trial of OROS methylphenidate once a day in children with attention-deficit/hyperactivity disorder. Pediatrics 108(4):883–892
World Health Organization (2003) Adherence to long-term therapies: evidence for action. World Health Organization, Geneva
Acknowledgments
The authors wish to pay tribute to their late colleague, Atilla Turgay, MD, and recognize his contributions to earlier drafts of this article.
The content of this manuscript, the ultimate interpretation, and the decision to submit it for publication in ADHD Attention Deficit and Hyperactivity Disorders were made independently by the authors. Writing and editing support for this manuscript was provided by Ogilvy CommonHealth Scientific Communications and Oxford PharmaGenesis™ Ltd and funded by Shire Development LLC.
Conflict of interest
Frank A. López, MD, is a consultant for Bristol-Myers Squibb, Celltech, Cephalon, Eli Lilly, New River Pharmaceuticals, Novartis, Pfizer, and Shire US; has received grant/research support from Bristol-Myers Squibb, Celltech, Cephalon, Eli Lilly, New River Pharmaceuticals, Novartis, Pfizer, and Shire; is on the speakers bureau for Cephalon, Novartis, and Shire; and is an advisory board member for Celltech, Cephalon, Eli Lilly, Novartis, and Shire. Jacques R. Leroux, MD, is a consultant or speaker for Canadian Psychiatric Association, Eli Lilly, Janssen Ortho, Le regroupement PANDA, Purdue Pharma, and Shire.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is dedicated to the memory of Atilla Turgay.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution License which permits any use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited.
About this article
Cite this article
López, F.A., Leroux, J.R. Long-acting stimulants for treatment of attention-deficit/hyperactivity disorder: a focus on extended-release formulations and the prodrug lisdexamfetamine dimesylate to address continuing clinical challenges. ADHD Atten Def Hyp Disord 5, 249–265 (2013). https://doi.org/10.1007/s12402-013-0106-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12402-013-0106-x