Abstract
Background
We previously developed a deep-learning (DL) network for image denoising in SPECT-myocardial perfusion imaging (MPI). Here we investigate whether this DL network can be utilized for improving detection of perfusion defects in standard-dose clinical acquisitions.
Methods
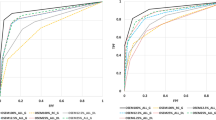
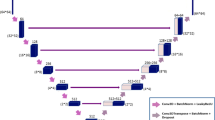
To quantify perfusion-defect detection accuracy, we conducted a receiver-operating characteristic (ROC) analysis on reconstructed images with and without processing by the DL network using a set of clinical SPECT-MPI data from 190 subjects. For perfusion-defect detection hybrid studies were used as ground truth, which were created from clinically normal studies with simulated realistic lesions inserted. We considered ordered-subset expectation-maximization (OSEM) reconstruction with corrections for attenuation, resolution, and scatter and with 3D Gaussian post-filtering. Total perfusion deficit (TPD) scores, computed by Quantitative Perfusion SPECT (QPS) software, were used to evaluate the reconstructed images.
Results
Compared to reconstruction with optimal Gaussian post-filtering (sigma = 1.2 voxels), further DL denoising increased the area under the ROC curve (AUC) from 0.80 to 0.88 (P-value < 10−4). For reconstruction with less Gaussian post-filtering (sigma = 0.8 voxels), thus better spatial resolution, DL denoising increased the AUC value from 0.78 to 0.86 (P-value < 10−4) and achieved better spatial resolution in reconstruction.
Conclusions
DL denoising can effectively improve the detection of abnormal defects in standard-dose SPECT-MPI images over conventional reconstruction.








Similar content being viewed by others
Abbreviations
- SPECT:
-
Single-photon emission computed tomography
- MPI:
-
Myocardial perfusion imaging
- LV:
-
Left ventricular
- OSEM:
-
Ordered-subset expectation-maximization
- AC:
-
Attenuation correction
- SC:
-
Scatter correction
- RC:
-
Resolution correction
- AUC:
-
Area under the ROC curve
- TPD:
-
Total perfusion deficit
- DL:
-
Deep learning
References
Sabharwal NK, Lahiri A. Role of myocardial perfusion imaging for risk stratification in suspected or known coronary artery disease. Heart 2003;89:1291-7. https://doi.org/10.1136/heart.89.11.1291.
Lyra M, Ploussi A. Filtering in SPECT image reconstruction. Int J Biomed Imaging 2011;2011:2-43. https://doi.org/10.1155/2011/693795.
Liu H, Wang K, Tian J. Postreconstruction filtering of 3D PET images by using weighted higher-order singular value decomposition. Biomed Eng Online 2016;15:1-20. https://doi.org/10.1186/s12938-016-0221-y.
Kim HS, Cho S-G, Kim JH, Kwon SY, Lee B-I, Bom H-S. Effect of post-reconstruction gaussian filtering on image quality and myocardial blood flow measurement with N-13 ammonia PET. Asia Ocean J Nucl Med Biol 2014;2(2):104-10.
Juan Ramon A, Yang Y, Pretorius PH, et al. Investigation of dose reduction in cardiac perfusion SPECT via optimization and choice of the image reconstruction strategy. J Nucl Cardiol 2018;25:2117-28. https://doi.org/10.1007/s12350-017-0920-1.
Chen H, Zhang Y, Kalra MK, et al. Low-dose CT with a residual encoder–decoder convolutional neural network (RED-CNN). IEEE Trans Med Imaging 2017;36:2524-35. https://doi.org/10.1109/TMI.2017.2715284.
Liu J, Zarshenas A, Wei Z, et al. Radiation dose reduction in digital breast tomosynthesis (DBT) by means of deep-learning-based supervised image processing. In: Angelini ED, Landman BA, eds. Medical Imaging 2018: Image Processing. Vol 10574. SPIE; 2018:14. https://doi.org/10.1117/12.2293125
Chan C, Zhou J, Yang L, Qi W, Asma E. Noise to noise ensemble learning for PET image denoising. https://www.researchgate.net/publication/339363866. Accessed March 31, 2020.
Ramon AJ, Yang Y, Pretorius PH, Johnson KL, King MA, Wernick MN. Improving diagnostic accuracy in low-dose SPECT myocardial perfusion imaging with convolutional denoising networks. IEEE Trans Med Imaging 2020;39:2893-903. https://doi.org/10.1109/tmi.2020.2979940.
Liu J, Yang Y, Wernick MN, Pretorius PH, King MA. Deep learning with noise-to-noise training for denoising in SPECT myocardial perfusion imaging. Med Phys 2021;48:156-68. https://doi.org/10.1002/mp.14577.
Lehtinen J, Munkberg J, Hasselgren J, et al. Noise2Noise: Learning Image Restoration without Clean Data. In: International Conference on Machine Learning (ICML); 2018. http://arxiv.org/abs/1803.04189. Accessed November 6, 2018.
Arsanjani R, Xu Y, Hayes SW, et al. Comparison of fully automated computer analysis and visual scoring for detection of coronary artery disease from myocardial perfusion SPECT in a large population NIH Public Access. J Nucl Med 2013;54:221-8. https://doi.org/10.2967/jnumed.112.108969.
Slomka PJ, Nishina H, Berman DS, et al. Automated quantification of myocardial perfusion SPECT using simplified normal limits. J Nucl Cardiol 2005;12:66-77. https://doi.org/10.1016/j.nuclcard.2004.10.006.
Bai C, Shao L, Da Silva AJ, Zhao Z. A generalized model for the conversion from CT numbers to linear attenuation coefficients. IEEE Nucl Sci Symp Med Imaging Conf 2002;2:1188-92. https://doi.org/10.1109/nssmic.2002.1239533.
Ogawa K, Harata Y, Ichihara T, Kubo A, Hashimoto S. A practical method for position-dependent compton-scatter correction in single photon emission CT. IEEE Trans Med Imaging 1991;10:408-12. https://doi.org/10.1109/42.97591.
Pretorius PH, King MA, Johnson KL, Yang Y, Wernick MN. Introducing Polar Map Defined Defects into Normal Cardiac Perfusion SPECT Slices using 3D Respiratory and Rigid-Body Motion Projection. In: The 13th International Meeting on Fully Three-Dimensional Image Reconstruction in Radiology and Nuclear Medicine.; 2015:1-4.
Narayanan MV, King MA, Hendrik Pretorius P, et al. Human-observer receiver-operating-characteristic evaluation of attenuation, scatter, and resolution compensation strategies for 99mTc myocardial perfusion imaging. J Nucl Med 2003;44:1725-34.
Tang Z, Peng X, Li K, Metaxas DN. Towards efficient U-nets: a coupled and quantized approach. IEEE Trans Pattern Anal Mach Intell 2019. https://doi.org/10.1109/tpami.2019.2907634.
scikit-learn: machine learning in Python—scikit-learn 0.23.1 documentation. https://scikit-learn.org/stable/#. Accessed June 2, 2020.
Acknowledgments
This work was supported by the National Heart, Lung, and Blood Institute of the National Institutes of Health under Award Number R01 HL154687.
Disclosure
The University of Massachusetts had a research agreement with Philips Healthcare at the time some of this work was performed. The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This work was supported by the National Institutes of Health (NIH) Grant R01 HL154687. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
The authors of this article have provided a PowerPoint file, available for download at SpringerLink, which summarises the contents of the paper and is free for re-use at meetings and presentations. Search for the article DOI on SpringerLink.com.
The authors have also provided an audio summary of the article, which is available to download as ESM, or to listen to via the JNC/ASNC Podcast.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Liu, J., Yang, Y., Wernick, M.N. et al. Improving detection accuracy of perfusion defect in standard dose SPECT-myocardial perfusion imaging by deep-learning denoising. J. Nucl. Cardiol. 29, 2340–2349 (2022). https://doi.org/10.1007/s12350-021-02676-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12350-021-02676-w