Abstract
Background
Non-alcoholic fatty liver disease (NAFLD) has emerged as an independent risk factor for cardiovascular diseases. However, there were few studies evaluating the condition of myocardial glucose metabolism in patients with NAFLD. Therefore, the aim of this study was to investigate the association between NAFLD and myocardial glucose uptake assessed by using 18F-fluorodeoxyglucose (18F-FDG) positron emission tomography (PET) and whether or not alteration of myocardial glucose uptake could be an indicator linking to cardiac dysfunction in NAFLD individuals.
Methods and Results
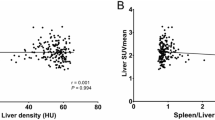
A total of 743 asymptomatic subjects (201 with NAFLD, 542 without NAFLD) were retrospectively studied. The ratio of maximum myocardium FDG uptake to the mean standardized uptake value of liver (SUVratio) was calculated to estimate myocardial glucose uptake by using 18F-FDG PET. The diagnosis of fatty liver and fatty liver grading was confirmed by unenhanced CT according to diagnostic criterion of previous studies. The myocardial geometric and functional data were obtained by echocardiogram. Myocardial glucose uptake was significantly lower in individuals with NAFLD compared with those without fatty liver (P < .001). When analysis of association trend was performed, SUVratio quartiles showed correlated inversely and strongly with liver steatosis (P < .001). NAFLD patients with lower myocardial glucose uptake were more likely to have higher proportion of increased LV filling pressure (P < .05). A significant relationship between myocardial SUVratio and E/e’ ratio was presented in the trend analysis (P < .05). Moreover, multivariate regression analysis showed that myocardial glucose uptake was independently associated with NAFLD after adjusting for clinical important factors (all P < .001).
Conclusions
The presence of NAFLD in otherwise healthy subjects is closely associated with decreased myocardial glucose uptake assessing by 18F-FDG PET imaging. Furthermore, the NAFLD individuals with lower myocardial glucose uptake are more likely to have high risk of having impaired diastolic heart function.






Similar content being viewed by others
Abbreviations
- BMI:
-
Body mass index
- CT:
-
Computed tomography
- CVD:
-
Cardiovascular diseases
- FDG:
-
Fluorodeoxyglucose
- FFA:
-
Free fatty acids
- LV:
-
Left ventricular
- NAFLD:
-
Non-alcoholic fatty liver disease
- OR:
-
Odds ratio
- PET:
-
Positron emission tomography
- SUV:
-
Standardized uptake value
References
Younossi ZM, Koenig AB, Abdelatif D, Fazel Y, Henry L, Wymer M. Global epidemiology of nonalcoholic fatty liver disease-meta-analytic assessment of prevalence, incidence, and outcomes. Hepatology 2016;64:73-84.
Lazo M, Hernaez R, Eberhardt MS, Bonekamp S, Kamel I, Guallar E, et al. Prevalence of nonalcoholic fatty liver disease in the United States: the Third National Health and Nutrition Examination Survey, 1988-1994. Am J Epidemiol 2013;178:38-45.
Eslam M, Valenti L, Romeo S. Genetics and epigenetics of NAFLD and NASH: Clinical impact. J Hepatol 2018;68:268-79.
Haddad TM, Hamdeh S, Kanmanthareddy A, Alla VM. Nonalcoholic fatty liver disease and the risk of clinical cardiovascular events: A systematic review and meta-analysis. Diabetes Metab Syndr 2017;11(Suppl 1):S209-16.
Lee HJ, Lee CH, Kim S, Hwang SY, Hong HC, Choi HY, et al. Association between vascular inflammation and non-alcoholic fatty liver disease: Analysis by (18)F-fluorodeoxyglucose positron emission tomography. Metabolism 2017;67:72-9.
Ong JP, Pitts A, Younossi ZM. Increased overall mortality and liver-related mortality in non-alcoholic fatty liver disease. J Hepatol 2008;49:608-12.
Sert A, Aypar E, Pirgon O, Yilmaz H, Odabas D, Tolu I. Left ventricular function by echocardiography, tissue doppler imaging, and carotid intima-media thickness in obese adolescents with nonalcoholic fatty liver disease. Am J Cardiol 2013;112:436-43.
Alp H, Karaarslan S, Eklioglu BS, Atabek ME, Altin H, Baysal T. Association between nonalcoholic fatty liver disease and cardiovascular risk in obese children and adolescents. Can J Cardiol 2013;29:1118-25.
Fotbolcu H, Yakar T, Duman D, Karaahmet T, Tigen K, Cevik C, et al. Impairment of the left ventricular systolic and diastolic function in patients with non-alcoholic fatty liver disease. Cardiol J 2010;17:457-63.
Fracanzani AL, Pisano G, Consonni D, Tiraboschi S, Baragetti A, Bertelli C, et al. Epicardial adipose tissue (EAT) thickness is associated with cardiovascular and liver damage in nonalcoholic fatty liver disease. PLoS ONE 2016;11:e0162473.
Pais R, Giral P, Khan J-F, Rosenbaum D, Housset C, Poynard T, et al. Fatty liver is an independent predictor of early carotid atherosclerosis. J Hepatol 2016;65:95-102.
Santoro N, Caprio S, Giannini C, Kim G, Kursawe R, Pierpont B, et al. Oxidized fatty acids: A potential pathogenic link between fatty liver and type 2 diabetes in obese adolescents? Antioxid Redox Sign 2014;20:383-9.
Lautamaki R, Borra R, Iozzo P, Komu M, Lehtimaki T, Salmi M, et al. Liver steatosis coexists with myocardial insulin resistance and coronary dysfunction in patients with type 2 diabetes. Am J Physiol Endocrinol Metab 2006;291:E282-90.
Gaggini M, Morelli M, Buzzigoli E, DeFronzo RA, Bugianesi E, Gastaldelli A. Non-alcoholic fatty liver disease (NAFLD) and its connection with insulin resistance, dyslipidemia, atherosclerosis and coronary heart disease. Nutrients 2013;5:1544-60.
Masoud WG, Ussher JR, Wang W, Jaswal JS, Wagg CS, Dyck JR, et al. Failing mouse hearts utilize energy inefficiently and benefit from improved coupling of glycolysis and glucose oxidation. Cardiovasc Res 2014;101:30-8.
Nagueh SF, Smiseth OA, Appleton CP, Byrd BF 3rd, Dokainish H, Edvardsen T, et al. Recommendations for the evaluation of left ventricular diastolic function by echocardiography: An update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr 2016;29:277-314.
Boyce CJ, Pickhardt PJ, Kim DH, Taylor AJ, Winter TC, Bruce RJ, et al. Hepatic steatosis (fatty liver disease) in asymptomatic adults identified by unenhanced low-dose CT. AJR Am J Roentgenol 2010;194:623-8.
Park YS, Park SH, Lee SS, Kim DY, Shin YM, Lee W, et al. Biopsy-proven nonsteatotic liver in adults: Estimation of reference range for difference in attenuation between the liver and the spleen at nonenhanced CT. Radiology 2011;258:760-6.
Lee YH, Kim KJ, Yoo ME, Kim G, Yoon HJ, Jo K, et al. Association of non-alcoholic steatohepatitis with subclinical myocardial dysfunction in non-cirrhotic patients. J Hepatol 2017. https://doi.org/10.1016/j.jhep.2017.11.023.
Hasegawa S, Kusuoka H, Uehara T, Yamaguchi H, Hori M, Nishimura T. Glucose tolerance and myocardial F-18 fluorodeoxyglucose uptake in normal regions in coronary heart disease patients. Ann Nucl Med 1998;12:363-8.
Tamaki N, Yonekura Y, Konishi J. Myocardial FDG PET studies with the fasting, oral glucose-loading or insulin clamp methods. J Nucl Med 1992;33:66-8.
van den Brom CE, Bulte CS, Loer SA, Bouwman RA, Boer C. Diabetes, perioperative ischaemia and volatile anaesthetics: consequences of derangements in myocardial substrate metabolism. Cardiovasc Diabetol 2013;12:42.
Kim G, Jo K, Kim KJ, Lee YH, Han E, Yoon HJ, et al. Visceral adiposity is associated with altered myocardial glucose uptake measured by (18)FDG-PET in 346 subjects with normal glucose tolerance, prediabetes, and type 2 diabetes. Cardiovasc Diabetol 2015;14:148.
Abikhzer G, Alabed YZ, Azoulay L, Assayag J, Rush C. Altered hepatic metabolic activity in patients with hepatic steatosis on FDG PET/CT. AJR Am J Roentgenol 2011;196:176-80.
Abele JT, Fung CI. Effect of hepatic steatosis on liver FDG uptake measured in mean standard uptake values. Radiology 2010;254:917-24.
Keramida G, Potts J, Bush J, Dizdarevic S, Peters AM. Hepatic steatosis is associated with increased hepatic FDG uptake. Eur J Radiol 2014;83:751-5.
Aerni-Flessner L, Abi-Jaoude M, Koenig A, Payne M, Hruz PW. GLUT4, GLUT1, and GLUT8 are the dominant GLUT transcripts expressed in the murine left ventricle. Cardiovasc Diabetol 2012;11:63.
Kouidhi S, Berrhouma R, Rouissi K, Jarboui S, Clerget-Froidevaux MS, Seugnet I, et al. Human subcutaneous adipose tissue Glut 4 mRNA expression in obesity and type 2 diabetes. Acta Diabetol 2013;50:227-32.
Mazumder PK, O’Neill BT, Roberts MW, Buchanan J, Yun UJ, Cooksey RC, et al. Impaired cardiac efficiency and increased fatty acid oxidation in insulin-resistant ob/ob mouse hearts. Diabetes 2004;53:2366-74.
Yilmaz Y, Kurt R, Yonal O, Polat N, Celikel CA, Gurdal A, et al. Coronary flow reserve is impaired in patients with nonalcoholic fatty liver disease: Association with liver fibrosis. Atherosclerosis 2010;211:182-6.
Yilmaz Y, Kurt R, Gurdal A, Alahdab YO, Yonal O, Senates E, et al. Circulating vaspin levels and epicardial adipose tissue thickness are associated with impaired coronary flow reserve in patients with nonalcoholic fatty liver disease. Atherosclerosis 2011;217:125-9.
Wong VWS, Wong GLH, Yip GWK, Lo AOS, Limquiaco J, Chu WCW, et al. Coronary artery disease and cardiovascular outcomes in patients with non-alcoholic fatty liver disease. Gut 2011;60:1721-7.
Lee SH, Yun SJ, Kim DH, Jo HH, Park YS. Severity of nonalcoholic fatty liver disease on sonography and risk of coronary heart disease. J Clin Ultrasound 2017;45:391-9.
Faasse S, Braun H, Vos M. The role of NAFLD in cardiometabolic disease: An update. F1000Res 2018;7:170.
Abenavoli L, Peta V. Role of adipokines and cytokines in non-alcoholic fatty liver disease. Rev Recent Clin Trials 2014;9:134-40.
Aljaroudi W, Alraies MC, Halley C, Rodriguez L, Grimm RA, Thomas JD, et al. Impact of progression of diastolic dysfunction on mortality in patients with normal ejection fraction. Circulation 2012;125:782-8.
Sunbul M, Kivrak T, Durmus E, Akin H, Aydin Y, Ergelen R, et al. Nonalcoholic steatohepatitis score is an independent predictor of right ventricular dysfunction in patients with nonalcoholic fatty liver disease. Cardiovasc Ther 2015;33:294-9.
Lee SW, Park SH, Kim KW, Choi EK, Shin YM, Kim PN, et al. Unenhanced CT for assessment of macrovesicular hepatic steatosis in living liver donors: Comparison of visual grading with liver attenuation index. Radiology 2007;244:479-85.
Pickhardt PJ, Park SH, Hahn L, Lee SG, Bae KT, Yu ES. Specificity of unenhanced CT for non-invasive diagnosis of hepatic steatosis: Implications for the investigation of the natural history of incidental steatosis. Eur Radiol 2012;22:1075-82.
Limanond P, Raman SS, Lassman C, Sayre J, Ghobrial RM, Busuttil RW, et al. Macrovesicular hepatic steatosis in living related liver donors: Correlation between CT and histologic findings. Radiology 2004;230:276-80.
Author Contributions
KT drafted the manuscript and contributed to the data analysis. XZ and JL contributed to clinical data acquisition and PET images analysis. MZ contributed to the data Statistical analysis. HL contributed to echocardiographic images analysis. TL contributed to CT images analysis. LW contributed to the study design and manuscript drafting. All authors read and approved the final version of the manuscript.
Disclosure
None declared.
Author information
Authors and Affiliations
Corresponding author
Additional information
The authors of this article have provided a PowerPoint file, available for download at SpringerLink, which summarises the contents of the paper and is free for re-use at meetings and presentations. Search for the article DOI on SpringerLink.com.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Tang, K., Zheng, X., Lin, J. et al. Association between non-alcoholic fatty liver disease and myocardial glucose uptake measured by 18F-fluorodeoxyglucose positron emission tomography. J. Nucl. Cardiol. 27, 1679–1688 (2020). https://doi.org/10.1007/s12350-018-1446-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12350-018-1446-x