Abstract
Background
Diabetes mellitus induces structural and functional cardiac alterations that can result in heart failure. Left ventricular (LV) shape is a dynamic component of cardiac geometry influencing its contractile function. However, few data are available comparing LV shape index in diabetic and nondiabetic patients without overt coronary artery disease after balancing for coronary risk factors.
Methods
We studied 1168 patients with normal myocardial perfusion and normal LV ejection fraction on stress gated single-photon emission computed tomography (SPECT) imaging. To account for differences in baseline characteristics between diabetic and nondiabetic patients, we created a propensity score-matched cohort considering clinical variables, coronary risk factors, and stress type.
Results
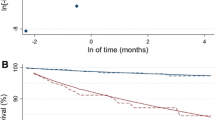
Before matching, diabetic patients were older, had higher prevalence of male gender and coronary risk factors, and higher end-diastolic and end-systolic LV shape index. After matching, all clinical characteristics were comparable between diabetic and nondiabetic patients, but diabetic patients still had higher end-diastolic and end-systolic LV shape index (both P < .001). At multivariable linear regression analysis, diabetes was a strong predictor of end-systolic LV shape index in the overall study population and in the propensity-matched cohort.
Conclusions
Diabetic patients have higher values of LV shape index compared to nondiabetic patients also after balancing clinical characteristics by propensity score analysis. Shape indexes assessment by gated SPECT may be useful for identifying early LV remodeling in patients with diabetes.
Spanish Abstract
Antecedentes
La Diabetes Mellitus induce alteraciones cardiacas a nivel estructural y funcional que pueden resultar en insuficiencia cardiaca. La forma ventricular izquierda (VI) es un componente dinámico de la geometría cardiaca que influye en su función contráctil. Sin embargo, existen pocos datos disponibles que comparen el Índice de Forma VI en pacientes diabéticos y no diabéticos sin enfermedad arterial coronaria después de equilibrar los factores de riesgo coronario.
Métodos
Estudiamos 1168 pacientes con perfusión miocárdica normal así como fracción de eyección del ventrículo izquierdo normal en la fase de estrés del gated SPECT. Para establecer las diferencias en las características basales entre pacientes diabéticos y no diabéticos, se creó una cohorte de puntuación de propensión teniendo en cuenta las variables clínicas, factores de riesgo coronario y tipo de estrés.
Resultados
Antes del emparejamiento, los pacientes diabéticos eran mayores, tenían mayor prevalencia de sexo masculino, factores de riesgo coronario así como un mayor Índice de Forma VI tele-diastólico y tele-sistólico. Después del emparejamiento, todas las características clínicas fueron comparables entre los pacientes diabéticos y no diabéticos, pero los pacientes diabéticos continuaron teniendo un mayor Índice de Forma VI al final de la sístole y diástole (p < 0.001). En el análisis de regresión lineal multivariable, la diabetes fue un fuerte predictor del Índice de Forma VI tele-sistólico en el total de la población de estudio y en la cohorte de propensión.
Conclusiones
Los pacientes diabéticos tienen mayores valores del Índice de Forma VI comparado con los pacientes no diabéticos incluso después de equilibrar las características mediante un análisis de puntaje de propensión. La evaluación de los Índices de Forma mediante gated SPECT pueden ser de utilidad para identificar de manera temprana el remodelado del ventrículo izquierdo en pacientes con diabetes.
Chinese Abstract
背景
糖尿病可诱导结构性和功能性的心脏病变, 并引起心衰。左心室 (LV) 形状是心脏几何结构的一个动态组成成分, 可影响心脏的收缩功能。然而, 对于无明显冠心病的糖尿病和非糖尿病病人, 尚无平衡冠心病风险因素后, 关于两者 LV 形状指数比较的报道。
方法
我们利用单光子发射计算机断层显像技术 (SPECT) 研究了 1168 名负荷心肌灌注显像正常, 且 LV 射血分数正常的病人。为了说明糖尿病与非糖尿病病人基线特征的不同, 我们建立了一个倾向评分匹配队列来比较临床变量、冠心病危险因素和负荷类型。
结果
匹配前, 糖尿病病人年龄较大, 男性比率和冠心病风险因素更多, 且收缩末期和舒张末期的 LV 形状指数更大; 匹配后, 糖尿病和非糖尿病病人的所有临床特征均无差异, 但糖尿病病人仍有较高的收缩末期和舒张末期 LV 形状指数 (p < 0.001)。多变量线性回归分析显示, 在所有研究对象及倾向评分匹配队列中, 糖尿病是收缩末期 LV 形状指数的一个强预测因子。
结论
利用倾向评分匹配临床特征后, 糖尿病较非糖尿病病人有较高的 LV 形状指数。门控 SPECT 测定 LV 形状指数, 可用于糖尿病病人早期 LV 重构的识别。
French Abstract
Contexte
La configuration du ventricule gauche (VG) est une composante dynamique importante du système cardio-vasculaire et sa géométrie influence sa fonction contractile. Le diabète sucré induit des altérations cardiaques structurelles et fonctionnelles qui peuvent induire une insuffisance cardiaque. Peu de données comparant la configuration du VG sont disponibles chez les patients diabétiques et non diabétiques sans maladie coronarienne manifeste.
Méthodes
Nous avons étudié 1,168 patients avec perfusion myocardique et éjection ventriculaire gauche normales obtenues par scintigraphie tomographique myocardique à émission de photons (gated SPECT). De manière à tenir compte des différences dans les caractéristiques de base des patients diabétiques et non diabétiques, les patients furent classifiés et analysés en fonction de leur facteurs de risque coronarien et du type d’épreuve d’effort subi.
Résultats
Avant correction pour facteur de risques et type d’épreuve d’effort, les patients diabétiques étaient plus âgés, avaient une plus grande prévalence masculine, des facteurs de risque coronariens plus important et des indices de configuration diastolique et systolique du VG superieures plus élevés que les patients non diabétiques. Après correction, l’ensemble des paramètres cliniques étaient comparables entre chez les patients diabétiques et non-diabétiques. Néanmoins les indices de configuration diastolique et systolique du VG restaient supérieurs (p < 0.001) chez les patients diabétiques. Après analyse de régression linéaire multivariée, le diabète s’avérait s’est avéré un indicateur important des indices de configuration diastolique et systolique du VG dans les groupes étudies avant et après correction.
Conclusions
Les indices de configuration systoliques et diastoliques du VG chez les patients diabétiques sont plus élevés que chez les patients non diabétiques. L’évaluation des indices de configuration du VG par SPECT peut être utile pour l’identification du remodelage précoce du VG chez les patients diabétiques.




Similar content being viewed by others
Abbreviations
- LV:
-
Left ventricular
- SPECT:
-
Single-photon emission computed tomography
- SI:
-
Shape index
- EF:
-
Ejection fraction
- CAD:
-
Coronary artery disease
References
Koitabashi N, Kass DA. Reverse remodeling in heart failure-mechanisms and therapeutic opportunities. Nat Rev Cardiol. 2011;9:147-57.
Heusch G, Libby P, Gersh B, Yellon D, Böhm M, Lopaschuk G, et al. Cardiovascular remodelling in coronary artery disease and heart failure. Lancet. 2014;383:1933-43.
Udelson JE. Left ventricular shape: the forgotten stepchild of remodeling parameters. JACC Heart Fail. 2017;5:179-81.
Levelt E, Mahmod M, Piechnik SK, Ariga R, Francis JM, Rodgers CT, et al. Relationship between left ventricular structural and metabolic remodeling in type 2 diabetes. Diabetes. 2016;65:44-52.
Chong CR, Clarke K, Levelt E. Metabolic remodeling in diabetic cardiomyopathy. Cardiovasc Res. 2017;113:422-30.
Walker AM, Patel PA, Rajwani A, Groves D, Denby C, Kearney L, et al. Diabetes mellitus is associated with adverse structural and functional cardiac remodelling in chronic heart failure with reduced ejection fraction. Diab Vasc Dis Res. 2016;13:331-40.
Germano G, Kavanagh PB, Waechter P, Areeda J, Van Kriekinge S, Sharir T, et al. A new algorithm for the quantitation of myocardial perfusion SPECT. I: Technical principles and reproducibility. J Nucl Med. 2000;41:712-9.
Abidov A, Slomka PJ, Nishina H, Hayes SW, Kang X, Yoda S, et al. Left ventricular shape index assessed by gated stress myocardial perfusion SPECT: Initial description of a new variable. J Nucl Cardiol. 2006;13:652-9.
Rosendorff C, Black HR, Cannon CP, Gersh BJ, Gore J, Izzo JL Jr, et al. Treatment of hypertension in the prevention and management of ischemic heart disease: a scientific statement from the American Heart Association Council for High Blood Pressure Research and the Councils on Clinical Cardiology and Epidemiology and Prevention. Circulation. 2007;115:2761-88.
Verberne HJ, Acampa W, Anagnostopoulos C, Ballinger J, Bengel F, De Bondt P, European Association of Nuclear Medicine (EANM), et al. EANM procedural guidelines for radionuclide myocardial perfusion imaging with SPECT and SPECT, CT: 2015 revision. Eur J Nucl Med Mol Imaging. 2015;2015(42):1929-40.
Petretta M, Acampa W, Evangelista L, Daniele S, Ferro A, Cuocolo A. Impact of inducible ischemia by stress SPECT (IDIS) investigators. Impact of inducible ischemia by stress SPECT in cardiac risk assessment in diabetic patients: Rationale and design of a prospective, multicenter trial. J Nucl Cardiol. 2008;15:100-4.
Acampa W, Petretta M, Evangelista L, Daniele S, Xhoxhi E, De Rimini ML, et al. Myocardial perfusion imaging and risk classification for coronary heart disease in diabetic patients. The IDIS study: A prospective, multicentre trial. Eur J Nucl Med Mol Imaging. 2012;39:387-95.
Akincioglu C, Berman DS, Nishina H, Kavanagh PB, Slomka PJ, Abidov A, et al. Assessment of diastolic function using 16-frame 99mtc-sestamibi gated myocardial perfusion SPECT: Normal values. J Nucl Med. 2005;46:1102-8.
Acampa W, Petretta M, Daniele S, Del Prete G, Assante R, Zampella E, et al. Incremental prognostic value of stress myocardial perfusion imaging in asymptomatic diabetic patients. Atherosclerosis. 2013;227:307-12.
Germano G, Kiat H, Kavanagh PB, Moriel M, Mazzanti M, Su HT, et al. Automatic quantification of ejection fraction from gated myocardial perfusion SPECT. J Nucl Med. 1995;36:2138-47.
Germano G, Berman DS. On the accuracy and reproducibility of quantitative gated myocardial perfusion SPECT. J Nucl Med. 1999;40:810-3.
Leuven E, Sianesi B. PSMATCH2: Stata module to perform full Mahalanobis and propensity score matching, common support graphing, and covariate imbalance testing. http://ideas.repec.org/c/boc/bocode/s432001.html, version 4.0.11, Oct. 22, 2014. Statistical Software Components (SSC), Boston College Department of Economics.
Austin PC. Balance diagnostics for comparing the distribution of baseline covariates between treatment groups in propensity-score matched samples. Stat Med. 2009;28:3083-107.
DiPrete TA, Gangl M. Assessing bias in the estimation of causal effects: Rosenbaum bounds on matching estimators and instrumental variables estimation with imperfect instruments. Sociol Methodol. 2004;34:271-310.
Hölscher ME, Bode C, Bugger H. Diabetic cardiomyopathy: does the type of diabetes matter? Int J Mol Sci. 2016;17:2036.
Lombardi C, Spigoni V, Gorga E, Dei Cas A. Novel insight into the dangerous connection between diabetes and heart failure. Herz. 2016;41:201-7.
Boudina S, Abel ED. Diabetic cardiomyopathy revisited. Circulation. 2007;115:3213-23.
An D, Rodrigues B. Role of changes in cardiac metabolism in development of diabetic cardiomyopathy. Am J Physiol Heart Circ Physiol. 2006;291:H1489-506.
Nichols GA, Gullion CM, Koro CE, Ephross SA, Brown JB. The incidence of congestive heart failure in type 2 diabetes: an update. Diab Care. 2004;27:1879-84.
Douglas PS, Morrow R, Ioli A, Reichek N. Left ventricular shape, afterload and survival in idiopathic dilated cardiomyopathy. J Am Coll Cardiol. 1989;13:311-5.
Maffessanti F, Caiani EG, Tamborini G, Muratori M, Sugeng L, Weinert L, et al. Serial changes in left ventricular shape following early mitral valve repair. Am J Cardiol. 2010;106:836-42.
St John Sutton M, Linde C, Gold MR, Abraham WT, Ghio S, Cerkvenik J, et al. Left ventricular architecture, long-term reverse remodeling, and clinical outcome in mild heart failure with cardiac resynchronization: results from the REVERSE trial. JACC Heart Fail. 2017;5:169-78.
Lorenzo-Almorós A, Tuñón J, Orejas M, Cortés M, Egido J, Lorenzo Ó. Diagnostic approaches for diabetic cardiomyopathy. Cardiovasc Diabetol. 2017;16:28.
Assante R, Acampa W, Zampella E, Arumugam P, Nappi C, Gaudieri V, et al. Coronary atherosclerotic burden vs. coronary vascular function in diabetic and nondiabetic patients with normal myocardial perfusion: A propensity score analysis. Eur J Nucl Med Mol Imaging. 2017;44(7):1129-35.
Ernande L, Rietzschel ER, Bergerot C, De Buyzere ML, Schnell F, Groisne L, et al. Impaired myocardial radial function in asymptomatic patients with type 2 diabetes mellitus: A speckle-tracking imaging study. J Am Soc Echocardiogr. 2010;23:1266-72.
Ernande L, Bergerot C, Girerd N, Thibault H, Davidsen ES, Gautier Pignon-Blanc P, et al. Longitudinal myocardial strain alteration is associated with left ventricular remodeling in asymptomatic patients with type 2 diabetes mellitus. J Am Soc Echocardiogr. 2014;27:479-88.
Gimelli A, Liga R, Clemente A, Marras G, Kusch A, Marzullo P. Left ventricular eccentricity index measured with SPECT myocardial perfusion imaging: An additional parameter of adverse cardiac remodeling. J Nucl Cardiol. 2017. doi:10.1007/s12350-017-0777-3.
Medrano-Gracia P, Cowan BR, Ambale-Venkatesh B, Bluemke DA, Eng J, Finn JP, et al. J Cardiovasc Magn Reson. 2014;16:56.
Heagerty AM, Aalkjaer C, Bund SJ, Korsgaard N, Mulvany MJ. Small artery structure in hypertension: Dual process of remodeling and growth. Hypertension. 1993;21:391-7.
Aquaro GD, Camastra G, Monti L, Lombardi M, Pepe A, Castelletti S, et al. Reference values of cardiac volumes, dimensions, and new functional parameters by MR: A multicenter, multivendor study. J Magn Reson Imaging. 2017;45:1055-67.
Muraru D, Badano LP, Peluso D, Dal Bianco L, Casablanca S, Kocabay G, et al. Comprehensive analysis of left ventricular geometry and function by three-dimensional echocardiography in healthy adults. J Am Soc Echocardiogr. 2013;26:618-28.
Disclosure
The authors have indicated that they have no financial conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
JNC thanks Erick Alexanderson MD, Carlos Guitar MD, and Diego Vences MD, UNAM, Mexico, for providing the Spanish abstract; Haipeng Tang MS, Zhixin Jiang MD, and Weihua Zhou PhD, for providing the Chinese abstract; and Jean-Luc Urbain, MD, PhD, CPE, Past President CANM, Chief Nuclear Medicine, Lebanon VAMC, PA, for providing the French abstract.
The authors of this article have provided a PowerPoint file, available for download at SpringerLink, which summarises the contents of the paper and is free for re-use at meetings and presentations. Search for the article DOI on SpringerLink.com
Electronic Supplementary Material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Nappi, C., Gaudieri, V., Acampa, W. et al. Comparison of left ventricular shape by gated SPECT imaging in diabetic and nondiabetic patients with normal myocardial perfusion: A propensity score analysis. J. Nucl. Cardiol. 25, 394–403 (2018). https://doi.org/10.1007/s12350-017-1009-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12350-017-1009-6