Abstract
Objectives
This paper describes a novel approach (same-patient processing, or SPP) aimed at improving left ventricular segmentation accuracy in patients with multiple SPECT studies, and evaluates its performance compared to conventional processing in a large population of 962 patients undergoing rest and stress electrocardiography-gated SPECT MPI, for a total of 5,772 image datasets (6 per patient).
Methods
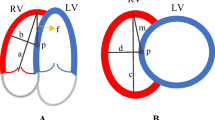
Each dataset was independently processed using a standard algorithm, and a shape quality control score (SQC) was produced for every segmentation. Datasets with a SQC score higher than a specific threshold, suggesting algorithmic failure, were automatically reprocessed with the SPP-modified algorithm, which incorporates knowledge of the segmentation mask location in the other datasets belonging to the same patient. Experienced operators blinded as to whether datasets had been processed based on the standard or SPP approach assessed segmentation success/failure for each dataset.
Results
The SPP approach reduced segmentation failures from 219/5772 (3.8%) to 42/5772 (0.7%) overall, with particular improvements in attenuation corrected (AC) datasets with high extra-cardiac activity (from 100/962 (10.4%) to 12/962 (1.4%) for rest AC, and from 41/962 (4.3%) to 9/962 (0.9%) for stress AC). The number of patients who had at least one of their 6 datasets affected by segmentation failure decreased from 141/962 (14.7%) to 14/962 (1.7%) using the SPP approach.
Conclusion
Whenever multiple image datasets for the same patient exist and need to be processed, it is possible to deal with the images as a group rather than individually. The same-patient processing approach can be implemented automatically, and may substantially reduce the need for manual reprocessing due to cardiac segmentation failure.



Similar content being viewed by others
Abbreviations
- SPP:
-
Same-patient processing
- SPECT:
-
Single photon emission computed tomography
- MPI:
-
Myocardial perfusion imaging
- LV:
-
Left ventricle
- AC:
-
Attenuation corrected
- SQC:
-
Shape quality control
References
Slomka PJ, Nishina H, Berman DS, Kang XP, Friedman JD, Hayes SW, et al. Automatic quantification of myocardial perfusion stress-rest change: A new measure of ischemia. J Nucl Med 2004;45:183–91.
Slomka PJ, Pan T, Berman DS, Germano G. Advances in SPECT and PET hardware. Progr Cardiovasc Dis 2015;57:566–78.
Einstein AJ, Pascual TNB, Mercuri M, Karthikeyan G, Vitola JV, Mahmarian JJ, et al. Current worldwide nuclear cardiology practices and radiation exposure: results from the 65 country IAEA Nuclear Cardiology Protocols Cross-Sectional Study (INCAPS). Eur Heart J 2015;36:1689–96.
Slomka PJ, Fish MB, Lorenzo S, Nishina H, Gerlach J, Berman DS, et al. Simplified normal limits and automated quantitative assessment for attenuation-corrected myocardial perfusion SPECT. J Nucl Cardiol 2006;13:642–51.
Germano G, Kavanagh PB, Chen J, Waechter P, Su HT, Kiat H, et al. Operator-less processing of myocardial perfusion SPECT studies. J Nucl Med 1995;36:2127–32.
Germano G, Kavanagh PB, Waechter P, Areeda J, Van Kriekinge S, Sharir T, et al. A new algorithm for the quantitation of myocardial perfusion SPECT. I: Technical principles and reproducibility. J Nucl Med 2000;41:712–9.
Xu Y, Kavanagh P, Fish M, Gerlach J, Ramesh A, Lemley M, et al. Automated quality control for segmentation of myocardial perfusion SPECT. J Nucl Med 2009;50:1418–26.
Arsanjani R, Xu Y, Hayes SW, Fish M, Lemley M, Gerlach J, et al. Comparison of fully automated computer analysis and visual scoring for detection of coronary artery disease from myocardial perfusion SPECT in a large population. J Nucl Med 2013;54:221–8.
Germano G, Kavanagh PB, Slomka PJ, Van Kriekinge SD, Pollard G, Berman DS. Quantitation in gated perfusion SPECT imaging: The Cedars-Sinai approach. J Nucl Cardiol 2007;14:433–54.
Garcia EV, Faber TL, Cooke CD, Folks RD, Chen J, Santana C. The increasing role of quantification in clinical nuclear cardiology: The Emory approach. J Nucl Cardiol 2007;14:420–32.
Ficaro EP, Lee BC, Kritzman JN, Corbett JR. Corridor4DM: The Michigan method for quantitative nuclear cardiology. J Nucl Cardiol 2007;14:455–65.
Germano G, Kavanagh PB, Su HT, Mazzanti M, Kiat H, Hachamovitch R, et al. Automatic reorientation of three-dimensional, transaxial myocardial perfusion SPECT images. J Nucl Med 1995;36:1107–14.
Germano G, Kiat H, Kavanagh PB, Moriel M, Mazzanti M, Su HT, et al. Automatic quantification of ejection fraction from gated myocardial perfusion SPECT. J Nucl Med 1995;36:2138–47.
Acknowledgments
This research was supported in part by Grant R01HL089765 from the National Heart, Lung, and Blood Institute/National Institutes of Health (NHLBI/NIH). Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the NHLBI/NIH.
Disclosure
Cedars-Sinai Medical Center receives royalties for the licensing of software and algorithms related to the quantitative assessment of perfusion, function and other cardiac parameters, a minority portion of which is distributed to some of the authors of this manuscript (Guido Germano, Paul B. Kavanagh, Daniel S. Berman and Piotr J. Slomka).
Author information
Authors and Affiliations
Corresponding author
Additional information
See related editorial, doi:10.1007/s12350-016-0703-0.
The authors of this article have provided a PowerPoint file, available for download at SpringerLink, which summarises the contents of the paper and is free for re-use at meetings and presentations. Search for the article DOI on SpringerLink.com.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Germano, G., Kavanagh, P.B., Fish, M.B. et al. “Same-Patient Processing” for multiple cardiac SPECT studies. 1. Improving LV segmentation accuracy. J. Nucl. Cardiol. 23, 1435–1441 (2016). https://doi.org/10.1007/s12350-016-0673-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12350-016-0673-2