Abstract
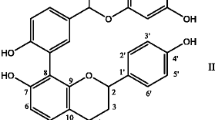
Clinical data suggest that people who use green tea have a lower cardiovascular risk. However, the exact mechanisms of these cardioprotective effects are unknown. We know that STAT1 plays a critical role in promoting apoptotic cell death and STAT3 may antagonise STAT1 and protect cardiac myocytes from ischaemia/reperfusion (I/R) injury. More recently it has been shown that specific molecules such as epigallocatechin-3-gallate (EGCG), which is present in green tea extract (GTE), have antioxidant properties. Considering that: (i) oxygen free radicals (OFR) are produced during myocardial I/R insult and (ii) OFR are responsible for reperfusion cardiac damage, we therefore investigated whether chronic administration per os of GTE reduced I/R damage in the Langendorff perfused isolated rat heart. In addition we evaluated myocardial content of STAT1 and STAT3 and degree of apoptosis. In Sprague-Dawley isolated hearts, GTE reduced the ischaemic mechanical insult, prolonged STAT3 activation/phosphorylation and reduced STAT1 activation with consequent less cell apoptosis. These results show that chronic treatment with GTE protects the heart from I/R injury. Activation of prosurvival STAT3 over the pro-apoptotic STAT1 could be one of the molecular mechanisms involved in green tea-mediated cardiopretection.
Similar content being viewed by others
References
Higton JV, Frei B (2003) Tea catechins and polyphenols: health effects, metabolism, and antioxidant function. Crit Rev Food Sci Nutr 43:89–143
Menegazzi M, Tedeschi E, Dussin D et al (2001) Anti-interferon gamma action of epigallocatechin-3-gallate mediated by specific inhibition of STAT1 activation. FASEB J 15:1309–1311
Scarabelli TM, Stephanou A, Pasini E et al (2002) Different signalling pathways induce apoptosis in endothelial cells and cardiac myocytes during ischaemia/reperfusion injury. Circ Res 90:745–748
Ferrari R, Cargnoni A, Bernocchi P et al (1996) Metabolic adaptation during a sequence of no-flow and low-flow ischemia: a possible trigger for hibernation. Circulation 94:2587–2596
Stephanou A, Brar BK, Scarabelli T et al (2000) Ischaemia-induced STAT-1 expression and activation plays a critical role in cardiac myocyte apoptosis. J Biol Chem 275:10002–10008
Stephanou A, Latchman DS (2005) Opposing actions of STAT-1 and STAT-3. Growth Factor 23:177–182
Stephanou A, Brar BK, Knight RA, Latchman DS (2000) Opposing actions of STAT-1 and STAT-3 on the Bcl-2 and Bcl-x promoters. Cell Death Differentiation 7:329–330
Stephanou A, Scarabelli T, Townsend PA et al (2002) The carboxyl-terminal activation domain of the STAT-1 transcription factor enhances ischaemia/reperfusion-induced apoptosis in cardiac myocytes. FASEB J 16:1841–1843
Stephanou A (2002) Activated STAT-1 pathway in the myocardium as a novel therapeutic target in ischaemia/reperfusion injury. European Cytokine Network 13:387–390
Stephanou A, Scarabelli T, Brar BK et al (2001) Induction of apoptosis and Fas/FasL expression by ischaemia/reperfusion in cardiac myocytes requires serine 727 of the STAT1 but not tyrosine 701. J Biol Chem 276:28340–28347
Menegazzi M, Tedeschi E, Dussin D et al (2001) Anti-interferon gamma action of epigallocatechin-3-gallate mediated by specific inhibition of STAT1 activation. FASEB J 15:1309–1311
Townsend PA, Scarabelli TM, Pasini E et al (2004) Epigallocatechin-3-gallate inhibits STAT-1 activation and protects cardiac myocytes from ischemia/reperfusion-induced apoptosis. FASEB J 18:1621–1623
Roth E (1998) The impact of L-arginine-nitric oxide metabolism on ischaemia/reperfusion injury. Curr Opin Clin Nutr Metab Care 1:97–99
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Pasini, E., Stephanou, A., Scarabelli, C.C. et al. Possible molecular basis of cardioprotective effects of green tea. Mediterr J Nutr Metab 2, 15–19 (2009). https://doi.org/10.1007/s12349-009-0036-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12349-009-0036-8