Abstract
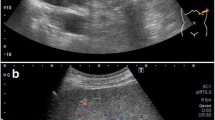
Xanthogranulomatous inflammation is a chronic inflammatory reaction microscopically characterized by aggregation of foamy histiocytes, fibrous tissue, and infiltration of various inflammatory cells. In contrast to xanthogranulomatous inflammation in the gallbladder or kidney, xanthogranulomatous pancreatitis is rare. We herein present a case of xanthogranulomatous pancreatitis in a patient who underwent distal pancreatectomy with splenectomy under preoperative suspicion of a pancreatic pseudocyst or pancreatic tumor. A 77-year-old woman with a 1 month history of epigastric pain, anorexia, and general fatigue was admitted to our hospital. Contrast-enhanced computed tomography revealed a cystic mass with ill-defined margins at the pancreatic tail together with a splenic abscess. Contrast-enhanced endoscopic ultrasound detected a hyperechoic cystic lesion at the tail of the pancreas with heterogeneous internal echogenicity, and part of the intra-cystic content was enhanced by the contrast agent. Endoscopic retrograde cholangiopancreatography showed a cystic lesion at the tail of the pancreas that continued into the main pancreatic duct, and the main pancreatic duct was slightly narrowed downstream of the cystic lesion. Pancreatic juice cytology revealed suspicious cells, leading to the possibility of intraductal papillary mucinous carcinoma. Distal pancreatectomy with splenectomy was performed, and the histopathological diagnosis was xanthogranulomatous pancreatitis with no malignant findings.







Similar content being viewed by others
References
Ueno T, Hamanaka Y, Nishihara K, Nishida M, Nishikawa M, Kawabata A, et al. Xanthogranulomatous change appearing in the pancreas cyst wall. Pancreas. 1993;8:649–51.
Houston JP, Collins MC, Cameron I, Reed MW, Parsons MA, Roberts KM. Xanthogranulomatous cholecystitis. Br J Surg. 1994;81:1030–2.
Kim PN, Lee SH, Gong GY, Kim JG, Ha HK, Lee YJ, et al. Xanthogranulomatous cholecystitis: radiologic findings with histologic correlation that focuses on intramural nodules. Am J Roentgenol. 1999;172:949–53.
Cozzutto C, Carbone A. The xanthogranulomatous process. Xanthogranulomatous inflammation Pathol Res Pract. 1988;183:395–402.
Guzmán-Valdivia G. Xanthogranulomatous cholecystitis: 15 years’ experience. World J Surg. 2004;28:254–7.
Nakatani T, Uchida J, Iwai T, Yoshida N, Kuratsukuri K, Takemoto Y, et al. Xanthogranulomatous pyelonephritis with acquired cystic disease of the kidney in a haemodialysis patient. Nephrology. 2003;8:101–3.
Antonakopoulos GN, Chapple CR, Newman J, Crocker J, Tudway DC, O’Brien JM, et al. Xanthogranulomatous pyelonephritis. A reappraisal and immunohistochemical study. Arch Pathol Lab Med. 1988;112:275–81.
Koo JS, Jung W. Xanthogranulomatous mastitis: clinicopathology and pathological implications. Pathol Int. 2009;59:234–40.
Kubosawa H, Yano K, Oda K, Shiobara M, Ando K, Nunomura M, Aarashina H. Xanthogranulomatous gastritis with pseudosarcomatous changes. Pathol Int. 2007;57:291–5.
Oh YH, Seong SS, Jang KS, Chung YW, Paik CH, Park YW, et al. Xanthogranulomatous inflammation presenting as a submucosal mass of the sigmoid colon. Pathol Int. 2005;55:440–4.
Iyer VK, Aggarwal S, Mathur M. Xanthogranulomatous pancreatitis: mass lesion of the pancreas simulating pancreatic carcinoma—a report of two cases. Indian J Pathol Microbiol. 2004;47:36–8.
Kamitani T, Nishimiya M, Takahashi N, Shida Y, Hasuo K, Koizuka H. Xanthogranulomatous pancreatitis associated with intraductal papillarymucinous tumor. AJR Am J Roentgenol. 2005;185:704–7.
Okabayashi T, Nishimori I, Kobayashi M, Sugimoto T, Kohsaki T, Okamoto K, et al. Xanthogranulomatous pancreatic abscess secondary to acute pancreatitis: two case reports. Hepatogastroenterology. 2007;54:1648–51.
Shima Y, Saisaka Y, Furukita Y, Nishimura T, Horimi T, Nakamura T, et al. Resected xanthogranulomatous pancreatitis. J Hepatobiliary Pancreat Surg. 2008;15:240–2.
Iso Y, Tagaya N, Kita J, Sawada T, Kubota K. Xanthogranulomatous lesion of the pancreas mimicking pancreatic cancer. Med Sci Monit. 2008;14:130–3.
Ikeura T, Takaoka M, Shimatani M, Koyabu M, Kusuda T, Suzuki R, et al. Xanthogranulomatous inflammation of the peripancreatic region mimicking pancreatic cystic neoplasm. Intern Med. 2009;48:1881–4.
Kim YN, Park SY, Kim YK, Moon WS. Xanthogranulomatous pancreatitis combined with intraductal papillary mucinous carcinoma in situ. J Korean Med Sci. 2010;25:1814–7.
Uguz A, Yakan S, Gurcu B, Yilmaz F, Ilter T, Coker A. Xanthogranulomatous pancreatitis treated by duodenum-preserving pancreatic head resection. Hepatobiliary Pancreat Dis Int. 2010;9:216–8.
Nishimura M, Nishihira T, Hirose T, Ishikawa Y, Yamaoka R, Inoue H, et al. Xanthogranulomatous pancreatitis mimicking a malignant cystic tumour of the pancreas: report of a case. Surg Today. 2011;41:1310–3.
Kim HS, Joo M, Chang SH, Song HY, Song TJ, Seo JW, et al. Xanthogranulomatous pancreatitis presents as a solid tumour mass: a case report. J Korean Med Sci. 2011;26:583–6.
Hanna T, Abdul-Rahman Z, Greenhalf W, Farooq A, Neoptolemos JP. Xanthogranulomatous pancreatitis associated with a mucinous cystic neoplasm. Pathol Int. 2016;66:174–6.
Atreyapurapu V, Keshwani A, Lingadakai R, Pai K. Xanthogranulomatous pancreatitis mimicking a malignant solid tumour. BMJ Case Rep. 2016. https://doi.org/10.1136/bcr-2015-209934.
Hyung JK. Xanthogranulomatous pancreatitis mimicking potentially malignant pancreatic neoplasm: report of a case. Ann Hepatobiliary Pancreat Surg. 2017;21:243–6.
Choi YH, Choi WH, Han SY, Han KH, Kim HS. A case of bilateral xanthogranulomatous pyelonephritis with renal failure. Korean J Nephrol. 2008;27:137–40.
Acknowledgements
This study was supported by a Grant-in-Aid for Research Activity Start-up (19K24012) and a Grant-in-Aid for Scientific Research C (22K08749) (to K.N.) from the Ministry of Education, Culture, Science and Sports, Japan. The authors thank Angela Morben, DVM, ELS, from Edanz (https://jp.edanz.com/ac) for editing a draft of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Keiji Nagata, Kojiro Nakamura, Taku Iida, Junji Iwasaki, Ryo Ito, Satsuki Asai, Misa Ishihara, Toshiyuki Hata, Atsushi Itami, and Takahisa Kyogoku declare that they have no conflict of interest.
Ethical approval
All procedures followed were in accordance with the ethical standards of the responsible committees on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008(5).
Informed consent
Informed consent was obtained from the patient described in this report.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Nagata, K., Nakamura, K., Iida, T. et al. A case of progressive xanthogranulomatous pancreatitis with splenic abscess. Clin J Gastroenterol (2024). https://doi.org/10.1007/s12328-024-01930-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12328-024-01930-1