Abstract
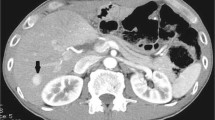
Hepatocellular adenomas are rare diseases, defined as benign liver neoplasms composed of cells with hepatocellular differentiation. Differential diagnosis of hepatocellular adenoma from other lesions, including focal nodular hyperplasia and hepatocellular carcinoma, is crucial to determine treatment strategy. We describe a case of β-catenin-activated inflammatory hepatocellular adenoma with malignant transformation. A 50-year-old man with a suspected liver tumor, based on abdominal ultrasonography findings, was referred to our hospital. Contrast-enhanced computed tomography and magnetic resonance imaging revealed a liver tumor in S2 which was enhanced in the arterial phase to the delayed phase. Based on diagnostic imaging findings, hepatocellular adenoma or focal nodular hyperplasia was suspected. We considered the possibility of malignant potential because of the enlargement of the lesion. Thus, we performed a laparoscopic hepatectomy. Histological examination showed pigment deposition in the hepatocytes, which was determined to be lipofuscin. Mild nuclear swelling and atypia in the tumor area indicated nodular growth. Based on the histological and immunohistochemical findings, the diagnosis was ꞵ-catenin-activated inflammatory hepatocellular adenoma with atypical features. The imaging features of hepatocellular adenoma and focal nodular hyperplasia are similar, but if the tumor tends to grow, surgical treatment should be performed because of the possibility of malignant hepatocellular adenoma.






Similar content being viewed by others
Data availability
All data generated or analyzed during this study are included in this article.
Abbreviations
- AFP:
-
α-Fetoprotein
- b-HCA:
-
ꞵ-Catenin-activated hepatocellular adenoma
- b-IHCA:
-
β-Catenin-activated inflammatory hepatocellular adenoma
- CRP:
-
C-reactive protein
- CT:
-
Computed tomography
- FNH:
-
Focal nodular hyperplasia
- Gd-EOB-DTPA:
-
Gadolinium ethoxybenzyl diethylenetriamine pentaacetic acid
- GS:
-
Glutamine synthetase
- HCA:
-
Hepatocellular adenoma
- HCC:
-
Hepatocellular carcinoma
- HNF1a:
-
Hepatocyte nuclear factor 1a
- H-HCA:
-
HNF1A-inactivated hepatocellular adenoma
- IHCA:
-
Inflammatory hepatocellular adenoma
- MRI:
-
Magnetic resonance imaging
- OATP:
-
Organic anion transporting polypeptide
- SAA:
-
Serum amyloid A
References
Paradis V, Fukayama M, Park YN, et al. WHO classification of tumours of the digestive system. 8. Tumours of the liver and intrahepatic bile ducts. 5th ed. Geneva: World Health Organization; 2019.
Micchelli STL, Vivekanandan P, Boitnott JK, et al. Malignant transformation of hepatic adenomas. Mod Pathol. 2008;21:491–7.
Dokmak S, Paradis V, Vilgrain V, et al. A single-center surgical experience of 122 patients with single and multiple hepatocellular adenomas. Gastroenterology. 2009;137:1698–705.
Sempoux C, Balabaud C, Bioulac-Sage P. Malignant transformation of hepatocellular adenoma. Hepat Oncol. 2014;1:421–31.
Coelho R, Gonçalves R, Carneiro F, et al. Pigmented hepatocellular adenoma with β-catenin activation: case report and literature review. Ann Hepatol. 2016;15:598–603.
Mounajjed T, Yasir S, Aleff PA, et al. Pigmented hepatocellular adenomas have a high risk of atypia and malignancy. Mod Pathol. 2015;28:1265–74.
Hechtman JF, Raoufi M, Fiel MI, et al. Hepatocellular carcinoma arising in a pigmented telangiectatic adenoma with nuclear β-catenin and glutamine synthetase positivity: case report and review of the literature. Am J Surg Pathol. 2011;35:927–32.
Guo Y, Li W, Cai W, et al. Diagnostic value of gadoxetic acid-enhanced MR imaging to distinguish HCA and its subtype from FNH: a systematic review. Int J Med Sci. 2017;14:668–74.
Rooks JB, Ory HW, Ishak KG, et al. Epidemiology of hepatocellular adenoma. The role of oral contraceptive use. JAMA. 1979;242:644–8.
Edmondson HA, Henderson B, Benton B. Liver-cell adenomas associated with use of oral contraceptives. N Engl J Med. 1976;294:470–2.
Cohen C, Lawson D, DeRose PB. Sex and androgenic steroid receptor expression in hepatic adenomas. Hum Pathol. 1998;29:1428–32.
Chang CY, Hernandez-Prera JC, Roayaie S, et al. Changing epidemiology of hepatocellular adenoma in the United States: review of the literature. Int J Hepatol. 2013;2013: 604860.
Singal AG, Lampertico P, Nahon P. Epidemiology and surveillance for hepatocellular carcinoma: new trends. J Hepatol. 2020;72:250–61.
Sasaki M, Yoneda N, Sawai Y, et al. Clinicopathological characteristics of serum amyloid A-positive hepatocellular neoplasms/nodules arising in alcoholic cirrhosis. Histopathology. 2015;66:836–45.
Calderaro J, Nault JC, Balabaud C, et al. Inflammatory hepatocellular adenomas developed in the setting of chronic liver disease and cirrhosis. Mod Pathol. 2016;29:43–50.
Rebouissou S, Franconi A, Calderaro J, et al. Genotype-phenotype correlation of CTNNB1 mutations reveals different ß-catenin activity associated with liver tumor progression. Hepatology. 2016;64:2047–61.
Brancatelli G, Federle MP, Vullierme MP, et al. CT and MR imaging evaluation of hepatic adenoma. J Comput Assist Tomogr. 2006;30:745–50.
Agrawal S, Agarwal S, Arnason T, et al. Management of hepatocellular adenoma: recent advances. Clin Gastroenterol Hepatol. 2015;13:1221–30.
Nault JC, Bioulac-Sage P, Zucman-Rossi J. Hepatocellular benign tumors-from molecular classification to personalized clinical care. Gastroenterology. 2013;144:888–902.
Bilreiro C, Soler JC, Ayuso JR, et al. Diagnostic value of morphological enhancement patterns in the hepatobiliary phase of gadoxetic acid-enhanced MRI to distinguish focal nodular hyperplasia from hepatocellular adenoma. Radiol Med (Torino). 2021;126:1379–87.
Auer TA, Walter-Rittel T, Geisel D, et al. HBP-enhancing hepatocellular adenomas and how to discriminate them from FNH in Gd-EOB MRI. BMC Med Imaging. 2021;21:21–8.
Reizine E, Amaddeo G, Pigneur F, et al. Quantitative correlation between uptake of Gd-BOPTA on hepatobiliary phase and tumor molecular features in patients with benign hepatocellular lesions. Eur Radiol. 2018;28:4243–53.
Acknowledgements
We would like to thank Dr. Yasuni Nakanuma at Fukui Saiseikai Hospital (Fukui, Japan) and all staff members at Aomori City Hospital (Aomori, Japan) for their contribution to this report.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
YW wrote the manuscript. YT managed the clinical practice and authored the case study. TK supervised the pathological examinations in the study. YK, TO, HJ, MN, KA, and HK provided advice on the manuscript. YT and ME supervised the clinical practice.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no competing interests to declare.
Human and animal rights
This case report was conducted in accordance with the Declaration of Helsinki. The Aomori City Hospital Ethics Committee (Aomori, Japan) approved the study protocol.
Informed consent
The patient provided consent for this case report to be published.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wakasa, Y., Toyoki, Y., Kusumi, T. et al. β-Catenin-activated inflammatory hepatocellular adenoma with pigmentation and atypical features: a case report. Clin J Gastroenterol 16, 237–243 (2023). https://doi.org/10.1007/s12328-023-01757-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12328-023-01757-2