Abstract
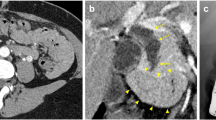
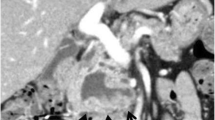
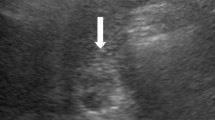
An 82-year-old woman who had been suffering from repeated obstructive jaundice for 7 years was referred to our hospital. Although endoscopic aspiration of the mucin in the common bile duct had been temporally effective, origin of the mucin production had not been detectable. The patient thus had been forced to be on long-term follow-up without curative resection. Endoscopic retrograde cholangioscopy on admission revealed massive mucin in the common bile duct. In addition, an anomalous bile duct located proximal to the gallbladder was identified. Since the lumen of the anomalous duct was irregular and the rest of biliary tree was completely free of suspicious lesions, the anomalous duct was judged to be the primary site. Surgical resection of the segment 4 and 5 of the liver combined with the extrahepatic biliary tract was performed. Pathological diagnosis was compatible to intraductal papillary neoplasm with high-grade intraepithelial dysplasia of the anomalous bile duct. The patient has been free from the disease for 6.5 years after resection. This is the first case of intraductal papillary neoplasm derived from an anomalous bile duct, which was resected after long-term conservative treatment. The present case suggested the slow growing character of natural history of the neoplasm.



Similar content being viewed by others
Abbreviations
- IPNB:
-
Intraductal papillary neoplasm of the biliary duct
- WHO:
-
World Health Organization
- IPMN-P:
-
Intraductal papillary neoplasm of the pancreas
References
Chen TC, Nakanuma Y, Zen Y, et al. Intraductal papillary neoplasms of the liver associated with heaptolithiasis. Hepatology. 2001;34:651–8.
Nakanuma Y, Curado M-P, Franceschi S, et al., editors. WHO classifyion of tumours of the digestive system. 4th ed. Lyon: WHO; 2010. p. 217–24.
Kubota K, Nakanuma Y, Kondo F, et al. Clinicopathological features and prognosis of mucin-producing bile duct tumor and mucinous cystic tumor of the liver: a multi-institutional study by the Japan Biliary Association. J Hepato-Biliary-Pancreat Sci. 2014;21:176–85.
Gordon-Weeks AN, Jones K, Harriss E, et al. Systematic review and meta-analysis of current experience in treating IPNB: clinical and pathological correlates. Ann Surg. 2016;263(4):656–63.
Yeh T, Tseng J, Chiu C, et al. Cholangiographic spectrum of intraductal papillary mucinous neoplasm of the bile ducts. Ann Surg. 2006;244:248–53.
Kim H, Kim M, Lee S, et al. Mucin-hypersecreting bile duct tumor characterized by a striking homology with an intraductal papillary mucinous tumor (IPMT) of the pancreas. Endoscopy. 2000;32:389–93.
Nakanuma Y, Zen Y, Harada K, et al. Tumorigenesis and phenotypic characteristics of mucin-producing bile duct tumors: an immunohistochemical approach. J Hepatobiliary Pancreat Sci. 2010;17:211–22.
Zen Y, Fujii T, Itatsu K, et al. Biliary papillary tumors share pathological features with intraductal papillary mucinous neoplasm of the pancreas. Hepatology. 2006;44:1333–43.
Rizzo R, Szucs R, Turner M. Congenital abnormalities of the pancreas and biliary tree in adults. Radiographics. 1995;15:49–68 (quiz 147-8).
Horaguchi J, Fujita N, Noda Y, et al. Choledochocele associated with superficial spreading cancer with cholesterolosis of the bile duct. J Gastroenterol. 2007;42:318–24.
Chirica M, Vullierme M, Sibert A, et al. Major hepatectomy for peripheral papillary cholangiocarcinoma with hilar extension in a patient with situs ambiguous. Gastroenterol Clin Biol. 2005;29:456–60.
Stanton R, Craig P, Jorgensen J, et al. Leakage via aberrant bile duct due to cholangiocarcinoma. HPB Surg. 1998;11:125–8.
Schenk E, Findlay CJ. Intrahepatic duct system anomaly and hepatic duct carcinoma. Arch Pathol. 1963;75:453–8.
Akiyama H, Kazitani T, Kuroda Y, et al. Bile duct carcinoma associated with an anomaly in the bile duct. Helv Chir Acta. 1979;45:813–6.
Kagawa Y, Kashihara S, Kuramoto S, et al. Carcinoma arising in a congenitally dilated biliary tract. Report of a case and review of the literature. Gastroenterology. 1978;74:1286–94.
Acknowledgements
The authors thank Rumi Hino, Tetsuo Ushiku, and Masashi Fukayama at Department of Pathology, Graduate School of Medicine, The University of Tokyo, for their kind advice for histological diagnosis of the present case.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest:
All the authors declare that they have no conflict of interests.
Human/Animal Rights:
All procedures followed have been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments.
Informed Consent:
Written informed consent was obtained from the patient for publication of this Case report and any accompanying images.
Rights and permissions
About this article
Cite this article
Maki, H., Aoki, T., Ishizawa, T. et al. Intraductal papillary neoplasm originating from an anomalous bile duct. Clin J Gastroenterol 10, 174–178 (2017). https://doi.org/10.1007/s12328-017-0721-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12328-017-0721-8