Abstract
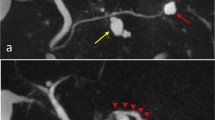
We report a rare case of an intraductal papillary mucinous neoplasm (IPMN) with a pancreatobiliary-type carcinoma in situ (CIS) that originated around a mural nodule formed in a gastric-type adenoma. A 64-year-old man was admitted to our hospital in December 2001 for dilation of the main pancreatic duct, detected on abdominal ultrasonography. Branch-duct-type IPMN (diameter 25 mm) was diagnosed, and because mural nodules were absent, the patient was annually followed up for 5 years. In 2006, computed tomography scans revealed thickening of the tumor wall and the development of a mural nodule (diameter approximately 6 mm); pancreatoduodenectomy with regional lymph-node dissection was performed. Histopathologic examination showed an intraductal papillary mucinous carcinoma arising from an adenoma. Hematoxylin and eosin (H&E) staining revealed that most of the tumor components, including the mural nodule, had adenomatous changes, indicating the tumor to be of the gastric type; however, immunohistochemistry showed positive MUC2 expression. Histologically, the tissues around the nodule, including those showing a cribriform pattern, were diagnosed as CIS. These tissues were classified as the pancreatobiliary-type on the basis of the results of both H&E staining and immunohistochemistry. The patient remained disease-free for 3 years after surgery.





Similar content being viewed by others
References
Kimura W, Kuroda A, Makuuchi M. Problems in the diagnosis and treatment of a so-called mucin-producing tumor of the pancreas. Pancreas. 1998;16:363–9.
Salvia R, Crippa S, Falconi M, Bassi C, Guarise A, Scapra A, et al. Branch-duct intraductal papillary mucinous neoplasms of the pancreas: to operate or not to operate? Gut. 2007;56:1086–90.
Jang JY, Kim SW, Lee SE, Yang SH, Lee UK, Lee YJ, et al. Treatment guidelines for branch duct type intraductal papillary mucinous neoplasms of the pancreas: when can we operate or observe? Ann Surg Oncol. 2008;15:199–205.
Kimura W, Makuuchi M. Operative indications for cystic lesions of the pancreas with malignant potential−our experience. Hepatogastroenterology. 1999;46:483–91.
Tanaka M, Chari S, Adsay V, Castillo CF, Falconi M, Shimizu M, et al. International consensus guidelines for management of intraductal papillary mucinous neoplasms and mucinous cystic neoplasms of the pancreas. Pancreatology. 2006;6:17–32.
Sugiyama M, Izumisato Y, Abe N, Masaki T, Mori T, Atomi Y. Predictive factors for malignancy in intraductal papillary-mucinous tumors of the pancreas. Br J Surg. 2003;90:1244–9.
Furukawa T, Gunter K, Adsay NV, Albores-Saavedra J, Fukushima N, Horii A, et al. Classification of types of intraductal papillary-mucinous neoplasm of the pancreas: consensus study. Virchows Arch. 2005;447:794–9.
Sanada Y, Kunita K, Yoshida K. Comparison of histologic subtype and growth pattern in intraductal papillary-mucinous carcinoma of the pancreas. Oncol Rep. 2008;19:1435–43.
Nakamura A, Horinouchi M, Goto M, Nagata K, Sakoda K, Takao S, et al. New classification of pancreatic intraductal papillary-mucinous tumour by mucin expression: its relationship with potential for malignancy. J Pathol. 2002;197:201–10.
Ban S, Naitoh Y, Ogawa F, Shimizu Y, Shimizu M, Yasumoto A, et al. Intraductal papillary mucinous neoplasm (IPMN) of the gastric-type with focal nodular growth of the arborizing papillae: a case of high-grade transformation of the gastric-type IPMN. Virchows Arch. 2006;449:112–6.
Yonezawa S, Nakamura A, Horinouchi M, Sato E. The expression of several types of mucin is related to the biological behavior of pancreatic neoplasms. J Hepatobiliary Pancreat Surg. 2002;9:328–41.
Adsay NV, Merati K, Basturk O, Iacobuzio-Donahue C, Levi E, Cheng JD, et al. Pathologically and biologically distinct types of epithelium in intraductal papillary mucinous neoplasm: delineation of an “intestinal” pathway of carcinogenesis. Am J Surg Pathol. 2004;28:839–48.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Takasu, N., Kimura, W., Moriya, T. et al. A pancreatobiliary-type carcinoma in situ at the periphery of a mural nodule developed from a gastric adenoma in an intraductal papillary mucinous neoplasm. Clin J Gastroenterol 3, 209–213 (2010). https://doi.org/10.1007/s12328-010-0162-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12328-010-0162-0