Abstract
Introduction
Exogenous gonadotropin (Gn) is given to regulate follicle-stimulating hormone (FSH) levels to achieve optimal ovarian response in in vitro fertilization/intracytoplasmic sperm injection (IVF/ICSI). The objective of this study was to analyze the optimal degree of change in FSH blood concentration with ovarian responsiveness in a short-acting gonadotropin-releasing hormone agonist (GnRH-a) long protocol for IVF/ICSI.
Methods
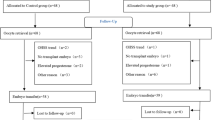
This retrospective study was conducted at Changzhou Maternity and Child Health Hospital's Reproductive Center from May 2017 to May 2023. A total of 794 ovarian stimulation cycles for IVF/ICSI using the short-acting GnRH-a long protocol was included. Ovarian responsiveness was assessed based on the number of follicles > 14 mm on human chorionic gonadotropin (HCG) trigger day, refine-follicular output rate (Refine-FORT) and good quality embryos. Delta 1 referred to the change in FSH level between days 6–8 of gonadotropin usage and baseline FSH, while Delta 2 referred to the change in FSH level between HCG trigger day and days 6–8 of gonadotropin usage. Simple and multiple linear regression analysis were performed to adjust for confounding factors.
Results
The number of follicles > 14 mm on HCG trigger day was found to be the most suitable indicator for evaluating ovarian responsiveness compared to the number of follicles > 16 mm and the number of retrieved oocytes. When Delta 1 ranged from 1.94 to 3.37, the number of follicles > 14 mm on HCG trigger day was the highest. When Delta 1 ranged from 3.37 to 5.90, the Refine-FORT was the highest. However, when Delta 1 exceeded 5.90, the number of follicles > 14 mm on HCG trigger day, Refine-FORT and good quality embryo all significantly decreased. On the other hand, when Delta 2 was ≤ − 1.58, the number of follicles > 14 mm on HCG trigger day and the Refine-FORT were both the highest.
Conclusion
This study identifies optimal Delta 1 and Delta 2 ranges for effective ovarian responsiveness in a short-acting GnRH-a long protocol for IVF/ICSI and introduces the novel measure of the number of follicles > 14 mm on HCG trigger day. The optimal range for Delta 1 was 1.94 to 3.37, and Delta 2 should be < − 1.58 for achieving a higher number and quality of oocytes.



Similar content being viewed by others
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request. Renjie Lu, Email: renjie_lu@126.com.
References
Coss D. Regulation of reproduction via tight control of gonadotropin hormone levels. Mol Cell Endocrinol. 2018;463:116–30.
Vegetti W, Alagna F. FSH and folliculogenesis: from physiology to ovarian stimulation. Reprod Biomed Online. 2006;12(6):684–94.
McGee EA, Hsueh AJ. Initial and cyclic recruitment of ovarian follicles. Endocr Rev. 2000;21(2):200–14.
Kubota T. Update in polycystic ovary syndrome: new criteria of diagnosis and treatment in Japan. Reprod Med Biol. 2013;12(3):71–7.
Lekamge DN, et al. Increased gonadotrophin stimulation does not improve IVF outcomes in patients with predicted poor ovarian reserve. J Assist Reprod Genet. 2008;25(11–12):515–21.
Hu L, et al. The relationship between Serum Delta FSH level and ovarian response in IVF/ICSI Cycles. Front Endocrinol (Lausanne). 2020;11: 536100.
Sunkara SK, et al. Association between the number of eggs and live birth in IVF treatment: an analysis of 400,135 treatment cycles. Hum Reprod. 2011;26(7):1768–74.
Goverde AJ, et al. Ovarian response to standard gonadotrophin stimulation for IVF is decreased not only in older but also in younger women in couples with idiopathic and male subfertility. Hum Reprod. 2005;20(6):1573–7.
McCulloh DH, et al. Follicle size indicates oocyte maturity and blastocyst formation but not blastocyst euploidy following controlled ovarian hyperstimulation of oocyte donors. Hum Reprod. 2020;35(3):545–56.
Wirleitner B, et al. Relationship between follicular volume and oocyte competence, blastocyst development and live-birth rate: optimal follicle size for oocyte retrieval. Ultrasound Obstet Gynecol. 2018;51(1):118–25.
Bergh C, et al. Comparison of fertilization, cleavage and pregnancy rates of oocytes from large and small follicles. Hum Reprod. 1998;13(7):1912–5.
Wang Y, et al. Causes and effects of oocyte retrieval difficulties: a retrospective study of 10,624 cycles. Front Endocrinol (Lausanne). 2021;12: 564344.
Findlay JK, et al. How is the number of primordial follicles in the ovarian reserve established? Biol Reprod. 2015;93(5):111.
Solernou R, et al. The Follicular Output Rate (FORT) as a method to evaluate transdermal testosterone efficacy in poor responders. JBRA Assist Reprod. 2021;25(2):229–34.
Grynberg M, Labrosse J. Understanding Follicular Output Rate (FORT) and its implications for POSEIDON criteria. Front Endocrinol (Lausanne). 2019;10:246.
Genro VK, et al. Frequent polymorphisms of FSH receptor do not influence antral follicle responsiveness to follicle-stimulating hormone administration as assessed by the Follicular Output RaTe (FORT). J Assist Reprod Genet. 2012;29(7):657–63.
Rodríguez-Fuentes A, et al. Volume-based follicular output rate improves prediction of the number of mature oocytes: a prospective comparative study. Fertil Steril. 2022;118(5):885–92.
Alviggi C, Esteves SC, Conforti A. Ovarian reserve tests: Are they only a quantitative measure? Fertil Steril. 2020;113(4):761–2.
Fleming R, et al. Assessing ovarian response: antral follicle count versus anti-Müllerian hormone. Reprod Biomed Online. 2015;31(4):486–96.
Shrikhande L, Shrikhande B, Shrikhande A. AMH and its clinical implications. J Obstet Gynaecol India. 2020;70(5):337–41.
Moolhuijsen LME, Visser JA. Anti-Müllerian hormone and ovarian reserve: update on assessing ovarian function. J Clin Endocrinol Metab. 2020;105(11):3361–73.
Steward RG, et al. Oocyte number as a predictor for ovarian hyperstimulation syndrome and live birth: an analysis of 256,381 in vitro fertilization cycles. Fertil Steril. 2014;101(4):967–73.
Ji J, et al. The optimum number of oocytes in IVF treatment: an analysis of 2455 cycles in China. Hum Reprod. 2013;28(10):2728–34.
Broekmans FJ, et al. A systematic review of tests predicting ovarian reserve and IVF outcome. Hum Reprod Update. 2006;12(6):685–718.
Sermondade N, et al. Serum antimüllerian hormone is associated with the number of oocytes matured in vitro and with primordial follicle density in candidates for fertility preservation. Fertil Steril. 2019;111(2):357–62.
Ben-Rafael Z, Levy T, Schoemaker J. Pharmacokinetics of follicle-stimulating hormone: clinical significance. Fertil Steril. 1995;63(4):689–700.
Sun PP, et al. The relationship between serum FSH level and ovarian response during controlled ovarian stimulation. Ginekol Pol. 2023;94(6):470–5.
Oudshoorn SC, et al. Ovarian response to controlled ovarian hyperstimulation: what does serum FSH say? Hum Reprod. 2017;32(8):1701–9.
Ahmed-Ebbiary NA, Lenton EA, Cooke ID. Hypothalamic-pituitary ageing: progressive increase in FSH and LH concentrations throughout the reproductive life in regularly menstruating women. Clin Endocrinol (Oxf). 1994;41(2):199–206.
Fatemi H, et al. Dose adjustment of follicle-stimulating hormone (FSH) during ovarian stimulation as part of medically-assisted reproduction in clinical studies: a systematic review covering 10 years (2007–2017). Reprod Biol Endocrinol. 2021;19(1):68.
Gerber RS, et al. Differential impact of controlled ovarian hyperstimulation on live birth rate in fresh versus frozen embryo transfer cycles: a Society for Assisted Reproductive Technology Clinic Outcome System study. Fertil Steril. 2020;114(6):1225–31.
Qiu Q, et al. Does an FSH surge at the time of hCG trigger improve IVF/ICSI outcomes? A randomized, double-blinded, placebo-controlled study. Hum Reprod. 2020;35(6):1411–20.
Thanking Patient Participants
We thank the participants of the study.
Funding
Funding for the Rapid Service Fee was provided by Changzhou Maternity and Child Health Care Hospital (Changzhou, Jiangsu, China). This work was supported by National Key R&D Program “Fertility Health and Health Security for Women and Children”: Clinical Cohort and Intervention Study on Genetic Problems in Assisted Reproduction Offspring (2021YFC2700602); Hospital management innovation research project of Jiangsu Hospital Association in 2023 (JSYGY-3-2023-247); the special project of soft science research of Changzhou science and technology association in 2020; Jiangsu maternal and child health research project (F202052); and the open project of biological resources sample bank of major diseases in Jiangsu province in 2020 (SBK202007002); and Top Talent of Changzhou “The 14th Five-Year Plan” High-Level Health Talents Training Project (2022CZBJ084).
Author information
Authors and Affiliations
Contributions
Lingmin Hu and Lijing Bai were responsible for the conception and design of the study as well as the acquisition of data and drafting the article. Rui Qin and Xiaoyu Wang were responsible for the interpretation of data. Jing Zhou was involved in revising the article critically for important intellectual content. Chunmei Yu and Yang Chen were responsible for giving final approval of the version to be submitted. Shuxian Wang and Shenyu Zhao took responsibility for ensuring accountability for all aspects of the work, including agreement to be accountable for questions related to accuracy and integrity of any part of the work, ensuring that any related concerns were appropriately investigated and resolved. Li Chen and Renjie Lu were responsible for maintaining the integrity of the work.
Corresponding authors
Ethics declarations
Conflict of Interest
Lingmin Hu, Lijing Bai, Rui Qin, Xiaoyu Wang, Jing Zhou, Chunmei Yu, Yang Chen, Shuxian Wang, Shenyu Zhao, Li Chen and Renjie Lu have nothing to disclose.
Ethical Approval
This study was conducted in accordance with the principles outlined in the Helsinki Declaration of 1964 and its later amendments. Ethical approval for this study was obtained from the Institutional Review Board of Changzhou Maternity and Child Health Hospital. All participants provided informed consent to participate in this study.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Hu, L., Bai, L., Qin, R. et al. Optimizing FSH Concentration Modulation in the Short-Acting GnRH-a Long Protocol for IVF/ICSI: A Retrospective Study. Adv Ther 41, 215–230 (2024). https://doi.org/10.1007/s12325-023-02702-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12325-023-02702-y