Abstract
Introduction
Polycystic ovary syndrome (PCOS) is a common endocrine-metabolic disorder and the main cause of infertility in women of reproductive age. Affected women suffer from insulin resistance and present with an intense stress response. Treatment with insulin sensitizers alone and in combination is used to ameliorate the signs and symptoms associated with the disease. This study was designed to compare the endocrine and metabolic parameters as well as subjective and objective measures of stress in women with PCOS before and after treatment with acetyl-l-carnitine (ALC) and metformin plus pioglitazone.
Methods
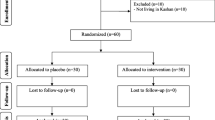
A total of 147 women with PCOS were randomly assigned into two groups: the combo group (n = 72) received a combination of metformin, pioglitazone, and ALC (500 mg, 15 mg, and 1500 mg, respectively), twice daily; the Met + Pio group (n = 75) received metformin plus pioglitazone (500 mg, 15 mg, respectively) and placebo (citric acid plus calcium carbonate), twice daily for 12 weeks. Medications were discontinued when pregnancy was confirmed. The Perceived Stress Scale (PSS14) and Profile of Mood States (POMS) were employed as subjective measures of stress. The endocrine and metabolic functions of women with PCOS were assessed by measuring insulin, leutinizing hormone (LH), follicle-stimulating hormone (FSH), testosterone, and adiponectin levels in fasting blood samples. Insulin resistance was calculated by Homeostatic Model Assessment of Insulin Resistance (HOMA-IR).
Results
Women at baseline had significantly elevated circulating concentration of insulin and low level of adiponectin. Treatment decreased insulin in both groups; however, the combo group showed a significant decrease (p = 0.001). Serum adiponectin level was raised significantly after treatment in both groups (p < 0.001). HOMA-IR also decreased in both groups (both p < 0.001). Testosterone, FSH, and LH significantly improved in both groups. LH also decreased in both groups; however, the change was significant only in the combo (metformin plus pioglitazone plus ALC) group (p = 0.013). Interestingly, there was a significant improvement in body circumference (p < 0.001) in the combo group. The PSS scores of the patients improved significantly (p < 0.001) in the combo group. Interestingly, regular menstrual cycles were found (97.2%) in the carnitine group, but in only 12.9% of the other group.
Conclusion
We conclude that addition of ALC therapy is superior to metformin plus pioglitazone in ameliorating insulin resistance, polycystic ovaries, menstrual irregularities, and hypoadiponectinemia in women with PCOS.
Trial Registration
Trial registration: clinicalTrial.gov NCT04113889. Registered 3 October, 2019. https://clinicaltrials.gov/ct2/show/NCT04113889.




Similar content being viewed by others
References
Teede HJ, Misso ML, Costello MF, et al. Recommendations from the international evidence-based guideline for the assessment and management of polycystic ovary syndrome. Hum Reprod. 2018;33(9):1602–18.
Khomami MB, Tehrani FR, Hashemi S, Farahmand M, Azizi F. Of PCOS symptoms, hirsutism has the most significant impact on the quality of life of Iranian women. PLoS One. 2015;10(4):e0123608.
Teede H, Deeks A, Moran L. Polycystic ovary syndrome: a complex condition with psychological, reproductive and metabolic manifestations that impacts on health across the lifespan. BMC Med. 2010;8(1):41.
Barry JA, Kuczmierczyk AR, Hardiman PJ. Anxiety and depression in polycystic ovary syndrome: a systematic review and meta-analysis. Hum Reprod. 2011;26(9):2442–51.
Veltman-Verhulst SM, Boivin J, Eijkemans MJ, Fauser BJ. Emotional distress is a common risk in women with polycystic ovary syndrome: a systematic review and meta-analysis of 28 studies. Hum Reprod Update. 2012;18(6):638–51.
Damone AL, Joham AE, Loxton D, Earnest A, Teede HJ, Moran LJ. Depression, anxiety and perceived stress in women with and without PCOS: a community-based study. Psychol Med. 2019;49(9):1510–20.
Escobar-Morreale HF, Villuendas G, Botella-Carretero JI, et al. Adiponectin and resistin in PCOS: a clinical, biochemical and molecular genetic study. Hum Reprod. 2006;21(9):2257–65.
Glintborg D, Andersen M, Hagen C, et al. Evaluation of metabolic risk markers in polycystic ovary syndrome (PCOS). Adiponectin, ghrelin, leptin and body composition in hirsute PCOS patients and controls. Eur J Endocrinol. 2006;155(2):337–45.
Spranger J, Möhlig M, Wegewitz U, et al. Adiponectin is independently associated with insulin sensitivity in women with polycystic ovary syndrome. Clin Endocrinol (Oxf). 2004;61(6):738–46.
Cusi K, Defronzo RA. Metformin: a review of its metabolic effects. Diabetes Rev. 1998;6(2):89–131.
Gillies PS, Dunn CJ. Pioglitazone. Drugs. 2000;60(2):333–43.
Binienda Z, Virmani A. The mitochondriotropic effects of L-carnitine and its esters in the central nervous system. Curr Med Chem-Cent Nerv Syst Agents. 2003;3(4):275–82.
Liu J, Head E, Kuratsune H, Cotman CW, Ames BN. Comparison of the effects of L-carnitine and acetyl-L-carnitine on carnitine levels, ambulatory activity, and oxidative stress biomarkers in the brain of old rats. Ann NY Acad Sci. 2004;1033(1):117–31.
Longo N, Frigeni M, Pasquali M. Carnitine transport and fatty acid oxidation. Biochim Biophys Acta. 2016;1863(10):2422–35.
Ibrahim NAM, Mansour YSE, Sulieman A, Hussein HS. A local study on the effects of L-carnitine supplement on serum lipid profiles in Libyan type 2 diabetic patients. IJARW. 2020;1:28–32.
Odo S, Tanabe K, Yohda M, Yamauchi M. Liver-oriented acute metabolic effects of a low dose of l-carnitine under fat-mobilizing conditions: pilot human clinical trial. J Nutr Sci Vitaminol (Tokyo). 2020;66(2):136–49.
Abd-Elfattah AT, Elomda FAE-A, Hashish MA-E, Megahed HI. Effect of adding L-carnitine to clomiphene resistant PCOs women on the ovulation and the pregnancy rate. Egypt J Hosp Med. 2019;76(5):4138–43.
Bruls YM, de Ligt M, Lindeboom L, et al. Carnitine supplementation improves metabolic flexibility and skeletal muscle acetylcarnitine formation in volunteers with impaired glucose tolerance: a randomised controlled trial. EBioMedicine. 2019;49:318–30.
Kousta E, White DM, Cela E, McCarthy MI, Franks S. The prevalence of polycystic ovaries in women with infertility. Hum Reprod. 1999;14(11):2720–3.
Jamilian H, Jamilian M, Samimi M, et al. Oral carnitine supplementation influences mental health parameters and biomarkers of oxidative stress in women with polycystic ovary syndrome: a randomized, double-blind, placebo-controlled trial. Gynecol Endocrinol. 2017;33(6):442–7.
Ishii T, Shimpo Y, Matsuoka Y, Kinoshita K. Anti-apoptotic effect of acetyl-L-carnitine and L-carnitine in primary cultured neurons. Jpn J Pharmacol. 2000;83(2):119–24.
Abolfathi M, Mohd-Yusof B-N, Hanipah ZN, Redzwan SM, Yusof LM, Khosroshahi MZ. The effects of carnitine supplementation on clinical characteristics of patients with non-alcoholic fatty liver disease: a systematic review and meta-analysis of randomized controlled trials. Complement Ther Med. 2020;48:102273.
Steiber A, Kerner J, Hoppel CL. Carnitine: a nutritional, biosynthetic, and functional perspective. Mol Aspects Med. 2004;25(5–6):455–73.
Fenkci SM, Fenkci V, Oztekin O, Rota S, Karagenc N. Serum total L-carnitine levels in non-obese women with polycystic ovary syndrome. Hum Reprod. 2008;23(7):1602–6.
Krsmanović LZ, Virmani MA, Stojilković SS, Catt KJ. Actions of acetyl-L-carnitine on the hypothalamo-pituitary-gonadal system in female rats. J Steroid Biochem Mol Biol. 1992;43(4):351–8.
Genazzani A, Lanzoni C, Ricchieri F, et al. Acetyl-L-carnitine (ALC) administration positively affects reproductive axis in hypogonadotropic women with functional hypothalamic amenorrhea. J Endocrinol Invest. 2011;34(4):287–91.
Reader KL, Cox NR, Stanton J-AL, Juengel JL. Effects of acetyl-L-carnitine on lamb oocyte blastocyst rate, ultrastructure, and mitochondrial DNA copy number. Theriogenology. 2015;83(9):1484–92.
Dumesic DA, Abbott DH. Implications of polycystic ovary syndrome (PCOS) on oocyte development. Semin Reprod Med. 2008;26(1):53–61.
Truong T, Gardner D. Antioxidants improve IVF outcome and subsequent embryo development in the mouse. Hum Reprod. 2017;32(12):2404–13.
Di Emidio G, Rea F, Placidi M, et al. Regulatory functions of L-carnitine, acetyl, and propionyl L-carnitine in a PCOS mouse model: focus on antioxidant/antiglycative molecular pathways in the ovarian microenvironment. Antioxidants. 2020;9(9):867.
Ismail AM, Hamed AH, Saso S, Thabet HH. Adding L-carnitine to clomiphene resistant PCOS women improves the quality of ovulation and the pregnancy rate. A randomized clinical trial. Eur J Obstet Gynecol Reprod Biol. 2014;180:148–52.
Várnagy Á, Bene J, Sulyok E, Kovács GL, Bódis J, Melegh B. Acylcarnitine esters profiling of serum and follicular fluid in patients undergoing in vitro fertilization. Reprod Biol Endocrinol. 2013;11(1):1–9.
Edris Y, Barakat E. Supplementation with L-carnitine improves uterine receptivity in women with prior implantation failure during frozen embryos transfer: A double-blinded, randomized, placebo-controlled clinical trial. Evid Based Women’s Health J. 2018;8(3):236–44.
Dunning KR, Robker RL. Promoting lipid utilization with l-carnitine to improve oocyte quality. Anim Reprod Sci. 2012;134(1–2):69–75.
El Sharkwy I, Sharaf E-D. l-Carnitine plus metformin in clomiphene-resistant obese PCOS women, reproductive and metabolic effects: a randomized clinical trial. Gynecol Endocrinol. 2019;35(8):701–5.
Samimi M, Jamilian M, Ebrahimi FA, Rahimi M, Tajbakhsh B, Asemi Z. Oral carnitine supplementation reduces body weight and insulin resistance in women with polycystic ovary syndrome: a randomized, double-blind, placebo-controlled trial. Clin Endocrinol (Oxf). 2016;84(6):851–7.
Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24(4):385–96.
Grove JR, Prapavessis H. Preliminary evidence for the reliability and validity of an abbreviated profile of mood states. Int J Sport Psychol. 1992;23(2):93–109.
Morfeld M, Petersen C, Krüger-Bödeker A, Von Mackensen S, Bullinger M. The assessment of mood at workplace-psychometric analyses of the revised Profile of Mood States (POMS) questionnaire. GMS Psycho-Social Med. 2007;4:Doc06.
Zahra M, Shah M, Ali A, Rahim R. Effects of metformin on endocrine and metabolic parameters in patients with polycystic ovary syndrome. Horm Metab Res. 2017;49(2):103–8.
Shah M, Ali A, Malik MO, et al. Treatment with metformin and combination of metformin plus pioglitazone on serum levels of IL-6 and IL-8 in polycystic ovary syndrome: a randomized clinical trial. Horm Metab Res. 2019;51(11):714–22.
El Sharkwy IA, El Aziz AWM. Randomized controlled trial of N-acetylcysteine versus l-carnitine among women with clomiphene-citrate-resistant polycystic ovary syndrome. Int J Gynecol Obstet. 2019;147(1):59–64.
Rahbar A, Shakerhosseini R, Saadat N, Taleban F, Pordal A, Gollestan B. Effect of L-carnitine on plasma glycemic and lipidemic profile in patients with type II diabetes mellitus. Eur J Clin Nutr. 2005;59(4):592–6.
Cooney LG, Lee I, Sammel MD, Dokras A. High prevalence of moderate and severe depressive and anxiety symptoms in polycystic ovary syndrome: a systematic review and meta-analysis. Hum Reprod. 2017;32(5):1075–91.
Annagür BB, Kerimoglu ÖS, Tazegül A, Gündüz Ş, Gençoglu BB. Psychiatric comorbidity in women with polycystic ovary syndrome. J Obstet Gynaecol Res. 2015;41(8):1229–33.
Hart R. PCOS and infertility. Panminerva Med. 2008;50(4):305–14.
Tsai Y-H, Wang T-W, Wei H-J, et al. Dietary intake, glucose metabolism and sex hormones in women with polycystic ovary syndrome (PCOS) compared with women with non-PCOS-related infertility. Br J Nutr. 2013;109(12):2190–8.
Talbott EO, Zborowski JV, Rager JR, Kip KE, Xu X, Orchard TJ. Polycystic ovarian syndrome (PCOS): a significant contributor to the overall burden of type 2 diabetes in women. J Womens Health. 2007;16(2):191–7.
Vrbikova J, Hainer V. Obesity and polycystic ovary syndrome. Obes Facts. 2009;2(1):26–35.
Ruggenenti P, Cattaneo D, Loriga G, et al. Ameliorating hypertension and insulin resistance in subjects at increased cardiovascular risk: effects of acetyl-L-carnitine therapy. Hypertension. 2009;54(3):567–74.
Mingorance C, del Pozo MG, Herrera MD, de Sotomayor MA. Oral supplementation of propionyl-l-carnitine reduces body weight and hyperinsulinaemia in obese Zucker rats. Br J Nutr. 2009;102(8):1145–53.
Bloomer RJ, Fisher-Wellman KH, Tucker PS. Effect of oral acetyl L-carnitine arginate on resting and postprandial blood biomarkers in pre-diabetics. Nutr Metab. 2009;6(1):25.
Giancaterini A, De Gaetano A, Mingrone G, et al. Acetyl-L-carnitine infusion increases glucose disposal in type 2 diabetic patients. Metabolism. 2000;49(6):704–8.
Center S, Harte J, Watrous D, et al. The clinical and metabolic effects of rapid weight loss in obese pet cats and the influence of supplemental oral L-carnitine. J Vet Intern Med. 2000;14(6):598–608.
Panidis D, Kourtis A, Farmakiotis D, Mouslech T, Rousso D, Koliakos G. Serum adiponectin levels in women with polycystic ovary syndrome. Hum Reprod. 2003;18(9):1790–6.
Tsao T-S, Lodish HF, Fruebis J. ACRP30, a new hormone controlling fat and glucose metabolism. Eur J Pharmacol. 2002;440(2–3):213–21.
Berg AH, Combs TP, Scherer PE. ACRP30/adiponectin: an adipokine regulating glucose and lipid metabolism. Trends Endocrinol Metab. 2002;13(2):84–9.
Pangaribuan B, Yusuf I, Mansyur M, Wijaya A. Serum adiponectin and resistin in relation to insulin resistance and markers of hyperandrogenism in lean and obese women with polycystic ovary syndrome. Ther Adv Endocrinol Metab. 2011;2(6):235–45.
Tschritter O, Fritsche A, Thamer C, et al. Plasma adiponectin concentrations predict insulin sensitivity of both glucose and lipid metabolism. Diabetes. 2003;52(2):239–43.
Acknowledgements
We thank the study subjects for participating in this clinical trial.
Funding
No funding or sponsorship was received for this study or publication of this article.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Author’s Contributions
Saman Tauqir and Momina Israr were involved in the execution of project. Bushra Rauf co-supervised the study and provided clinical expertise. Syed Hamid Habib and Fawad Ali Shah helped in editing and provided critical comments. Muhammad Omar Malik helped in organization of data and did the statistical analysis. Muhammad Usman and Muhammad Asif Raza helped in packaging of drug and masking. Inayat Shah, Haroon Badshah, and Ehtesham Ehtesham provided critical discussion in the manuscript. Mohsin Shah supervised, designed, executed the study and wrote the manuscript.
Disclosures
The authors Saman Tauqir, Momina Israr, Bushra Rauf, Muhammad Omar Malik, Syed Hamid Habib, Fawad Ali Shah, Muhammad Usman, Muhammad Asif Raza, Inayat Shah, Haroon Badshah, Ehtesham Ehtesham, and Mohsin Shah have nothing to disclose. The authors alone are responsible for the content and writing of the paper. Metformin plus pioglitazone medications (which come under the trade name of Zolid Plus) were bought from Getz Pharmaceuticals. Acetyl-l-carnitine (ALC) was purchased by Hengtai chemical Co. Ltd (Batch#10,100,420,190,605) and packed by Zenta Pharmaceutical Company. Placebo was prepared and packed in identical packaging to ALC by Zenta Pharmaceutical Company. The pharmaceutical company had no other role in the current study.
Compliance with Ethics Guidelines
All procedures involving human participants performed in this study were in accordance with the ethical standards of Khyber Medical University’s ethics committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The study was approved by the institution board of study and informed consent was obtained from each participants included in the study.
Data Availability
Available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Tauqir, S., Israr, M., Rauf, B. et al. Acetyl-l-Carnitine Ameliorates Metabolic and Endocrine Alterations in Women with PCOS: A Double-Blind Randomized Clinical Trial. Adv Ther 38, 3842–3856 (2021). https://doi.org/10.1007/s12325-021-01789-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12325-021-01789-5