Abstract
Introduction
Although cardiac resynchronization therapy (CRT) has the potential to improve cardiac function in patients with heart failure (HF), a considerable portion of patients do not respond to therapy. This study assessed the economic burden among patients with and without HF worsening after receiving CRT in real-world practice.
Methods
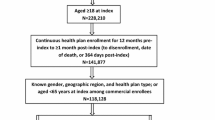
In this retrospective claims-based study using Optum’s de-identified Clinformatics® Data Mart Database (January 2007–December 2018), adults who received CRT were stratified into two cohorts based on whether they showed evidence of HF worsening within 180 days post-CRT implantation. Inverse probability of treatment weighting (IPTW) was used to adjust for confounding, accounting for demographics (e.g., age, sex), the Quan–Charlson Comorbidity Index, other clinical characteristics, healthcare resource utilization (HRU), and healthcare costs during the 180 days pre-CRT (baseline period). Annualized all-cause and congestive HF-related HRU and healthcare costs from payer and patient perspectives were assessed from day 181 post-CRT (follow-up period), and compared between cohorts using incidence rate ratios (IRRs) and cost ratios (CRs).
Results
This study included 12,753 patients (n = 4785 with HF worsening; n = 7968 without). Mean age was 72 years and roughly two-thirds were male. Baseline characteristics were balanced between cohorts post-IPTW. During follow-up, patients with HF worsening had significantly greater annual all-cause inpatient [adjusted IRR (95% confidence interval) = 1.55 (1.44, 1.66), p < 0.001], outpatient [adjusted IRR = 1.46 (1.32, 1.61), p < 0.001], and emergency department [adjusted IRR = 1.31 (1.22, 1.41), p < 0.001] visits. Mean annual total per patient payer-paid amounts were significantly higher for patients with HF worsening versus without HF worsening [adjusted CR = 1.68 (1.56, 1.80), p < 0.001]. Annual patient-paid medical costs were also higher for patients with HF worsening [adjusted CR = 1.31 (1.25, 1.38), p < 0.001]. Results were similar for congestive HF-related HRU and costs.
Conclusions
The incremental economic burden among patients with HF worsening following CRT is substantial. Efforts aimed at CRT optimization may help reduce this burden.




Similar content being viewed by others
References
Savarese G, Lund LH. Global public health burden of heart failure. Card Fail Rev. 2017;3(1):7–11.
Benjamin EJ, Muntner P, Alonso A, Bittencourt MS, Callaway CW, Carson AP, et al. Heart disease and stroke statistics-2019 update: a report from the American Heart Association. Circulation. 2019;139(10):e56–528.
King M, Kingery J, Casey B. Diagnosis and evaluation of heart failure. Am Fam Physician. 2012;85(12):1161–8.
Heidenreich PA, Albert NM, Allen LA, Bluemke DA, Butler J, Fonarow GC, et al. Forecasting the impact of heart failure in the United States: a policy statement from the American Heart Association. Circ Heart Fail. 2013;6(3):606–19.
Jackson S, Tong X, King R, Loustalot F, Hong Y, Ritchey M. National burden of heart failure events in the United States, 2006 to 2014. Circ Heart Fail. 2018;11(12):e004873.
Gedela M, Khan M, Jonsson O. Heart failure. SD Med. 2015;68(9):403–5 ((7-9)).
Shah KS, Xu H, Matsouaka RA, Bhatt DL, Heidenreich PA, Hernandez AF, et al. Heart failure with preserved, borderline, and reduced ejection fraction: 5-year outcomes. J Am Coll Cardiol. 2017;70(20):2476–86.
McAloon C, Theodoreson M, Hayat S, Osman F. Cardiac resynchronization therapy and its role in the management of heart failure. Br J Hosp Med (Lond). 2017;78(6):312–9.
Katbeh A, Van Camp G, Barbato E, Galderisi M, Trimarco B, Bartunek J, et al. Cardiac resynchronization therapy optimization: a comprehensive approach. Cardiology. 2019;142(2):116–28.
van der Meer P, Gaggin HK, Dec GW. ACC/AHA versus ESC guidelines on heart failure: JACC guideline comparison. J Am Coll Cardiol. 2019;73(21):2756–68.
Rossi A, Rossi G, Piacenti M, Startari U, Panchetti L, Morales MA. The current role of cardiac resynchronization therapy in reducing mortality and hospitalization in heart failure patients: a meta-analysis from clinical trials. Heart Vessels. 2008;23(4):217–23.
Cooper LB, DeVore AD, Michael FG. The impact of worsening heart failure in the United States. Heart Fail Clin. 2015;11(4):603–14.
DeVore AD, Hammill Bradley G, Sharma Puza P, Qualls Laura G, Mentz Robert J, Waltman Johnson K, et al. In-hospital worsening heart failure and associations with mortality, readmission, and healthcare utilization. J Am Heart Assoc. 2014;3(4):e001088.
Guidance regarding methods for de-identification of protected health information in accordance with the Health Insurance Portability and Accountability Act (HIPAA) privacy rule. 2012.
Chung ES, Leon AR, Tavazzi L, Sun J-P, Nihoyannopoulos P, Merlino J, et al. Results of the Predictors of Response to CRT (PROSPECT) Trial. Circulation. 2008;117(20):2608–16.
Stevenson WG, Hernandez AF, Carson PE, Fang JC, Katz SD, Spertus JA, et al. Indications for cardiac resynchronization therapy: 2011 update from the Heart Failure Society of America Guideline Committee. J Card Fail. 2012;18(2):94–106.
Lellouche N, De Diego C, Vaseghi M, Buch E, Cesario DA, Mahajan A, et al. Cardiac resynchronization therapy response is associated with shorter duration of atrial fibrillation. Pacing Clin Electrophysiol. 2007;30(11):1363–8.
Powell AC, Rogstad TL, Deshmukh UU, Price SE, Simmons JD. An exploration of the association between ischemic etiology and the likelihood of heart failure hospitalization following cardiac resynchronization therapy. Clin Cardiol. 2017;40(11):1090–4.
Austin PC, Stuart EA. Moving towards best practice when using inverse probability of treatment weighting (IPTW) using the propensity score to estimate causal treatment effects in observational studies. Stat Med. 2015;34(28):3661–79.
Corbisiero R, Buck DC, Muller D, Bharmi R, Dalal N, Kazemian P. What is the cost of non-response to cardiac resynchronization therapy? Hospitalizations and healthcare utilization in the CRT-D population. J Interv Card Electrophysiol. 2016;47(2):189–95.
Lunati M, Magenta G, Cattafi G, Moreo A, Falaschi G, Contardi D, et al. Clinical relevance of systematic CRT device optimization. J Atr Fibrillation. 2014;7(2):1077.
Daubert C, Behar N, Martins RP, Mabo P, Leclercq C. Avoiding non-responders to cardiac resynchronization therapy: a practical guide. Eur Heart J. 2017;38(19):1463–72.
Forleo GB, Santini L, Calò L, Ricciardi D, Curnis A, Pignalberi C, et al. Clinical and economic impact of multipoint left ventricular pacing: A comparative analysis from the Italian registry on multipoint pacing in cardiac resynchronization therapy (IRON-MPP). J Cardiovasc Electrophysiol. 2020;31(5):1166–74.
Mullens W, Grimm RA, Verga T, Dresing T, Starling RC, Wilkoff BL, et al. Insights from a cardiac resynchronization optimization clinic as part of a heart failure disease management program. J Am Coll Cardiol. 2009;53(9):765–73.
Krum H, Lemke B, Birnie D, Lee KL, Aonuma K, Starling RC, et al. A novel algorithm for individualized cardiac resynchronization therapy: rationale and design of the adaptive cardiac resynchronization therapy trial. Am Heart J. 2012;163(5):747-52e1.
Daoud GE, Houmsse M. Cardiac resynchronization therapy pacemaker: critical appraisal of the adaptive CRT-P device. Med Devices (Auckl). 2016;9:19–25.
Martin DO, Lemke B, Birnie D, Krum H, Lee KL, Aonuma K, et al. Investigation of a novel algorithm for synchronized left-ventricular pacing and ambulatory optimization of cardiac resynchronization therapy: results of the adaptive CRT trial. Heart Rhythm. 2012;9(11):1807–14.
Hsu JC, Birnie D, Stadler RW, Cerkvenik J, Feld GK, Birgersdotter-Green U. Adaptive cardiac resynchronization therapy is associated with decreased risk of incident atrial fibrillation compared to standard biventricular pacing: a real-world analysis of 37,450 patients followed by remote monitoring. Heart Rhythm. 2019;16(7):983–9.
Birnie D, Lemke B, Aonuma K, Krum H, Lee KL, Gasparini M, et al. Clinical outcomes with synchronized left ventricular pacing: analysis of the adaptive CRT trial. Heart Rhythm. 2013;10(9):1368–74.
Starling RC, Krum H, Bril S, Tsintzos SI, Rogers T, Hudnall JH, et al. Impact of a novel adaptive optimization algorithm on 30-Day readmissions: evidence from the adaptive CRT trial. JACC Heart Fail. 2015;3(7):565–72.
Hernandez-Madrid A, Lu X, Tsintzos SI, Fagan DH, Klepfer RN, Matia R, et al. Heart failure hospitalization reduction and cost savings achieved by improved delivery of effective biventricular pacing: economic implications of the OLE study under the US setting. Clinicoecon Outcomes Res. 2019;11:385–93.
Dauw J, Martens P, Mullens W. CRT optimization: what is new? What is necessary? Curr Treat Options Cardiovasc Med. 2019;21(9):45.
Fornwalt BK, Sprague WW, BeDell P, Suever JD, Gerritse B, Merlino JD, et al. Agreement is poor among current criteria used to define response to cardiac resynchronization therapy. Circulation. 2010;121(18):1985–91.
Zhu H, Zou T, Zhong Y, Yang C, Ren Y, Wang F. Prevention of non-response to cardiac resynchronization therapy: points to remember. Heart Fail Rev. 2020;25(2):269–75.
Packer M. Proposal for a new clinical end point to evaluate the efficacy of drugs and devices in the treatment of chronic heart failure. J Card Fail. 2001;7(2):176–82.
Quan H, Li B, Couris CM, Fushimi K, Graham P, Hider P, Januel J, Sundararajan V. Updating and validating the charlson comorbidity index and score for risk adjustment in hospital discharge abstracts using data from 6 countries. Am J Epidemiol. 2011;173(6):676–82.
Acknowledgements
Funding
Sponsorship for this study and the Rapid Service Fee were funded by Medtronic.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Medical Writing, Editorial, and Other Assistance
Editorial assistance in the preparation of this article was provided by Gloria DeWalt, PhD, an employee of Analysis Group, support for this assistance was funded by Medtronic.
Disclosures
Eugene S. Chung receives consulting honoraria from Medtronic, Abbott, EBR Systems. John Rickard has received consulting fees from Medtronic as well as speaking fees and research funding from Abbott. Xiaoxiao Lu is an employee of Medtronic. Maral DerSarkissian, Miriam L. Zichlin, Hoi Ching Cheung, Natalia Swartz, and Alexandra Greatsinger are employees of Analysis Group, which received research funding for the conduct of this study.
Prior Presentation
Preliminary findings from this study were presented at the Heart Rhythm Society 2020 virtual congress.
Compliance with Ethics Guidelines
Data in the CDM are statistically de-identified under the Expert Determination method, comply with the Health Insurance Portability and Accountability Act, and are managed according to Optum customer data use agreements [14]. The study and use of the data did not require approval or oversight from an institutional review board. The approval to access the data was granted via a licensing agreement with Optum.
Data Availability
The datasets generated and/or analyzed during the current study are not publically available due to licensing agreement with Optum Clinformatics© Data Mart Database.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Chung, E.S., Rickard, J., Lu, X. et al. Real-World Economic Burden Among Patients With And Without Heart Failure Worsening After Cardiac Resynchronization Therapy. Adv Ther 38, 441–467 (2021). https://doi.org/10.1007/s12325-020-01536-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12325-020-01536-2