Abstract
Introduction
Chronic pain remains an important public health problem as it continues to increase healthcare-related cost. Comorbidities like obesity have been associated with efficacy of spinal cord stimulator (SCS) therapy and worse outcomes. The goal of this study is to investigate the trends of obesity amongst hospitalized patients with SCS therapy as well as healthcare utilization outcomes.
Methods
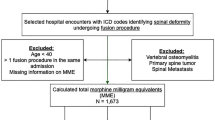
Using the International Classification of Diseases (ICD) ninth and tenth procedure and diagnosis code, we investigated the National Inpatient Sample (NIS) for patients with SCS implants between 2011 and 2015. Patients received a diagnosis of obesity based on the following categories: class I, II and III obesity. Age, gender, and comorbid conditions of patients with obesity were matched 1:1 on propensity score to those without obesity diagnosis. Our primary outcome was defined as trend of obesity diagnosis. Our secondary outcome, healthcare utilization, included in-hospital cost, length of stay, and discharge location.
Results
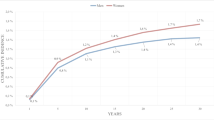
Between 2011 and 2015, a total of 3893 patients with SCS implants were identified (average age 56 ± 15 years, 58% female, 0.70 ± 1.1 Charlson Comorbidity Index, CCI). Of this cohort, 640 patients were identified as obese. The proportion of patients with obesity diagnosis increased significantly from 13.75% in 2011 to 19.36% in 2015 (p < 0.001). After 1:1 matching on propensity score, 597 patients with obesity were successfully matched to 597 patients without obesity. The total hospital cost for SCS patients with obesity (median $104,845, IQR $74,648–144,292) was not significantly different from patients without obesity diagnosis (median $111,092, IQR $68,990–145,459) (p = 0.161).
Conclusions
The data from our study suggests that there is an increasing rate of obesity diagnosis amongst patients with SCS therapy. However, there was no difference in healthcare utilization between patients with and without obesity. Additional studies may provide more insight into our findings.
Graphic Abstract


Similar content being viewed by others
References
Verrills P, Sinclair C, Barnard A. A review of spinal cord stimulation systems for chronic pain. J Pain Res. 2016;9:481–92. https://doi.org/10.2147/JPR.S108884.
Jeon YH. Spinal cord stimulation in pain management: a review. Korean J Pain. 2012;25(3):143–50. https://doi.org/10.3344/kjp.2012.25.3.143.
Chandwani HS. The economic burden of chronic back pain in the United States: a societal perspective. 2013. https://repositories.lib.utexas.edu/handle/2152/23087?show=full. Accessed August 28, 2019.
Curet ME, Mason RJ. The cost of obesity for nonbariatric inpatient operative procedures in the United States: national cost estimates obese versus nonobese patients. Ann Surg. 2013;258(4):552–3. https://doi.org/10.1097/SLA.0b013e3182a500ce.
Mekhail N, Azer G, Saweris Y, Mehanny DS, Costandi S, Mao G. The impact of tobacco cigarette smoking on spinal cord stimulation effectiveness in chronic spine-related pain patients. Reg Anesth Pain Med. 2018;43(7):768–75. https://doi.org/10.1097/AAP.0000000000000870.
Mekhail N, Mehanny D, Armanyous S, Saweris Y, Costandi S. The impact of obesity on the effectiveness of spinal cord stimulation in chronic spine-related pain patients. Spine J. 2019;19(3):476–86. https://doi.org/10.1016/j.spinee.2018.08.006.
Chooi YC, Ding C, Magkos F. The epidemiology of obesity. Metabolism. 2019;92:6–10. https://doi.org/10.1016/j.metabol.2018.09.005.
Okifuji A, Hare BD. The association between chronic pain and obesity. J Pain Res. 2015;8:399–408. https://doi.org/10.2147/JPR.S55598.
Bir SC, Konar S, Maiti T, Nanda A, Guthikonda B. Neuromodulation in intractable pain management: outcomes and predictors of revisions of spinal cord stimulators. Neurosurg Focus. 2016;40(5):E4. https://doi.org/10.3171/2016.3.FOCUS15634.
Follett KA, Boortz-Marx RL, Drake JM, et al. Prevention and management of intrathecal drug delivery and spinal cord stimulation system infections. Vol 100, 2004. www.anesthesiology.org. Accessed August 28, 2019.
Deer TR, Stewart CD. Complications of spinal cord stimulation: identification, treatment, and prevention. Pain Med. 2008. https://doi.org/10.1111/j.1526-4637.2008.00444.x.
Sastry S, Nussear D, Gillespy A, Berger K. Technical challenges of spinal cord stimulation lead placement in morbidly obese patients. Open Anesthesiol J. 2016;10(1):8–11. https://doi.org/10.2174/1874321801610010008.
HCUP. NIS Trend Weights. https://www.hcup-us.ahrq.gov/db/nation/nis/trendwghts.jsp. Accessed August 29, 2019.
Smuck M, Kao M-CJ, Brar N, Martinez-Ith A, Choi J, Tomkins-Lane CC. Does physical activity influence the relationship between low back pain and obesity? Spine J. 2014;14(2):209–16. https://doi.org/10.1016/j.spinee.2013.11.010.
Hanley MJ, Abernethy DR, Greenblatt DJ. Effect of obesity on the pharmacokinetics of drugs in humans. Clin Pharmacokinet. 2010;49(2):71–877. https://doi.org/10.2165/11318100-000000000-00000.
HHS. Federal Policy for the Protection of Human Subjects (Common Rule | HHS.gov). https://www.hhs.gov/ohrp/regulations-and-policy/regulations/common-rule/index.html. Accessed August 29, 2019.
Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011–2012. JAMA. 2014;311(8):806–14. https://doi.org/10.1001/jama.2014.732.
Hales CM, Carroll MD, Fryar CD, Ogden CL. Prevalence of obesity among adults and youth: United States, 2015–2016 Key Findings Data from the National Health and Nutrition Examination Survey. 2017. https://www.cdc.gov/nchs/data/databriefs/db288_table.pdf#1. Accessed August 28, 2019.
Khosravizadeh O, Vatankhah S, Bastani P, Kalhor R, Alirezaei S, Doosty F. Factors affecting length of stay in teaching hospitals of a middle-income country. Electron Phys. 2016;8(10):3042–7. https://doi.org/10.19082/3042.
Marola O, Cherala R, Prusik J, et al. BMI as a predictor of spinal cord stimulation success in chronic pain patients. Neuromodulation. 2017;20(3):269–73. https://doi.org/10.1111/ner.12482.
Hauck K, Hollingsworth B. The impact of severe obesity on hospital length of stay. Med Care. 2010;48(4):335–40. https://doi.org/10.1097/MLR.0b013e3181ca3d85.
Madineni RA, Smith CM, Clark SW, et al. Effect of preoperative opioid dosage on postoperative period after thoracic spinal cord stimulator surgery. Pain Med. 2018;19(4):693–8. https://doi.org/10.1093/pm/pnx250.
de Hoogd S, Välitalo PAJ, Dahan A, et al. Influence of morbid obesity on the pharmacokinetics of morphine, morphine-3-glucuronide, and morphine-6-glucuronide. Clin Pharmacokinet. 2017;56(12):1577–87. https://doi.org/10.1007/s40262-017-0544-2.
Patanwala AE, Holmes KL, Erstad BL. Analgesic response to morphine in obese and morbidly obese patients in the emergency department. Emerg Med J. 2014;31:139–42. https://doi.org/10.1136/emermed-2012-202168.
Wakefield H, Vaughan-Sarrazin M, Cullen JJ. Influence of obesity on complications and costs after intestinal surgery. Am J Surg. 2012;204(4):434–40. https://doi.org/10.1016/j.amjsurg.2012.01.013.
Zizza C, Herring AH, Stevens J, Popkin BM. Length of hospital stays among obese individuals. Am J Public Health. 2004;94(9):1587–91. https://doi.org/10.2105/ajph.94.9.1587.
Nguyen AT, Tsai C-L, Hwang L-Y, Lai D, Markham C, Patel B. Obesity and mortality, length of stay and hospital cost among patients with sepsis: a nationwide inpatient retrospective cohort study. PLoS One. 2016;11(4):e0154599. https://doi.org/10.1371/journal.pone.0154599.
US Census Bureau. Annual estimates of the resident population for selected age groups by sex for the United States, States, Counties, and Puerto Rico Commonwealth and Municipios: April 1, 2010 to July 1, 2014. Am FactFinder. 2015. https://factfinder.census.gov/faces/tableservices/jsf/pages/productview.xhtml?src=bkmk. Accessed August 28, 2019.
Hales CM, Carroll MD, Fryar CD, Ogden CL. Prevalence of obesity among adults and youth: United States, 2015–2016 Key Findings Data from the National Health and Nutrition Examination Survey. 2015. https://www.cdc.gov/nchs/data/databriefs/db288_table.pdf#1. Accessed August 28, 2019.
Bartley EJ, Fillingim RB. Sex differences in pain: a brief review of clinical and experimental findings. Br J Anaesth. 2013;111(1):52–8. https://doi.org/10.1093/bja/aet127.
Musey PI, Linnstaedt SD, Platts-Mills TF, et al. Gender differences in acute and chronic pain in the emergency department: results of the 2014 Academic Emergency Medicine consensus conference pain section. Acad Emerg Med. 2014;21(12):1421–30. https://doi.org/10.1111/acem.12529.
Johannes CB, Le TK, Zhou X, Johnston JA, Dworkin RH. The prevalence of chronic pain in United States adults: results of an internet-based survey. J Pain. 2010;11(11):1230–9. https://doi.org/10.1016/j.jpain.2010.07.002.
Thomas E, Peat G, Harris L, Wilkie R, Croft PR. The prevalence of pain and pain interference in a general population of older adults: cross-sectional findings from the North Staffordshire Osteoarthritis Project (NorStOP). Pain. 2004;110(1–2):361–8. https://doi.org/10.1016/j.pain.2004.04.017.
KFF. Population distribution by race/ethnicity. The Henry J. Kaiser Family Foundation. 2017. https://www.kff.org/other/state-indicator/distribution-by-raceethnicity/?currentTimeframe=0&selectedRows=%7B%22states%22:%7B%22pennsylvania%22:%7B%7D%7D%7D&sortModel=%7B%22colId%22:%22Location%22,%22sort%22:%22asc%22%7D. Accessed Aug 28, 2019.
Reyes-Gibby CC, Anderson KO, Shete S, Bruera E, Yennurajalingam S. Early referral to supportive care specialists for symptom burden in lung cancer patients: a comparison of non-Hispanic whites, Hispanics, and non-Hispanic blacks. Cancer. 2012;118(3):856–63. https://doi.org/10.1002/cncr.26312.
Mosher CE, Duhamel KN, Egert J, Smith MY. Self-efficacy for coping with cancer in a multiethnic sample of breast cancer patients: associations with barriers to pain management and distress. Clin J Pain. 2010;26(3):227–34. https://doi.org/10.1097/AJP.0b013e3181bed0e3.
Bernabei R, Gambassi G, Lapane K, et al. Management of pain in elderly patients with cancer. J Am Med Assoc. 1998;279(23):1877–82. https://doi.org/10.1001/jama.279.23.1877.
Harris D, Andrews R, Elixhauser A. Racial and gender differences in use of procedures for black and white hospitalized adults. Ethn Dis. 1997;7(2):91–105.
Kamble PS, Hayden J, Collins J, et al. Association of obesity with healthcare resource utilization and costs in a commercial population. Curr Med Res Opin. 2018;34(7):1335–433. https://doi.org/10.1080/03007995.2018.1464435.
Bossola M, Giungi S, Luciani G, Tazza L. Body mass index, comorbid conditions and quality of life in hemodialysis patients. J Nephrol. 2018;22(4):508–14.
Valle-Giler EP, Sulaiman WAR. Midline minimally invasive placement of spinal cord stimulators: a technical note. Ochsner J. 2014;14(1):51–6.
Eldabe S, Buchser E, Duarte RV. Complications of spinal cord stimulation and peripheral nerve stimulation techniques: a review of the literature. Pain Med. 2016;17(2):325–36. https://doi.org/10.1093/pm/pnv025.
Kim DD, Vakharyia R, Kroll HR, Shuster A. Rates of lead migration and stimulation loss in spinal cord stimulation: a retrospective comparison of laminotomy versus percutaneous implantation. Pain Phys. 2011;14(6):513–24.
Acknowledgements
Funding
No funding or sponsorship was received for this study or publication of this article.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published. All authors critically revised the manuscript, interpreted the results, and performed a critical review of the manuscript for intellectual content.
Disclosure
Vwaire Orhurhu, Faizan Khan, Mariam Salisu Orhurhu, Emeka Agudile, Ivan Urits, Jamal Hasoon, Khurram Owais, Robert Chu, Dotun Ogunsola, Omar Viswanath, Cyrus Yazdi, Jay Karri, Samir Hirji and Jatinder Gill have nothing to disclose. Thomas Simopoulos has served as a speaker for Boston Scientific, St. Jude, and Nevro Corp.
Compliance with Ethic Guidelines
The NIS database is a de-identified database that consists of a collection of billing and diagnostic codes used by participating hospitals with the goal of quality control, population monitoring, and tracking procedures. The NIS does not require institutional review board (IRB) approval or exempt determination.
Data Availability
The dataset analyzed during the current study are available in the NIS repository by the Agency for Healthcare Research and Quality, http://www.hcup-us.ahrq.gov, or from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Corresponding author
Additional information
Digital Features
To view digital features for this article go to https://doi.org/10.6084/m9.figshare.12860522.
Rights and permissions
About this article
Cite this article
Orhurhu, V., Khan, F., Salisu Orhurhu, M. et al. Obesity Trends Amongst Hospitalized Patients with Spinal Cord Stimulator Implants. Adv Ther 37, 4614–4626 (2020). https://doi.org/10.1007/s12325-020-01487-8
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12325-020-01487-8