Abstract
Introduction
Guidelines for resuscitation recommend positive-pressure ventilation with a fixed ventilation rate as provided by an automated transport ventilator during cardiopulmonary resuscitation (CPR) with a secured airway. We investigated the influence of manual chest compressions (CC) on the accuracy of ventilator presets and the quality of CC with intermittent positive-pressure ventilation (IPPV), bilevel ventilation (BiLevel), and the novel ventilation mode chest compression synchronized ventilation (CCSV) in a simulation model.
Methods
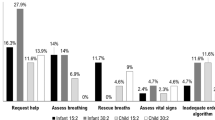
Ninety paramedics performed continuous CC for 2 min on a modified advanced life support mannequin with a realistic lung model. IPPV, BiLevel, and CCSV were applied in a randomized order. CCSV is a novel type of pressure-controlled ventilation with short insufflations synchronized with CC, which are stopped before decompression begins. The ventilator presets (tolerance range) were IPPV Vt = 450 (400–500) ml, PEEP = 0 hPa, f = 10/min; BiLevel Pinsp = 19 (17.1–20.9) hPa, PEEP = 5 hPa, f = 10/min; CCSV Pinsp = 60 (54–66) hPa, PEEP = 0 hPa, Tinsp = 205 ms, f = CC rate. Preset values were compared with the measured results. Values were defined as correct within a tolerance range. Quality of CC was evaluated using ERC guidelines (depth >50 mm, CC rate 100–120/min).
Results
Median (25th/75th percentiles) IPPV V t = 399 (386/411) ml, BiLevel Pinsp = 22.0 (19.7/25.6) hPa, and CCSV Pinsp = 55.2 (52.6/56.7) hPa. Relative frequency of delivering correct ventilation parameters according to ventilation mode: IPPV = 40 (0/100)% vs. BiLevel = 20 (0/100)%, p = 0.37 and vs. CCSV = 71 (50/83)%, p < 0.02. Pinsp was too high in BiLevel = 80 (0/100)% vs. CCSV = 0(0/0)%, p < 0.001. CC depth: IPPV 56 (48/63) mm, BiLevel 57 (48/63) mm, CCSV 60 (52/67) mm; CC rate: IPPV 117 (105/124)/min, BiLevel 116 (107/123)/min, CCSV 117 (107/125)/min.
Conclusion
When compared to IPPV and BiLevel, CCSV works best with preset values, without exceeding the upper pressure preset during simulated CPR. Quality of CC is not negatively affected by any of the ventilation patterns.
Funding
Parts of this study were supported by Weinmann Emergency Medical Technology GmbH + Co.KG.





Similar content being viewed by others
References
Huepfl M, Selig HF, Nagele P. Chest-compression-only versus standard cardiopulmonary resuscitation: a meta-analysis. Lancet. 2010;376(11):1552–7.
Deakin CD, Nolan JP, Soar J, et al. European Resuscitation Council Guidelines for Resuscitation 2010. Section 4. Adult advanced life support. Resuscitation. 2010;81:1305–52.
Chalkias A, Xanthos T. Timing positive-pressure ventilation during chest compression: the key to improving the thoracic pump? Eur Hear J Acute Cardiovasc Care. 2013;4(1):24–7.
Kill C, Hahn O, Dietz F, et al. Mechanical ventilation during cardiopulmonary resuscitation with intermittent positive-pressure ventilation, BiLevel ventilation, or chest compression Synchronized ventilation in a pig model. Crit Care Med. 2014;42(2):e89–95.
Kleinsasser A, Lindner KH, Schaefer A, Loeckinger A. Decompression-triggered positive-pressure ventilation during cardiopulmonary resuscitation improves pulmonary gas exchange and oxygen uptake. Circulation. 2002;106(3):373–8.
Theres H, Binkau J, Laule M, et al. Phase-related changes in right ventricular cardiac output under volume-controlled mechanical ventilation with positive end-expiratory pressure. Crit Care Med. 1999;27(5):953–8.
Yannopoulos D, McKnite S, Metzger A, Lurie KG. Intrathoracic pressure regulation improves 24-hour survival in a porcine model of hypovolemic shock. Anesth Analg. 2007;104(1):157–62.
Yannopoulos D, Nadkarni VM, McKnite SH, et al. Intrathoracic pressure regulator during continuous-chest-compression advanced cardiac resuscitation improves vital organ perfusion pressures in a porcine model of cardiac arrest. Circulation. 2005;112(6):803–11.
Kill C, Galbas M, Neuhaus C, et al. Chest compression synchronized ventilation versus intermittent positive pressure ventilation during cardiopulmonary resuscitation in a pig model. PLoS One. 2015;10(5):e0127759.
Kill C, Thonke R, Hahn O, et al. Cerebral oxygenation during resuscitation: influence of the ventilation modes chest compression synchronized ventilation (CCSV) or intermitted positive pressure ventilation (IPPV) and of vasopressors on cerebral tissue oxygen saturation. Resuscitation. 2015;96(11):44.
World Medical Association. World Medical Association declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA. 2013;310(20):2191–4.
Oczenski W. Atmen—Atemhilfen (in German). 9th ed. Stuttgart: Georg Thieme Verlag KG; 2012.
Ornato JP. Measurement of ventilation during cardiopulmonary resuscitation. Crit Care Med. 1983;11(2):79–82.
Davis K, Johannigman JA, Johnson RC, Branson RD. Lung compliance following cardiac arrest. Acad Emerg Med. 1995;2(10):874–8.
Lung ventilators—Part 3: Particular requirements for emergency and transport ventilators; German version EN 794-3:1998+A2:2009. https://www.beuth.de/de/norm/din-en-794-3/120991369. Accessed 24 July 2016.
WEINMANN Emergency Medical Technology GmbH + Co. KG. WEINMANN Medumat Transport—Instructor’s manual. https://www.weinmann-emergency.com/downloads/instructions_for_use/MEDUMAT_Transport/MEDUMAT_Transport_66000d_de.pdf. Accessed 14 Sept 2017.
Harnischmacher U. Clinical-Trials.De. http://www.clinical-trials.de/de/Werkzeuge/Online_Hilfsmittel/online_hilfsmittel.html. Accessed 24 July 2016.
Cohen J. Statistical power analysis for the behavioral sciences. 2nd ed. Hillsdale: Lawrence Erlbaum Associates; 1988.
Bortz J, Schuster C. Statistik für Sozial- und Humanwissenschaftler. 7th ed. Heidelberg: Springer; 2010.
Bortz J, Döring N. Forschungsmethoden und Evaluation. 4th ed. Heidelberg: Springer; 2006.
StataCorp LP. STATA—data analysis and statistical software, Version 13.1 (2013). http://www.stata.com. Accessed 14 Sept 2017.
BiAS. für Windows. Data analysis and statistical software, Version 10.04, Epsilon Verlag. http://www.bias-online.de. Accessed 14 Sept 2017.
Aufderheide TP, Lurie KG. Death by hyperventilation: a common and life-threatening problem during cardiopulmonary resuscitation. Crit Care Med. 2004;32(9):345–51.
Aufderheide TP, Sigurdsson G, Pirrallo RG, et al. Hyperventilation-induced hypotension during cardiopulmonary resuscitation. Circulation. 2004;109:1960–5.
O’Neill JF, Deakin CD. Do we hyperventilate cardiac arrest patients? Resuscitation. 2007;73:82–5.
McInnes AD, Sutton RM, Orioles A, et al. The first quantitative report of ventilation rate during in-hospital resuscitation of older children and adolescents. Resuscitation. 2011;82:1025–9.
Gazmuri RJ, Ayoub IM, Radhakrishnan J, Motl J, Upadhyaya MP. Clinically plausible hyperventilation does not exert adverse hemodynamic effects during CPR but markedly reduces end-tidal PCO2. Resuscitation. 2012;83:259–64.
Ahn HJ, Kim KD, Jeong WJ, Lee JW, Yoo IS, Ryu SR. The adequacy of a conventional mechanical ventilator as a ventilation method during cardiopulmonary resuscitation: a manikin study. Korean J Crit Care Med. 2015;30(2):89–94.
Lurie KG, Lindo C, Chin J. CPR: the P stands for plumber’s helper. JAMA. 1990;264:1661.
Ewy GA. Cardiocerebral resuscitation: the new cardiopulmonary resuscitation. Circulation. 2005;111(16):2134–42.
Chalkias A, Pavlopoulos F, Koutsovasilis A, d’Aloja E, Xanthos T. Airway pressure and outcome of out-of-hospital cardiac arrest: a prospective observational study. Resuscitation. 2016;110:101–6.
Criley JM, Blaufuss AH, Kissel GL. Cough-induced cardiac compression. JAMA. 1976;236:1246–50.
Vadeboncoeur T, Stolz U, Panchal A, et al. Chest compression depth and survival in out-of-hospital cardiac arrest. Resuscitation. 2014;85:182–8.
Hellevuo H, Sainio M, Nevalainen R, et al. Deeper chest compression—more complications for cardiac arrest patients? Resuscitation. 2013;84:760–5.
Stiell IG, Brown SP, Nichol G, et al. Resuscitation outcomes consortium I What is the optimal chest compression depth during out-of-hospital cardiac arrest resuscitation of adult patients? Circulation. 2014;130:1962–70.
Acknowledgements
The authors would like to express their gratitude to the paramedics working for the EMS of Marburg-Biedenkopf and Giessen, who have participated in this study. We also thank Thomas Ploch for his support in planning the experiment and his statistical review. Weinmann Emergency Medical Technology GmbH + Co.KG provided support in the form of a salary for author CN, but did not have any additional role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript. Article processing charges were subsidized by Weinmann Emergency Medical Technology GmbH + Co.KG. There are no patents, products in development, or marketed products to declare. All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this manuscript, take responsibility for the integrity of the work as a whole, and have given final approval for the version to be published. All authors had full access to all of the data in this study and take complete responsibility for the integrity of the data and accuracy of the data analysis.
Disclosures
T. Speer received compensation for travel from Weinmann EMT. B. Kleine received compensation for travel from Weinmann EMT. T. Speer received refunds for congress fees from Weinmann EMT. T. Speer worked as a medical consultant for Weinmann EMT. C. Kill worked as a medical consultant for Weinmann EMT. C. Neuhaus is an employee of Weinmann EMT. W. Dersch has nothing to disclose.
Compliance with Ethics Guidelines
Ethics Committee of the Medical Faculty of the Philipps University of Marburg, reference number 36/14. This article does not contain any studies collecting data from human or animal. All participants received oral and written information about the study and gave informed consent, which could be withdrawn at any time.
Data Availability
All data generated or analyzed during this study are included as supplementary information files.
Author information
Authors and Affiliations
Corresponding author
Additional information
Enhanced content
To view enhanced content for this article go to http://www.medengine.com/Redeem/A57AF0605F09C878.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Speer, T., Dersch, W., Kleine, B. et al. Mechanical Ventilation During Resuscitation: How Manual Chest Compressions Affect a Ventilator’s Function. Adv Ther 34, 2333–2344 (2017). https://doi.org/10.1007/s12325-017-0615-7
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12325-017-0615-7