Abstract
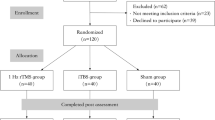
Repetitive transcranial magnetic stimulation (rTMS), a noninvasive neuroregulatory technique used to treat neurodegenerative diseases, holds promise for spinocerebellar ataxia type 3 (SCA3) treatment, although its efficacy and mechanisms remain unclear. This study aims to observe the short-term impact of cerebellar rTMS on motor function in SCA3 patients and utilize resting-state functional magnetic resonance imaging (RS-fMRI) to assess potential therapeutic mechanisms. Twenty-two SCA3 patients were randomly assigned to receive actual rTMS (AC group, n = 11, three men and eight women; age 32–55 years) or sham rTMS (SH group, n = 11, three men and eight women; age 26–58 years). Both groups underwent cerebellar rTMS or sham rTMS daily for 15 days. The primary outcome measured was the ICARS scores and parameters for regional brain activity. Compared to baseline, ICARS scores decreased more significantly in the AC group than in the SH group after the 15-day intervention. Imaging indicators revealed increased Amplitude of Low Frequency Fluctuation (ALFF) values in the posterior cerebellar lobe and cerebellar tonsil following AC stimulation. This study suggests that rTMS enhances motor functions in SCA3 patients by modulating the excitability of specific brain regions and associated pathways, reinforcing the potential clinical utility of rTMS in SCA3 treatment. The Chinese Clinical Trial Registry identifier is ChiCTR1800020133.


Similar content being viewed by others
Data Availability
The data that support the findings of this study are available from the corresponding author, upon reasonable request.
References
Dulski J, Al-Shaikh RH, Sulek A, Kasprzak J, Sławek J, Wszolek ZK. Spinocerebellar ataxia type 3 (Machado-Joseph disease). Pol Arch Intern Med 2022; 132.
Beaudin M, Manto M, Schmahmann JD, Pandolfo M, Dupre N. Recessive cerebellar and afferent ataxias - clinical challenges and future directions. Nat Rev Neurol. 2022;18:257–72.
Chien HF, Zonta MB, Chen J, et al. Rehabilitation in patients with cerebellar ataxias. Arq Neuropsiquiatr. 2022;80:306–15.
Ferrucci R, Bocci T, Cortese F, Ruggiero F, Priori A. Noninvasive Cerebellar Stimulation as a Complement Tool to Pharmacotherapy. Curr Neuropharmacol. 2019;17:14–20.
Liu Y, Ma Y, Zhang J, Yan X, Ouyang Y. Effects of Non-invasive Brain Stimulation on Hereditary Ataxia: a Systematic Review and Meta-analysis. Cerebellum 2023.
Zesiewicz TA, Wilmot G, Kuo SH, et al. Comprehensive systematic review summary: Treatment of cerebellar motor dysfunction and ataxia: Report of the Guideline Development, Dissemination, and Implementation Subcommittee of the American Academy of Neurology. Neurology. 2018;90:464–71.
Manor B, Greenstein PE, Davila-Perez P, Wakefield S, Zhou J, Pascual-Leone A. Repetitive Transcranial Magnetic Stimulation in Spinocerebellar Ataxia: A Pilot Randomized Controlled Trial. Front Neurol. 2019;10:73.
Sanna A, Follesa P, Tacconi P, et al. Therapeutic Use of Cerebellar Intermittent Theta Burst Stimulation (iTBS) in a Sardinian Family Affected by Spinocerebellar Ataxia 38 (SCA 38). Cerebellum. 2022;21:623–31.
Qiu M, Wang R, Shen Y, Hu Z, Zhang Y. Efficacy and Safety of Repetitive Transcranial Magnetic Stimulation in Spinocerebellar Ataxia Type 3: a Systematic Review and Meta‑analysis of Randomized Controlled Trials. Cerebellum 2023 .
Shi Y, Zou G, Chen Z, et al. Efficacy of cerebellar transcranial magnetic stimulation in spinocerebellar ataxia type 3: a randomized, single-blinded, controlled trial. J Neurol. 2023;270:5372–9.
Benussi A, Batsikadze G, França C, Cury RG, Maas R. The Therapeutic Potential of Non-Invasive and Invasive Cerebellar Stimulation Techniques in Hereditary Ataxias. Cells. 2023;12:1193.
Sikandar A, Liu XH, Xu HL, et al. Short-term efficacy of repetitive transcranial magnetic stimulation in SCA3: A prospective, randomized, double-blind, sham-controlled study. Parkinsonism Relat Disord. 2023;106:105236.
Chen XY, Lian YH, Liu XH, et al. Effects of Repetitive Transcranial Magnetic Stimulation on Cerebellar Metabolism in Patients With Spinocerebellar Ataxia Type 3. Front Aging Neurosci. 2022;14:827993.
Tang Z, Liu T, Han K, et al. The effects of rTMS on motor recovery after stroke: a systematic review of fMRI studies. Neurol Sci. 2023;45:897–909.
González-García N, Armony JL, Soto J, Trejo D, Alegría MA, Drucker-Colín R. Effects of rTMS on Parkinson’s disease: a longitudinal fMRI study. J Neurol. 2011;258:1268–80.
Guo J, Jiang Z, Liu X, et al. Cerebello-cerebral resting-state functional connectivity in spinocerebellar ataxia type 3. Hum Brain Mapp. 2023;44:927–36.
Trouillas P, Takayanagi T, Hallett M, et al. International Cooperative Ataxia Rating Scale for pharmacological assessment of the cerebellar syndrome. The Ataxia Neuropharmacology Committee of the World Federation of Neurology. J Neurol Sci. 1997;145:205–11.
Kiviniemi V, Kantola JH, Jauhiainen J, Tervonen O. Comparison of methods for detecting nondeterministic BOLD fluctuation in fMRI. Magn Reson Imaging. 2004;22:197–203.
Zang Y, Jiang T, Lu Y, He Y, Tian L. Regional homogeneity approach to fMRI data analysis. Neuroimage. 2004;22:394–400.
Long Z, Du L, Marino M. Individual resting-state network functional connectivity predicts treatment improvement of repetitive transcranial magnetic stimulation in major depressive disorder: A pilot study. Psychiatry Res. 2024;331:115616.
Rosso C, Moulton EJ, Kemlin C, et al. Cerebello-Motor Paired Associative Stimulation and Motor Recovery in Stroke: a Randomized, Sham-Controlled. Double-Blind Pilot Trial Neurotherapeutics. 2022;19:491–500.
Li X, Qi G, Yu C, et al. Cortical plasticity is correlated with cognitive improvement in Alzheimer’s disease patients after rTMS treatment. Brain Stimul. 2021;14:503–10.
Qin Y, Liu X, Guo X, Liu M, Li H, Xu S. Low-Frequency Repetitive Transcranial Magnetic Stimulation Restores Dynamic Functional Connectivity in Subcortical Stroke. Front Neurol. 2021;12:771034.
Shiga Y, Tsuda T, Itoyama Y, et al. Transcranial magnetic stimulation alleviates truncal ataxia in spinocerebellar degeneration. J Neurol Neurosurg Psychiatry. 2002;72:124–6.
Zhou M, Qiu M, Jin Y et al. Effectiveness of High-Frequency Repetitive Transcranial Magnetic Stimulation in Patients With Spinocerebellar Ataxia Type 3. J ECT 2023 .
Grimaldi G, Argyropoulos GP, Boehringer A, et al. Non-invasive cerebellar stimulation–a consensus paper. Cerebellum. 2014;13:121–38.
Manto M, Serrao M, Filippo Castiglia S, et al. Neurophysiology of cerebellar ataxias and gait disorders. Clin Neurophysiol Pract. 2023;8:143–6029.
Jantzen KJ, Oullier O, Marshall M, Steinberg FL, Kelso JA. A parametric fMRI investigation of context effects in sensorimotor timing and coordination. Neuropsychologia. 2007;45:673–84.
Liu WF, Shu YQ, Zhu PW, et al. The Cerebellum Posterior Lobe Associates with the Exophthalmos of Primary Hyperthyroidism: A Resting-State fMRI Study. Int J Endocrinol. 2019;2019:8135671.
Hu XF, Zhang JQ, Jiang XM, et al. Amplitude of low-frequency oscillations in Parkinson’s disease: a 2-year longitudinal resting-state functional magnetic resonance imaging study. Chin Med J (Engl). 2015;128:593–601.
Bier JC, Dethy S, Hildebrand J, et al. Effects of the oral form of ondansetron on cerebellar dysfunction A multi-center double-blind study. J Neurol. 2003;250:693–7.
Zesiewicz TA, Greenstein PE, Sullivan KL, et al. A randomized trial of varenicline (Chantix) for the treatment of spinocerebellar ataxia type 3. Neurology. 2012;78:545–50.
Acknowledgements
The authors would like to thank the kind patients, families, and caregivers who participated in this research.
Funding
This work was supported by The Joint Funds for the Innovation of Science and Technology Fujian Province to X–Y Chen (No.2021Y9088, Fujian).
Author information
Authors and Affiliations
Consortia
Contributions
XL, LZ, HLX and XYC formulated and designed the study concept; XHL, AS, MCL, XYX, ZQH, NPC, and YQT enrolled the patients and conducted clinical assessments and neuropsychological tests; JPH and QLC conducted imaging data collection; SRG, XYC, QLC and SZW analyzed the data, and interpreted the results; All authors were involved in drafting/revising the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethical Approval
This study is within the framework of a clinical trial (MRCTA, ECFAH OF [2018]201) approved by Local Institutional Review Board. Written informed consent was obtained from the patient for publication of their clinical details, imaging and video data.
Competing Interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Xia Liu, Lin Zhang and Hao-Lin Xu these authors share the first authorship of this article.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Liu, X., Zhang, L., Xu, HL. et al. Effect of Regional Brain Activity Following Repeat Transcranial Magnetic Stimulation in SCA3: A Secondary Analysis of a Randomized Clinical Trial. Cerebellum (2024). https://doi.org/10.1007/s12311-024-01689-8
Accepted:
Published:
DOI: https://doi.org/10.1007/s12311-024-01689-8